Introduction
- The male genital system is a complex and highly specialized anatomical structure responsible for reproduction, sexual function, and the production of male sex hormones.
- This system includes internal and external organs that work harmoniously to produce, store, and transport sperm while also secreting testosterone.
- This hormone is essential for the development of male characteristics and fertility.
- The primary organs of the male genital system are the testes, where sperm and testosterone are produced, and the penis, which is used for sexual intercourse and the passage of urine.
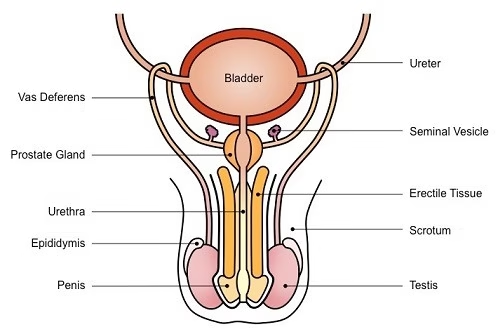
- The system also includes accessory organs such as the epididymis, vas deferens, seminal vesicles, prostate gland, and bulbourethral glands, each playing vital roles in sperm maturation, nourishment, and protection.
- Spermatogenesis, the process of sperm production, is initiated in the testes and completed in the epididymis.
- The sperm are then transported through the vas deferens and mixed with fluids from the seminal vesicles, prostate, and bulbourethral glands to form semen.
- The male genital system is regulated by intricate hormonal feedback loops, primarily involving the hypothalamus, pituitary gland, and testes.
- These hormones not only control sperm production but also govern the development of secondary sexual characteristics such as muscle mass, facial hair, and a deeper voice.
Anatomy of the Male Genital System
External Genitalia:
-
Penis:
- Structure:
- Root: The base of the penis, which is attached to the pelvic bones.
- Shaft: The elongated body of the penis, which is cylindrical and is made up of erectile tissue. The shaft contains three columns of erectile tissue: two corpora cavernosa (located on the dorsal side) and one corpus spongiosum (located ventrally around the urethra).
- Glans Penis: The rounded tip of the penis, which is highly sensitive. It is covered by the prepuce (foreskin) in uncircumcised males and is exposed when circumcised.
- Function: The penis serves two primary functions:
- Urination: The urethra runs through the penis and allows for the passage of urine from the bladder.
- Sexual Intercourse: During arousal, the erectile tissues of the penis fill with blood, causing an erection, which facilitates penetration during intercourse for reproductive purposes.
- Structure:
-
Urethra:
- The urethra is a tubular structure that runs from the bladder through the penis, opening at the glans.
- It serves a dual purpose:
- Urine Passage: Carries urine from the bladder during urination.
- Semen Passage: Carries semen from the ejaculatory ducts during ejaculation. The urethra is divided into three regions: prostatic urethra, membranous urethra, and penile urethra.
-
Scrotum:
- Structure: The scrotum is a pouch of skin and muscle that holds the testes outside the body cavity. It has a wrinkled appearance due to the dartos muscle, and also has the cremaster muscle, which can elevate or lower the testes.
- Function:
- The scrotum serves to protect the testes and maintain their temperature.
- Spermatogenesis occurs optimally at a temperature slightly lower than normal body temperature (around 34–36°C), which is why the testes are housed outside the body.
- The scrotum can adjust its position by contracting or relaxing the muscles to maintain this temperature.
Internal Genitalia:
-
Testes (Testicles):
- Structure:
- The testes are oval-shaped organs located within the scrotum. A tough, fibrous layer surrounds each testis called the tunica albuginea.
- Inside the testes are numerous coiled tubes called seminiferous tubules, where sperm are produced.
- Between the seminiferous tubules, clusters of Leydig cells produce testosterone.
- Function:
- Sperm Production (Spermatogenesis): Within the seminiferous tubules, spermatogonia (stem cells) divide and undergo meiosis to form sperm cells. This process takes about 64–72 days.
- Hormone Production: Leydig cells secrete testosterone, which is critical for the development of male secondary sexual characteristics and plays a role in sexual drive (libido) and the maintenance of spermatogenesis.
- Structure:
-
Epididymis:
- Structure: The epididymis is a long, coiled tube located on the posterior surface of each testis. It consists of three parts: the head, body, and tail.
- Function:
- Sperm Maturation: Sperm produced in the seminiferous tubules are immature and incapable of fertilizing an egg.
