Introduction
-
Diphtheria is an acute, communicable, toxin-mediated bacterial infection.
-
It primarily affects the upper respiratory tract, especially the tonsils, pharynx, and larynx.
-
The disease is caused by Corynebacterium diphtheriae.
-
A characteristic feature of diphtheria is the formation of a grayish-white pseudomembrane over the throat.
-
The pseudomembrane may lead to airway obstruction and respiratory distress.
-
Diphtheria toxin is responsible for both local tissue necrosis and systemic toxicity.
-
Systemic absorption of the toxin can cause serious complications such as myocarditis and neuropathy.
-
Humans are the only reservoir of infection.
-
The disease spreads mainly through respiratory droplets and close contact.
-
Diphtheria was a major cause of childhood mortality before the introduction of vaccination.
-
The incidence has markedly decreased due to routine immunization programs.
-
However, diphtheria still occurs in areas with low immunization coverage, overcrowding, and poor socioeconomic conditions.
-
Diphtheria is a vaccine-preventable disease, and immunization remains the cornerstone of prevention.

Causative Agent
Diphtheria is caused by Corynebacterium diphtheriae.
Morphological Characteristics
-
Gram-positive, pleomorphic bacilli
-
Club-shaped rods with irregular swelling at one end
-
Arranged in Chinese-letter or palisade pattern due to snapping division
-
Non-motile and non-spore forming
-
Aerobic or facultative anaerobic
Staining Features
-
Gram stain: Gram-positive pleomorphic bacilli
-
Albert stain: Green bacilli with bluish-black metachromatic (volutin) granules at the poles
Biotypes
Based on colony morphology and biochemical reactions:
-
Gravis
-
Mitis
-
Intermedius
Important: Disease severity depends on toxin production, not on biotype.
Virulence Factor: Diphtheria Toxin
The most important virulence factor of C. diphtheriae is the diphtheria exotoxin.
-
The toxin is encoded by the tox gene, which is carried by a β-corynephage
-
Only toxigenic strains produce classical diphtheria
Mechanism of Action
-
The toxin inhibits protein synthesis by inactivating elongation factor-2 (EF-2)
-
This leads to cell death and tissue necrosis
Effects of the Toxin
-
Local tissue damage → pseudomembrane formation
-
Systemic absorption → damage to:
-
Heart (myocarditis)
-
Nervous system (neuritis)
-
Kidneys (rare)
-
Epidemiology
-
Humans are the only reservoir
-
Occurs worldwide but more common in:
-
Unimmunized or partially immunized children
-
Overcrowded living conditions
-
Poor sanitation and nutrition
-
-
No natural immunity; protection is acquired only through vaccination or previous infection
-
Waning immunity in adults can lead to outbreaks if booster doses are not taken
Mode of Transmission
-
Respiratory droplets during coughing or sneezing
-
Direct contact with secretions from infected individuals
-
Rarely through contaminated fomites
The disease spreads easily in close-contact settings, such as households and schools.
Incubation Period
-
Usually 2–5 days
-
Range: 1–10 days
Pathogenesis
-
C. diphtheriae enters the body through the respiratory tract
-
The organism colonizes the tonsils, pharynx, or larynx
-
Local multiplication occurs without tissue invasion
-
The exotoxin causes:
-
Local epithelial cell death
-
Inflammation and exudation
-
-
A pseudomembrane is formed, composed of:
-
Fibrin
-
Necrotic epithelial cells
-
Inflammatory cells
-
Bacteria
-
Clinical importance:
Forceful removal of the pseudomembrane causes bleeding and may worsen airway obstruction.
-
Absorbed toxin enters the bloodstream, leading to systemic complications
Clinical Manifestations
1. Respiratory Diphtheria (Most Common Form)
-
Sore throat
-
Low-grade fever
-
Malaise
-
Dysphagia (difficulty in swallowing)
-
Grayish-white pseudomembrane over tonsils or pharynx
-
Cervical lymphadenopathy leading to “bull neck” appearance
2. Laryngeal Diphtheria
-
Hoarseness of voice
-
Stridor
-
Severe respiratory distress
-
High risk of asphyxia, especially in children
3. Nasal Diphtheria
-
Serosanguinous nasal discharge
-
Mild systemic symptoms
-
Common in infants
4. Cutaneous Diphtheria
-
Chronic, non-healing skin ulcers
-
Usually mild but acts as a source of infection
Systemic Complications
Complications occur due to circulating diphtheria toxin:
1. Cardiac Complications
-
Myocarditis (most serious)
-
Arrhythmias
-
Heart failure
-
Occurs during the 2nd–3rd week of illness
2. Neurological Complications
-
Peripheral neuritis
-
Palatal paralysis (nasal speech, regurgitation of food)
-
Cranial nerve palsies
-
Limb weakness
3. Others
-
Renal damage (rare)
-
Secondary bacterial infections
Laboratory Diagnosis
1. Specimen Collection
Specimen of Choice
-
Throat swab from:
-
Edge of the pseudomembrane
-
Area beneath the pseudomembrane (if safely possible)
-
Important:
-
Swabs should be collected before starting antibiotics or antitoxin
-
Forceful removal of pseudomembrane should be avoided as it may cause bleeding
Other Specimens
-
Nasal swab (in nasal diphtheria)
-
Swab from skin lesions (cutaneous diphtheria)
2. Microscopic Examination
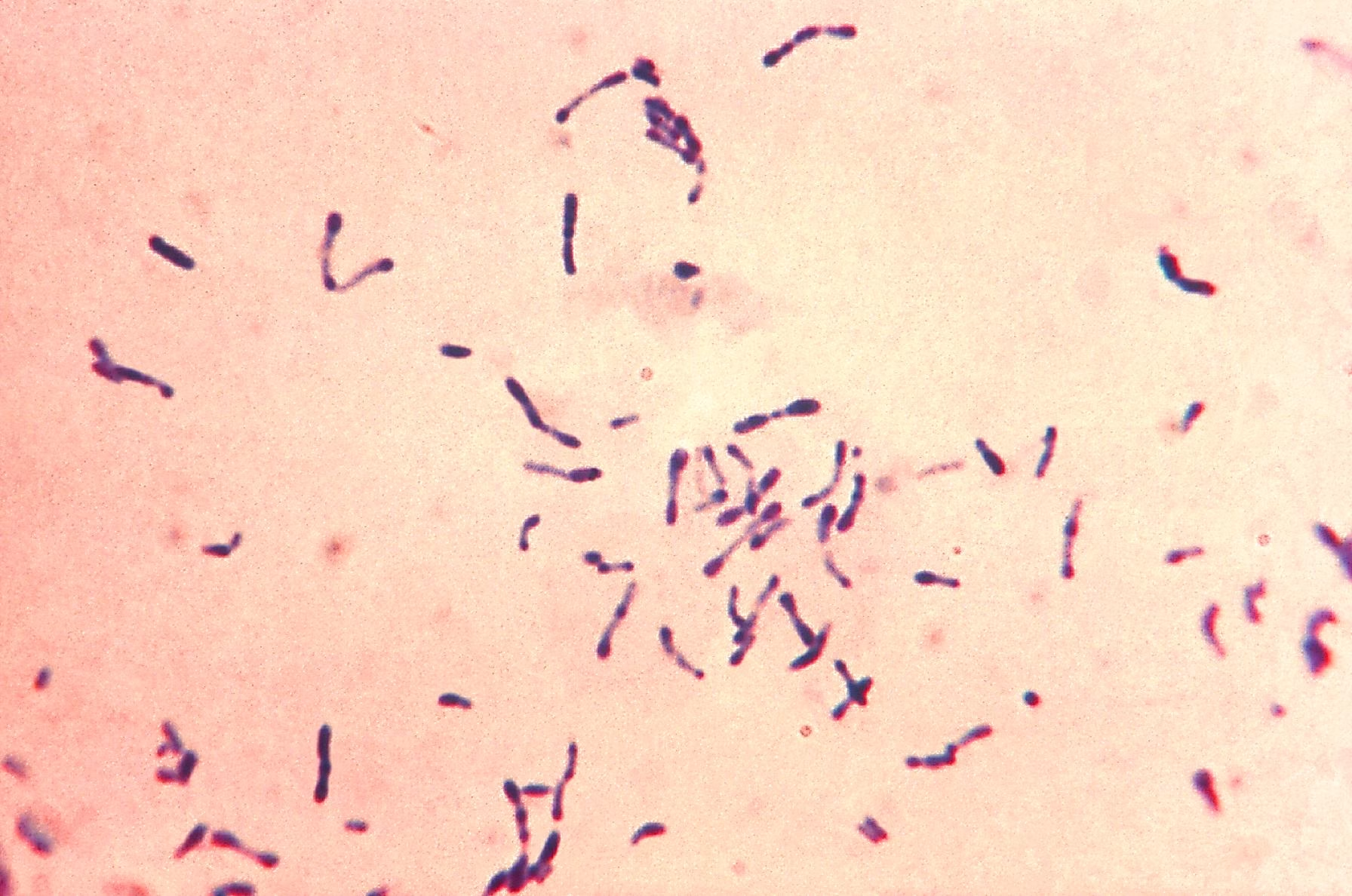
Gram Staining
-
Shows:
-
Gram-positive, pleomorphic bacilli
-
Club-shaped rods
-
Arranged in Chinese-letter (V, L, Y) pattern
-
Limitation:
-
Gram stain is suggestive but not confirmatory
Albert Staining (Special Stain)
-
Demonstrates metachromatic (volutin) granules
-
Findings:
-
Bacilli: Green
-
Granules: Bluish-black, present at the poles
-
Exam Point:
Albert stain is highly useful for presumptive diagnosis.
3. Culture
Culture is essential for definitive identification of the organism.
Culture Media Used
a) Löffler’s Serum Slope
-
Enriched medium
-
Enhances:
-
Rapid growth (within 6–8 hours)
-
Formation of metachromatic granules
-
-
Useful for early diagnosis
b) Potassium Tellurite Agar (Selective Medium)
-
Inhibits growth of normal throat flora
-
Corynebacterium diphtheriae reduces tellurite to tellurium
Colony Appearance:
-
Gray to black colonies
-
Different biotypes show characteristic colony morphology
Incubation Conditions
-
Temperature: 35–37°C
-
Atmosphere: Aerobic
-
Time: 24–48 hours
4. Identification Tests
After culture, colonies are identified by:
-
Gram staining
-
Albert staining
-
Biochemical tests (sugar fermentation patterns)
-
Biotype differentiation (Gravis, Mitis, Intermedius)
5. Demonstration of Toxin Production (Most Important Step)
Clinical significance:
Only toxigenic strains cause classical diphtheria. Hence, toxin demonstration is mandatory.
Elek’s Gel Precipitation Test (Gold Standard)
-
In vitro immunodiffusion test
-
Principle:
-
Diphtheria toxin diffuses from bacterial growth
-
Antitoxin diffuses from filter paper strip
-
Formation of precipitin lines indicates toxin production
-
Interpretation:
-
Positive test → toxigenic strain
-
Negative test → non-toxigenic strain
Molecular Methods
-
PCR for tox gene
-
Rapid and highly sensitive
-
Used in reference or advanced laboratories
6. Serological Tests
-
Antibody detection has limited diagnostic value
-
Mainly useful for:
-
Epidemiological studies
-
Assessing immune status
-
-
Not recommended for routine diagnosis
Treatment
1. Diphtheria Antitoxin
-
Neutralizes circulating toxin
-
Must be administered as early as possible
-
Does not reverse already established tissue damage
2. Antibiotic Therapy
-
Penicillin or Erythromycin
-
Eliminates the organism and prevents transmission
3. Supportive Care
-
Airway management
-
Bed rest
-
Cardiac monitoring
-
Isolation of the patient
Prevention and Control
Immunization
-
Diphtheria toxoid vaccine given as:
-
DPT / DT in children
-
Td booster in adolescents and adults
-
-
Booster doses are essential due to waning immunity
Public Health Measures
-
Isolation of cases
-
Chemoprophylaxis for close contacts
-
Surveillance and outbreak control
Public Health Importance
-
Diphtheria is a vaccine-preventable disease
-
Resurgence occurs due to:
-
Inadequate vaccination
-
Migration
-
Vaccine hesitancy
-
-
Early diagnosis and rapid treatment significantly reduce mortality
MCQs
1. Diphtheria is caused by:
A. Streptococcus pyogenes
B. Corynebacterium diphtheriae
C. Bordetella pertussis
D. Staphylococcus aureus
Answer: B
2. Diphtheria is primarily a disease of:
A. Skin
B. Gastrointestinal tract
C. Upper respiratory tract
D. Central nervous system
Answer: C
3. The characteristic lesion of diphtheria is:
A. Ulcer
B. Vesicle
C. Pseudomembrane
D. Abscess
Answer: C
4. The pseudomembrane in diphtheria is composed mainly of:
A. Mucus only
B. Necrotic tissue and fibrin
C. Pus cells
D. Blood clot
Answer: B
5. Attempted removal of pseudomembrane causes:
A. Healing
B. No effect
C. Bleeding
D. Scar formation
Answer: C
6. Corynebacterium diphtheriae is:
A. Gram-negative cocci
B. Gram-positive bacillus
C. Acid-fast bacillus
D. Spirochete
