
Introduction
-
Clostridium is a genus of Gram-positive, spore-forming, obligate anaerobic bacilli of major medical importance.
-
These organisms are widely distributed in soil, dust, water, and the gastrointestinal tract of humans and animals.
-
The presence of endospores enables Clostridium species to survive harsh environmental conditions and facilitates transmission.
-
Many species are highly pathogenic and cause disease mainly through the production of potent exotoxins.
-
Important diseases include:
-
Botulism – caused by Clostridium botulinum
-
Tetanus – caused by Clostridium tetani
-
Gas gangrene and food poisoning – caused by Clostridium perfringens
-
Antibiotic-associated diarrhoea and pseudomembranous colitis – caused by Clostridioides difficile
-
-
Clostridial infections are often rapidly progressive and life-threatening, requiring early diagnosis and prompt treatment.
General Character
Genus: Clostridium
Family
Clostridiaceae
Medically Important Species
-
Clostridium botulinum – Causes botulism, a severe neuroparalytic illness
-
Clostridium tetani – Causes tetanus, characterized by spastic paralysis
-
Clostridium perfringens – Causes gas gangrene (clostridial myonecrosis) and food poisoning
-
Clostridioides (Clostridium) difficile – Causes antibiotic-associated diarrhoea and pseudomembranous colitis
Gram Staining
Clostridia are Gram-positive bacteria, appearing purple on Gram staining due to the presence of a thick peptidoglycan cell wall. Older cultures may appear Gram-variable.
Shape and Arrangement
-
Shape: Large, straight rod-shaped bacilli
-
Arrangement: Commonly seen as single cells or pairs; some species may form short or long chains
Oxygen Requirement
Clostridia are obligate anaerobes, meaning they cannot survive or multiply in the presence of oxygen. Their ability to form resistant endospores allows survival in adverse environmental conditions.
Morphology
Clostridia are large, Gram-positive, anaerobic bacilli with characteristic spore formation, which is an important identifying feature.
Size
- Relatively large bacteria
- Average size: 3–8 µm in length and 0.6–1.2 µm in width
Shape
- Straight or slightly curved rod-shaped bacilli
- Ends may be rounded or square-cut depending on species
Arrangement
- Commonly seen as single cells or in pairs
- Some species may form short or long chains
- Tissue samples often show scanty inflammatory cells (especially in gas gangrene)
Gram Staining
- Gram-positive (purple-stained)
- Older cultures may appear Gram-variable or Gram-negative due to cell wall degeneration
Spore Formation
- Endospore-forming bacteria
- Spore position is species-specific:
- Terminal spores – C. tetani (drumstick appearance)
- Subterminal spores – C. botulinum
- Central or subterminal spores – C. perfringens (rarely seen in clinical specimens)
- Spores are oval or spherical, refractile, and highly resistant to heat and disinfectants
Motility
- Most species are motile due to peritrichous flagella
- C. perfringens is non-motile
Capsule
- Capsule may be present in some species
- C. perfringens has a polysaccharide capsule, contributing to virulence.
Cultural Characteristics
Atmospheric Requirement
-
Grow only under anaerobic conditions
-
Cultured using:
-
Anaerobic jars (GasPak system)
-
Anaerobic chambers
-
Reducing media
-
Temperature
-
Optimum growth at 37°C
-
Some species can grow between 20–50°C
Culture Media
1. Robertson Cooked Meat (RCM) Medium
-
Most commonly used enrichment medium
-
Shows:
-
Turbidity
-
Gas production
-
Meat digestion (proteolysis) – blackening and foul odor
-
-
C. perfringens: Stormy fermentation may be seen
2. Blood Agar (Anaerobic)
-
Colonies vary by species:
-
Large, opaque, irregular colonies
-
Double zone of hemolysis characteristic of C. perfringens:
-
Inner zone: complete (β) hemolysis
-
Outer zone: partial (α) hemolysis
-
-
3. Egg Yolk Agar
-
Used to detect lecithinase activity
-
C. perfringens produces:
-
Opaque zone around colonies due to lecithinase (α-toxin)
-
-
Nagler reaction is positive
4. Selective Media
-
Cycloserine–Cefoxitin–Fructose Agar (CCFA) for C. difficile
-
Yellow colonies with horse-stable odor
-
Fluorescence under UV light
-
Biochemical Reactions
Carbohydrate Fermentation
-
Most Clostridia ferment carbohydrates producing acid and gas
-
Fermentation patterns vary among species and are used for identification
| Species | Glucose Fermentation | Gas Production |
|---|---|---|
| C. perfringens | Positive | Positive |
| C. tetani | Negative | Negative |
| C. botulinum | Variable | Variable |
| C. difficile | Positive | Variable |
Lecithinase Test
-
Detects alpha toxin (lecithinase)
-
Positive in C. perfringens
-
Produces an opaque zone around colonies on egg yolk agar
-
Nagler reaction: Opalescence inhibited by antitoxin (confirmatory)
Lipase Test
-
Detects lipase enzyme
-
Positive in:
-
C. botulinum
-
C. sporogenes
-
-
Produces iridescent sheen on egg yolk agar
Indole Test
-
Positive: C. tetani, C. sporogenes
-
Negative: C. perfringens, C. difficile
Proteolytic Activity
-
Demonstrated in Robertson cooked meat medium
-
Seen as:
-
Digestion of meat
-
Blackening and foul odor
-
-
Strongly positive in:
-
C. sporogenes
-
C. tetani
-
Stormy Fermentation (Litmus Milk Test)
-
Characteristic of C. perfringens
-
Features:
-
Acid clot formation
-
Disruption of clot by gas production
-
Gelatin Liquefaction
-
Positive: C. tetani, C. sporogenes
-
Negative: C. perfringens
Catalase & Oxidase Tests
-
Catalase: Negative
-
Oxidase: Negative
Differentiating Biochemical Reactions
| Test | C. perfringens | C. tetani | C. botulinum | C. difficile |
|---|---|---|---|---|
| Glucose fermentation | + | – | ± | + |
| Gas production | + | – | ± | ± |
| Lecithinase | + | – | – | – |
| Lipase | – | – | + | – |
| Indole | – | + | – | – |
| Stormy fermentation | + | – | – | – |
Pathogenicity
Mechanisms of Pathogenicity
1. Exotoxin Production
Toxin production is the major virulence factor of Clostridium species.
Neurotoxins
-
Clostridium botulinum
-
Produces botulinum toxin
-
Blocks acetylcholine release at neuromuscular junctions
-
Causes flaccid paralysis (botulism)
-
-
Clostridium tetani
-
Produces tetanospasmin
-
Blocks release of GABA and glycine
-
Causes spastic paralysis (tetanus)
-
2. Cytotoxic and Tissue-Destroying Toxins
-
Clostridium perfringens produces multiple toxins:
-
Alpha toxin (lecithinase) – causes cell membrane destruction, hemolysis, and myonecrosis
-
Theta toxin – cardiotoxic and hemolytic
-
-
Results in:
-
Gas gangrene (clostridial myonecrosis)
-
Extensive tissue necrosis
-
Systemic toxemia
-
3. Enterotoxin-Mediated Disease
-
Clostridioides difficile
-
Produces:
-
Toxin A (enterotoxin) – causes fluid secretion and mucosal damage
-
Toxin B (cytotoxin) – causes cell death
-
-
-
Leads to:
-
Antibiotic-associated diarrhoea
-
Pseudomembranous colitis
-
4. Spore Formation and Environmental Survival
-
Spores allow:
-
Long-term survival in soil, dust, and hospital environments
-
Resistance to heat, disinfectants, and drying
-
-
Facilitates transmission and recurrence of infection (especially C. difficile)
5. Anaerobic Tissue Environment
-
Trauma, devitalized tissue, or ischemia create low oxygen tension
-
Favors:
-
Rapid bacterial multiplication
-
Toxin production
-
Gas formation
-
Diseases Caused by Clostridium
| Species | Disease |
|---|---|
| C. botulinum | Botulism |
| C. tetani | Tetanus |
| C. perfringens | Gas gangrene, food poisoning |
| C. difficile | Antibiotic-associated colitis |
| C. septicum | Spontaneous myonecrosis |
Laboratory Diagnosis
Early and accurate laboratory diagnosis of Clostridial infections is essential due to their rapid progression and high mortality. Diagnosis involves a combination of clinical suspicion, microscopy, culture, toxin detection, and molecular methods.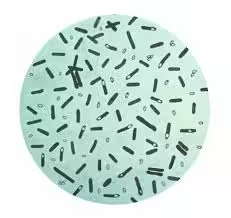
1. Specimen Collection
Specimens should be collected before antibiotic therapy and transported under anaerobic conditions.
| Suspected Disease | Specimen |
|---|---|
| Gas gangrene | Wound exudate, tissue biopsy |
| Tetanus | Wound swab / tissue (organism rarely isolated) |
| Botulism | Serum, stool, gastric aspirate, food sample |
| C. difficile infection | Stool sample |
| Food poisoning | Stool and suspected food |
2. Direct Microscopy
Gram Staining
- Large Gram-positive bacilli
- Spores may be seen:
- Terminal (drumstick appearance) – C. tetani
- In gas gangrene:
- Numerous bacilli
- Few or no pus cells (important diagnostic clue)
3. Culture
Culture must be done under strict anaerobic conditions.
Media Used
- Robertson Cooked Meat (RCM) medium
- Turbidity, gas production
- Meat digestion and foul odor
- Anaerobic Blood Agar
- Colony morphology
- Double zone hemolysis – C. perfringens
- Egg Yolk Agar
- Lecithinase production
- Nagler reaction positive for C. perfringens
- CCFA (Cycloserine-Cefoxitin-Fructose Agar)
- Selective medium for C. difficile
- Yellow colonies with characteristic odor
4. Biochemical Tests
- Sugar fermentation patterns
- Lecithinase and lipase tests
- Indole test
- Stormy fermentation in milk (C. perfringens)
(Used mainly for species differentiation)
5. Toxin Detection
Toxin demonstration is crucial, as disease is primarily toxin-mediated.
Methods
- ELISA / EIA – C. difficile toxins A & B
- PCR – toxin gene detection
- Mouse bioassay (historical gold standard for botulinum toxin)
6. Molecular Methods
- PCR-based assays
- Rapid and sensitive
- Detect toxin-producing strains
- Widely used for C. difficile diagnosis
7. Serological Tests
- Limited role
- Antitoxin detection in specialized laboratories
8. Imaging and Supportive Findings
- Gas in tissues on X-ray / CT scan (gas gangrene)
- Colonoscopy showing pseudomembranes (C. difficile)
Antibiotic Resistance
Antibiotic resistance among Clostridium species is an emerging clinical concern, particularly due to widespread antibiotic misuse, hospital exposure, and the spore-forming ability of these organisms. Resistance patterns vary between species and directly influence treatment strategies.
General Antibiotic Susceptibility
Most Clostridia are traditionally susceptible to:
- Penicillin
- Metronidazole
- Clindamycin
- Vancomycin (especially C. difficile)
However, resistance to several commonly used antibiotics has been increasingly reported.
Mechanisms of Antibiotic Resistance
1. Spore Formation
- Spores are metabolically inactive
- Highly resistant to:
- Antibiotics
- Heat
- Disinfectants
- Major cause of recurrent infections, especially C. difficile
2. Altered Target Sites
- Modification of:
- Penicillin-binding proteins (PBPs)
- Ribosomal binding sites
- Leads to resistance to:
- β-lactams
- Macrolides
3. Enzyme Production
- Some strains produce:
- β-lactamases
- Results in resistance to:
- Penicillins
- Cephalosporins
4. Reduced Drug Uptake
- Thick cell wall and anaerobic metabolism reduce antibiotic penetration
- Particularly affects:
- Aminoglycosides (intrinsically ineffective)
5. Antibiotic-Induced Dysbiosis
- Broad-spectrum antibiotics suppress normal gut flora
- Allows overgrowth of resistant C. difficile strains
Species-Specific Resistance Patterns
Clostridioides difficile
- Increasing resistance to:
- Clindamycin
- Fluoroquinolones
- Cephalosporins
- Usually susceptible to:
- Vancomycin
- Fidaxomicin
- Metronidazole (mild cases)
Clostridium perfringens
- Generally susceptible to:
- Penicillin
- Metronidazole
- Occasional resistance to:
- Clindamycin
Clostridium tetani
- Treatment mainly with:
- Metronidazole
- Antibiotic resistance is rare, as disease is toxin-mediated
Clostridium botulinum
- Antibiotics have limited role
- Antitoxin and supportive care are primary
Prevention
1. Immunization
Tetanus Prevention
-
Tetanus toxoid vaccine is the most effective preventive measure
-
Included in national immunization programs (DPT / Td)
-
Booster doses every 10 years are essential for lifelong protection
-
Proper post-exposure prophylaxis for wounds:
-
Tetanus toxoid
-
Tetanus immunoglobulin (if indicated)
-
2. Proper Wound Care
-
Immediate cleaning and debridement of wounds
-
Removal of devitalized tissue
-
Adequate oxygenation of tissues
-
Especially important in:
-
Traumatic injuries
-
Surgical wounds
-
Crush injuries
-
3. Food Safety Measures
Prevention of botulism and Clostridial food poisoning depends on safe food handling practices.