- The epididymis is where sperm undergo final maturation, acquiring the ability to swim and fertilize an egg.
- Sperm Storage: The epididymis also acts as a storage site for sperm until they are ejaculated.
-
Vas Deferens (Ductus Deferens):
- Structure: The vas deferens is a thick-walled tube that connects the epididymis to the ejaculatory ducts. It passes through the inguinal canal and the pelvic cavity.
- Function:
- The vas deferens transports mature sperm from the epididymis to the ejaculatory ducts in anticipation of ejaculation.
- During sexual arousal, smooth muscle contractions propel sperm through the vas deferens toward the urethra.
-
Seminal Vesicles:
- Structure: The seminal vesicles are paired glands behind the bladder and are connected to the vas deferens via the seminal duct.
- Function:
- The seminal vesicles secrete seminal fluid, which makes up the majority of semen.
- This fluid is rich in fructose, a sugar that provides energy to sperm for motility.
- The fluid also contains prostaglandins, which help sperm navigate the female reproductive tract by stimulating uterine contractions.
-
Prostate Gland:
- Structure: The prostate is a walnut-sized gland located just below the bladder, surrounding the urethra. It has a glandular structure composed of smooth muscle and glandular tissue.
- Function:
- The prostate secretes a milky, alkaline fluid that contributes to the composition of semen.
- This fluid helps neutralize the acidity of the vaginal environment, ensuring sperm survive in the female reproductive tract.
- The prostate also helps propel semen into the urethra during ejaculation through muscle contractions.
-
Bulbourethral Glands (Cowper’s Glands):
- Structure: These are two small pea-sized glands located beneath the prostate, near the base of the penis.
- Function:
- The bulbourethral glands secrete a clear, mucus-like fluid during sexual arousal.
- This fluid is a lubricant for the urethra, reducing friction during ejaculation.
- It also neutralizes any residual urine that may be acidic in the urethra.
Physiology of the Male Genital System
-
Spermatogenesis:
- Process Overview:
- Spermatogenesis is the process by which spermatozoa (sperm cells) are produced in the seminiferous tubules. It begins with spermatogonia (stem cells) that undergo mitosis to create more spermatogonia. Some of these cells enter meiosis to become primary spermatocytes.
- Meiosis: The primary spermatocytes divide to form secondary spermatocytes, which then divide again into spermatids. The spermatids mature into spermatozoa (sperm cells) through spermiogenesis.
- Maturation of Sperm: Sperm cells are immature when first formed and must undergo a maturation process in the epididymis, where they gain motility and the ability to fertilize an egg.
- Process Overview:
-
Testosterone Production:
- Leydig Cells: Located between the seminiferous tubules, these cells produce testosterone in response to luteinizing hormone (LH) from the anterior pituitary.
- Testosterone Effects: Testosterone is responsible for:
- Development of Male Sexual Characteristics: It triggers the development of secondary sexual characteristics such as facial hair, deeper voice, increased muscle mass, and broader shoulders.
- Spermatogenesis: Testosterone is crucial for the maturation of sperm cells.
- Sexual Drive (Libido): It influences sexual desire and behaviour.
-
Erection and Ejaculation:
- Erection:
- An erection is initiated by sexual arousal, which triggers the parasympathetic nervous system.
- This causes vasodilation of the blood vessels supplying the penis, leading to the filling of the corpora cavernosa and corpus spongiosum with blood.
- The increased blood flow causes the penis to become rigid.
- Ejaculation:
- Ejaculation is a reflex action controlled by the sympathetic nervous system.
- During sexual climax, rhythmic contractions of the prostate, seminal vesicles, and vas deferens push sperm into the urethra, which is then expelled through the penis during ejaculation. This process is called emission.
- Erection:
-
Regulation of the Male Genital System:
- Hypothalamic-Pituitary-Gonadal Axis:
- The production of sperm and testosterone is regulated by the hypothalamus, which releases gonadotropin-releasing hormone (GnRH). GnRH stimulates the anterior pituitary to release LH and FSH.
- LH stimulates Leydig cells to produce testosterone, while FSH promotes spermatogenesis in the seminiferous tubules.
- Increased levels of testosterone inhibit the release of GnRH and LH, creating a negative feedback loop that maintains hormonal balance.
- Hypothalamic-Pituitary-Gonadal Axis: