Introduction
-
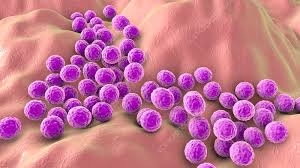
Staphylococci are Gram-positive cocci that typically appear in grape-like clusters due to division in multiple planes.
-
They are non-motile, non-spore-forming, and facultative anaerobes.
-
Staphylococci are widely present in nature and form part of the normal flora of skin, anterior nares, and mucous membranes of humans.
-
They are catalase-positive, which differentiates them from Streptococci (catalase-negative).
-
Based on coagulase production, they are divided into:
-
Coagulase-positive (e.g., Staphylococcus aureus)
-
Coagulase-negative (e.g., S. epidermidis, S. saprophyticus)
-
-
Staphylococci are highly resistant to environmental conditions, surviving drying, heat, and high salt concentrations.
-
They produce multiple virulence factors such as enzymes, toxins, and adhesion molecules, enabling colonization and invasion.
-
Clinically, they are major causes of pyogenic infections, wound infections, abscesses, and device-related infections.
-
Some strains (especially S. aureus) cause toxin-mediated diseases like food poisoning, scalded skin syndrome, and toxic shock syndrome.
-
Staphylococci are significant hospital-acquired (nosocomial) pathogens, including MRSA strains with antimicrobial resistance.
General Character
- Genus: Staphylococcus
- Family: Staphylococcaceae
- Gram Staining: Staphylococci are Gram-positive, appearing purple under a microscope due to their thick peptidoglycan layer.
- Shape and Arrangement:
- Shape: They are spherical (cocci) in shape.
- Arrangement: Staphylococci are typically found in clusters resembling grapes due to division in multiple planes without separation.
- Oxygen Requirements: Staphylococci are facultative anaerobes. This means they can grow in both the presence and absence of oxygen, allowing them to inhabit diverse environments, including human skin and mucosal surfaces.
Morphology
- Cell Wall Structure:
- Composed of a thick peptidoglycan layer (approximately 30-80% of the cell wall) provides structural integrity and helps resist osmotic pressure.
- It contains teichoic acids that play roles in cell wall maintenance and regulation of cell growth.
- Capsule:
- Some species, particularly Staphylococcus aureus, possess a polysaccharide capsule that helps evade phagocytosis by immune cells.
- Surface Structures:
- Slime Layer: Contributes to biofilm formation, particularly in coagulase-negative staphylococci (CoNS), enhancing adherence to surfaces like catheters and prosthetic devices.
- Flagella: Staphylococci are non-motile, lacking flagella and using other mechanisms for adherence and colonization.
Cultural Characteristics
- Growth Media:
- Blood Agar: Supports the growth of various staphylococcal species and allows for hemolysis observation. S. aureus shows β-hemolysis, while S. epidermidis is usually non-hemolytic.
- Mannitol Salt Agar (MSA): A selective medium for staphylococci. It contains high salt concentration (7.5% NaCl) and mannitol. S. aureus ferments mannitol, resulting in a yellow colour change, while S. epidermidis does not ferment it and remains red.
- Colony Appearance:
- Colonies of S. aureus are typically golden-yellow due to carotenoid pigments, while S. epidermidis colonies are usually white or off-white.
- Temperature and pH Range:
- The optimal growth temperature is around 37°C, but they can grow between 15°C and 45°C.
- They can tolerate a broad pH range, but neutral pH is preferred for optimal growth.
Biochemical Reactions
- Catalase Test: Staphylococci produce the enzyme catalase, which converts hydrogen peroxide into water and oxygen, resulting in bubbling. This distinguishes them from streptococci, which are catalase-negative.
- Coagulase Test:
- S. aureus: Positive for coagulase, causing plasma to clot.
- Coagulase-negative Staphylococci (CoNS), like S. epidermidis, are usually coagulase-negative.
- Mannitol Fermentation:
- S. aureus: Ferments mannitol, producing acid and causing a colour change in MSA.
- S. epidermidis: Does not ferment mannitol.
- Other Biochemical Tests:
- Oxidase Test: Negative.
- Urease Test: Variable; most strains of S. saprophyticus are urease-positive, while others are typically negative.
- DNase Test: Positive for S. aureus, indicating the ability to degrade DNA. This is a differentiating feature for identifying S. aureus.
Pathogenicity
- Virulence Factors:
- Toxins:
- Enterotoxins: Heat-stable toxins responsible for food poisoning, leading to gastrointestinal symptoms.
- Toxic Shock Syndrome Toxin (TSST-1): A superantigen that can cause toxic shock syndrome characterized by fever, rash, and multi-organ failure.
- Alpha-toxin: A pore-forming toxin that disrupts cell membranes, causing tissue damage and necrosis.
- Enzymes:
- Coagulase: Promotes clot formation, helping to shield the bacteria from immune responses.
- Hyaluronidase: Breaks down hyaluronic acid in connective tissue, facilitating tissue invasion.
- Lipase: Allows for colonization of sebaceous glands by breaking down lipids.
- Adhesins: Surface proteins that promote binding to host tissues, critical for colonization and infection.
- Toxins:
- Clinical Infections:
- Skin and Soft Tissue Infections: Commonly cause boils, abscesses, impetigo, and cellulitis.
- Invasive Infections: This can lead to more severe conditions like endocarditis (infection of the heart valves), osteomyelitis (bone infection), and septic arthritis.
- Respiratory Infections: S. aureus can cause pneumonia, especially in immunocompromised individuals or those with chronic lung disease.
- Food Poisoning: Resulting from ingestion of food contaminated with enterotoxins, leading to nausea, vomiting, and diarrhoea.
- Opportunistic Pathogen:
- S. epidermidis: Often associated with infections related to medical devices (e.g., catheters, prosthetic joints) due to biofilm formation.
- S. saprophyticus: A common cause of urinary tract infections, particularly in young women.
Laboratory Diagnosis
- Specimen Collection: Obtaining samples from infected sites (e.g., skin lesions, abscesses, blood, urine). The choice of specimen depends on the clinical presentation.
- Microscopic Examination:
- A Gram stain of the specimen reveals Gram-positive cocci in clusters.
- This initial finding guides further testing and identification.
- Culture Techniques:
- Inoculation: Samples are inoculated on blood agar and MSA to promote growth and identify species.
- Incubation: Cultures are typically incubated at 35-37°C for 24-48 hours.
- Colony Morphology Examination: Observing colony colour and morphology aids in preliminary identification.
- Biochemical Testing:
- Catalase Test: Distinguishes staphylococci from streptococci.
- Coagulase Test: Essential for differentiating S. aureus from CoNS.
- Mannitol Fermentation Test: Further identifies S. aureus based on mannitol fermentation.
- Additional tests may include the DNase and urease tests, depending on the suspected species.
- Molecular Methods:
- Polymerase chain reaction (PCR) and other nucleic acid amplification techniques can provide rapid and specific identification of staphylococci and detection of antibiotic resistance genes.
- These methods are especially useful in outbreaks or cases of severe infections.
Antibiotic Resistance
- Methicillin-resistant Staphylococcus aureus (MRSA): A significant public health concern due to its resistance to beta-lactam antibiotics. MRSA strains are often associated with severe infections and are prevalent in both hospital and community settings.
- Vancomycin-Resistant Staphylococcus aureus (VRSA): The emergence of strains resistant to vancomycin complicates treatment options.
- Coagulase-negative Staphylococci: Increasingly recognized for their resistance to multiple antibiotics, posing challenges in treating infections associated with implanted medical devices.
MCQs
1. Staphylococci appear microscopically as:
A. Gram-negative rods
B. Gram-positive cocci in chains
C. Gram-positive cocci in clusters
D. Gram-negative cocci
2. The word “staphyle” means:
A. Chain
B. Grape
C. Spiral
D. Rod
3. Staphylococci are:
A. Motile
B. Non-motile
C. Spore forming
D. Acid-fast
4. Staphylococci are:
A. Obligate anaerobes
B. Facultative anaerobes
C. Strict aerobes
D. Microaerophilic
5. Staphylococci are differentiated from Streptococci by:
A. Oxidase test
B. Catalase test
C. Coagulase test
D. Urease test
6. The most pathogenic species of Staphylococcus is:
A. S. epidermidis
B. S. aureus
C. S. saprophyticus
D. S. hominis
7. Staphylococcus aureus colonies typically appear:
A. White
B. Golden yellow
C. Red
D. Green
8. The enzyme that differentiates S. aureus from other staphylococci is:
A. Catalase
B. Oxidase
C. Coagulase
D. Urease
9. Majority of Staphylococci on skin are:
A. Coagulase-positive
B. Coagulase-negative
C. Acid-fast
D. Motile
10. Catalase-positive organisms include:
A. Streptococcus
B. Staphylococcus
C. Enterococcus
D. Pneumococcus
11. Hemolysis pattern of S. aureus on blood agar is:
A. Alpha
B. Beta
C. Gamma
D. None
12. S. aureus ferments mannitol to produce:
A. Red colonies
B. Yellow colonies
C. Black colonies
D. White colonies
13. Mannitol Salt Agar selects for Staphylococci due to:
A. High sugar
B. High NaCl concentration
C. Low pH
D. Antibiotics
14. S. epidermidis is best known for:
A. Food poisoning
B. Toxic shock syndrome
C. Biofilm formation
D. Skin peeling toxin
15. S. saprophyticus commonly causes:
A. Pneumonia
B. UTI in young women
C. Meningitis
D. Osteomyelitis
16. Coagulase-negative Staphylococci include:
A. S. aureus
B. S. epidermidis
C. S. pyogenes
D. E. coli
17. The major virulence factor of S. aureus that binds IgG is:
A. Exotoxin A
B. Protein A
C. Hemolysin
D. Coagulase
18. Staphylococcal enterotoxin causes:
A. Diarrhea after 6–12 hours
B. Rapid food poisoning within hours
C. Jaundice
D. Meningitis
19. Toxic Shock Syndrome is caused by:
A. TSST-1
B. Coagulase
C. Beta toxin
D. Alpha hemolysin
20. MRSA carries which gene?
A. blaZ
B. mecA
C. vanA
D. tetM
21. mecA gene encodes:
A. Beta-lactamase
B. Altered PBP2a
C. Protein A
D. Coagulase
22. First-line drug for serious MRSA infection is:
A. Penicillin
B. Vancomycin
C. Gentamicin
D. Tetracycline
23. Common colonization site for S. aureus is:
A. Rectum
B. Nasal cavity
C. Mouth
D. Stomach
24. Staphylococci divide along:
A. One plane
B. Multiple planes
C. Spiral axis
D. Horizontal axis
25. S. aureus possesses:
A. Capsule
B. Flagella
C. Spores
D. Fimbriae
26. Staphylococcal alpha toxin causes:
A. Protein synthesis inhibition
B. Membrane pore formation
C. DNA damage
D. Neurotoxicity
27. Enterotoxins of S. aureus are:
A. Heat-labile
B. Heat-stable
C. Inactivated by cooking
D. Antibiotic sensitive
28. A common hospital-acquired infection caused by S. aureus is:
A. Malaria
B. Surgical wound infection
C. Liver abscess
D. Typhoid
29. S. epidermidis infections commonly involve:
A. Catheters and implants
B. Lungs
C. GI tract
D. Kidneys
30. Coagulase test positive means:
A. No clot formation
B. Clot formation
C. Color change only
D. Rapid hemolysis
31. Staphylococci tolerate:
A. 1% NaCl
B. 7.5% NaCl
C. No salt
D. Only low-salt medium
32. Staphylococcal scalded skin syndrome is due to:
A. TSST-1
B. Exfoliative toxin
C. Enterotoxin
D. Hemolysin
33. Food poisoning by S. aureus is due to:
A. Infection
B. Preformed toxin
C. Endotoxin
D. Coagulase
34. Staphylococci are part of normal flora of:
A. Skin
B. Blood
C. CSF
D. Bone marrow
35. Novobiocin resistance helps differentiate:
A. S. aureus
B. S. saprophyticus
C. S. epidermidis
D. S. hominis
36. Biofilm formation is a key virulence factor of:
A. S. aureus
B. S. epidermidis
C. S. saprophyticus
D. S. lugdunensis
37. On Gram stain, Staphylococci appear:
A. Pink rods
B. Purple cocci
C. Pink cocci
D. Purple rods
38. S. aureus is commonly associated with:
A. Impetigo
B. Pneumonia
C. Osteomyelitis
D. All of the above
39. Beta-lactamase in S. aureus causes resistance to:
A. Methicillin
B. Penicillin
C. Vancomycin
D. Linezolid
40. The most common coagulase-negative Staphylococcus causing device infections is:
A. S. aureus
B. S. epidermidis
C. S. saprophyticus
D. S. hominis
41. Staphylococci grow best at:
A. 20°C
B. 25°C
C. 35–37°C
D. 50°C
42. Staphylococcal toxic shock involves:
A. Superantigen activity
B. Endotoxin action
C. Viral mimicry
D. Hemolysis only
43. Staphylococci are:
A. Acid-fast
B. Non–acid-fast
C. Weakly acid-fast
D. Obligate acid-fast
44. Cell wall of Staphylococci contains:
A. Mycolic acid
B. Teichoic acid
C. Lipopolysaccharide
D. Capsule only
45. S. aureus beta hemolysis results from:
A. Protein A
B. Hemolysins
C. Coagulase
D. Capsule
46. The enzyme catalase breaks down:
A. H₂O₂ → H₂O + O₂
B. H₂O → H⁺ + OH⁻
C. CO₂ → CO + O₂
D. Lipids → fatty acids
47. Staphylococci are best cultured on:
A. MacConkey agar
B. Mannitol salt agar
C. SS agar
D. Thiosulfate agar
48. The structure allowing S. epidermidis to stick to surfaces is:
A. Flagella
B. Biofilm
C. Pili
D. Fimbriae
49. Exfoliative toxin causes:
A. Peeling of skin
B. Food poisoning
C. Fever only
D. Kidney injury
50. S. aureus pneumonia is often seen following:
A. Viral influenza
B. COVID-19 only
C. Asthma
D. Common cold
✅ Answer Key
1-C
2-B
3-B
4-B
5-B
6-B
7-B
8-C
9-B
10-B
11-B
12-B
13-B
14-C
15-B
16-B
17-B
18-B
19-A
20-B
21-B
22-B
23-B
24-B
25-A
26-B
27-B
28-B
29-A
30-B
31-B
32-B
33-B
34-A
35-B
36-B
37-B
38-D
39-B
40-B
41-C
42-A
43-B
44-B
45-B
46-A
47-B
48-B
49-A
50-A