-
Proper cooking and reheating of food
-
Avoidance of improperly canned or preserved food
-
Maintenance of appropriate food storage temperatures
-
Destruction of spores by:
-
High-temperature pressure cooking (autoclaving)
-
-
Avoid feeding honey to infants (prevention of infant botulism)
4. Hospital Infection Control
Prevention of Clostridioides difficile Infection
-
Judicious use of antibiotics
-
Contact isolation for infected patients
-
Hand hygiene using soap and water (alcohol-based sanitizers are ineffective against spores)
-
Environmental cleaning with sporicidal disinfectants
5. Antibiotic Stewardship
-
Avoid unnecessary broad-spectrum antibiotics
-
Use narrow-spectrum agents when possible
-
Shorten duration of antibiotic therapy
-
Monitor antibiotic resistance patterns
6. Public Health Measures
-
Health education on vaccination and food safety
-
Surveillance of Clostridial infections
-
Proper disposal of animal and human waste
-
Safe agricultural and slaughterhouse practices
7. Special Preventive Strategies
-
Prophylactic antibiotics in high-risk surgical procedures
-
Early identification and isolation of infected individuals
-
Probiotics (adjunct role in preventing recurrent C. difficile infections)
MCQs
1. Clostridium species are best described as:
A. Gram-negative aerobes
B. Gram-positive obligate anaerobes
C. Gram-negative facultative anaerobes
D. Acid-fast bacilli
Answer: B
2. Which Clostridium species causes botulism?
A. C. tetani
B. C. difficile
C. C. botulinum
D. C. perfringens
Answer: C
3. The major virulence factor of Clostridium tetani is:
A. Alpha toxin
B. Enterotoxin
C. Tetanospasmin
D. Lecithinase
Answer: C
4. Drumstick appearance on microscopy is characteristic of:
A. C. perfringens
B. C. botulinum
C. C. difficile
D. C. tetani
Answer: D
5. Double zone of hemolysis on blood agar is seen with:
A. C. tetani
B. C. difficile
C. C. perfringens
D. C. botulinum
Answer: C
6. Which Clostridium is non-motile?
A. C. tetani
B. C. botulinum
C. C. difficile
D. C. perfringens
Answer: D
7. Stormy fermentation in milk is produced by:
A. C. botulinum
B. C. perfringens
C. C. tetani
D. C. difficile
Answer: B
8. Nagler reaction detects which toxin?
A. Enterotoxin
B. Neurotoxin
C. Lecithinase
D. Hemolysin
Answer: C
9. Which organism causes pseudomembranous colitis?
A. C. perfringens
B. C. botulinum
C. C. difficile
D. C. tetani
Answer: C
10. Toxin A and Toxin B are produced by:
A. C. tetani
B. C. botulinum
C. C. difficile
D. C. perfringens
Answer: C
11. Preferred selective medium for C. difficile is:
A. Blood agar
B. MacConkey agar
C. CCFA
D. Lowenstein–Jensen
Answer: C
12. Which Clostridium produces flaccid paralysis?
A. C. tetani
B. C. botulinum
C. C. perfringens
D. C. difficile
Answer: B
13. Gas gangrene is also known as:
A. Cellulitis
B. Pseudomembranous colitis
C. Myonecrosis
D. Septic arthritis
Answer: C
14. Alpha toxin of C. perfringens is a:
A. Protease
B. Lipase
C. Lecithinase
D. DNase
Answer: C
15. Which Clostridium infection is mainly a clinical diagnosis?
A. Botulism
B. Tetanus
C. Food poisoning
D. Colitis
Answer: B
16. Spores of Clostridium help in:
A. Rapid growth
B. Antibiotic production
C. Environmental survival
D. Capsule formation
Answer: C
17. Gram stain of gas gangrene tissue typically shows:
A. Numerous pus cells
B. No bacteria
C. Gram-negative cocci
D. Numerous bacilli with few pus cells
Answer: D
18. Which antibiotic is most effective against anaerobes including Clostridium?
A. Gentamicin
B. Metronidazole
C. Azithromycin
D. Ciprofloxacin
Answer: B
19. Antibiotic most commonly associated with C. difficile infection is:
A. Penicillin
B. Metronidazole
C. Clindamycin
D. Vancomycin
Answer: C
20. Which Clostridium causes food poisoning with short incubation?
A. C. tetani
B. C. botulinum
C. C. perfringens
D. C. difficile
Answer: C
21. Lipase positive Clostridium is:
A. C. perfringens
B. C. botulinum
C. C. tetani
D. C. difficile
Answer: B
22. Best prevention of tetanus is:
A. Antibiotics
B. Antitoxin only
C. Vaccination with toxoid
D. Isolation
Answer: C
23. Which Clostridium shows terminal spores?
A. C. perfringens
B. C. difficile
C. C. botulinum
D. C. tetani
Answer: D
24. Which Clostridium is part of normal gut flora?
A. C. tetani
B. C. botulinum
C. C. difficile
D. C. septicum
Answer: C
25. Anaerobic culture is essential because Clostridia are:
A. Aerobes
B. Facultative anaerobes
C. Microaerophilic
D. Obligate anaerobes
Answer: D
26. Which disinfectant is ineffective against C. difficile spores?
A. Chlorine
B. Soap and water
C. Alcohol-based sanitizer
D. Bleach
Answer: C
27. Gas production in tissues is mainly due to:
A. Protein metabolism
B. Lipid metabolism
C. Carbohydrate fermentation
D. Capsule formation
Answer: C
28. Which Clostridium is commonly associated with malignancy of colon?
A. C. difficile
B. C. septicum
C. C. botulinum
D. C. tetani
Answer: B
29. Which toxin inhibits release of GABA and glycine?
A. Botulinum toxin
B. Alpha toxin
C. Enterotoxin
D. Tetanospasmin
Answer: D
30. The preferred drug for severe C. difficile infection is:
A. Metronidazole
B. Ciprofloxacin
C. Vancomycin
D. Amoxicillin
Answer: C
31. Lecithinase test is done using:
A. Blood agar
B. Chocolate agar
C. Egg yolk agar
D. MacConkey agar
Answer: C
32. Which Clostridium is least invasive but highly toxic?
A. C. perfringens
B. C. tetani
C. C. botulinum
D. C. septicum
Answer: C
33. Foul smell in Clostridial infection is due to:
A. Ammonia
B. Fatty acids
C. Sulfur
D. Ketones
Answer: B
34. Which antibiotic has no role in treating tetanus?
A. Metronidazole
B. Penicillin
C. Vancomycin
D. Antibiotics play only adjunct role
Answer: C
35. Best method to destroy Clostridium spores is:
A. Boiling
B. Alcohol
C. Autoclaving
D. UV radiation
Answer: C
36. C. difficile toxins are detected by:
A. Widal test
B. ELISA
C. Coagulase test
D. Urease test
Answer: B
37. Which Clostridium commonly causes food poisoning via reheated meat?
A. C. botulinum
B. C. difficile
C. C. tetani
D. C. perfringens
Answer: D
38. Incubation period of tetanus is usually:
A. Hours
B. 1–2 days
C. 7–10 days
D. Months
Answer: C
39. Which Clostridium shows minimal pus formation?
A. C. difficile
B. C. perfringens
C. C. botulinum
D. C. tetani
Answer: B
40. First step in gas gangrene management is:
A. Antibiotics only
B. Vaccination
C. Surgical debridement
D. Antitoxin
Answer: C
41. Which Clostridium is indole positive?
A. C. perfringens
B. C. difficile
C. C. tetani
D. C. botulinum
Answer: C
42. Antibiotic resistance is most significant in:
A. C. tetani
B. C. botulinum
C. C. perfringens
D. C. difficile
Answer: D
43. Alcohol-based hand rubs are ineffective against:
A. Vegetative cells
B. Viruses
C. Spores
D. Fungi
Answer: C
44. Infant botulism is associated with consumption of:
A. Milk
B. Eggs
C. Honey
D. Meat
Answer: C
45. Which toxin is cardiotoxic?
A. Tetanospasmin
B. Botulinum toxin
C. Theta toxin
D. Enterotoxin
Answer: C
46. Robertson cooked meat medium shows blackening due to:
A. Acid production
B. Gas bubbles
C. Proteolysis
D. Capsule formation
Answer: C
47. Clostridium infections are favored by:
A. High oxygen tension
B. Ischemic tissue
C. High pH
D. Dry environment
Answer: B
48. Which Clostridium is capsulated?
A. C. tetani
B. C. botulinum
C. C. perfringens
D. C. difficile
Answer: C
49. Most important preventive measure against tetanus:
A. Antibiotics
B. Steroids
C. Vaccination
D. Isolation
Answer: C
50. Clostridium species belong to family:
A. Bacillaceae
B. Enterobacteriaceae
C. Clostridiaceae
D. Corynebacteriaceae
Answer: C