Answer: B
7. Arrangement of C. diphtheriae is typically:
A. Chains
B. Clusters
C. Chinese-letter pattern
D. Diplococci
Answer: C
8. Special stain used to demonstrate metachromatic granules is:
A. Ziehl–Neelsen stain
B. Giemsa stain
C. Albert stain
D. India ink
Answer: C
9. Metachromatic granules contain:
A. Glycogen
B. Lipid
C. Polyphosphate
D. Protein
Answer: C
10. C. diphtheriae is:
A. Motile
B. Spore forming
C. Non-motile and non-spore forming
D. Flagellated
Answer: C
11. Virulence of diphtheria depends mainly on:
A. Capsule
B. Spore
C. Exotoxin production
D. Enzyme secretion
Answer: C
12. Diphtheria toxin inhibits:
A. DNA synthesis
B. RNA synthesis
C. Protein synthesis
D. Cell wall synthesis
Answer: C
13. Diphtheria toxin acts by inactivating:
A. RNA polymerase
B. Ribosome
C. Elongation factor-2 (EF-2)
D. DNA gyrase
Answer: C
14. The tox gene is carried by:
A. Plasmid
B. Transposon
C. β-corynephage
D. Chromosome only
Answer: C
15. Only which strains cause classical diphtheria?
A. Non-capsulated strains
B. Non-toxigenic strains
C. Toxigenic strains
D. Resistant strains
Answer: C
16. Common biotypes of C. diphtheriae include all EXCEPT:
A. Gravis
B. Mitis
C. Intermedius
D. Lenta
Answer: D
17. Humans are the:
A. Intermediate host
B. Accidental host
C. Only reservoir
D. Animal reservoir
Answer: C
18. Mode of transmission of diphtheria is mainly:
A. Feco-oral route
B. Vector-borne
C. Respiratory droplets
D. Blood transfusion
Answer: C
19. Incubation period of diphtheria is usually:
A. 1–2 hours
B. 2–5 days
C. 10–14 days
D. 1 month
Answer: B
20. The most common form of diphtheria is:
A. Nasal
B. Cutaneous
C. Respiratory
D. Intestinal
Answer: C
21. “Bull neck” appearance is due to:
A. Thyroid enlargement
B. Edema and lymphadenopathy
C. Muscle spasm
D. Fat deposition
Answer: B
22. Most serious complication of diphtheria is:
A. Pneumonia
B. Myocarditis
C. Hepatitis
D. Nephritis
Answer: B
23. Neurological complication commonly seen is:
A. Seizures
B. Peripheral neuritis
C. Meningitis
D. Stroke
Answer: B
24. Specimen of choice for diagnosis is:
A. Blood
B. Sputum
C. Throat swab
D. Urine
Answer: C
25. Best site for collecting throat swab is:
A. Center of pseudomembrane
B. Edge of pseudomembrane
C. Tongue
D. Cheek
Answer: B
26. Culture medium that enhances granule formation is:
A. Blood agar
B. Chocolate agar
C. Löffler’s serum slope
D. MacConkey agar
Answer: C
27. Selective medium for C. diphtheriae is:
A. TCBS agar
B. Lowenstein–Jensen medium
C. Potassium tellurite agar
D. CLED agar
Answer: C
28. Colonies on tellurite agar appear:
A. Green
B. Yellow
C. Black or gray
D. Red
Answer: C
29. Gold standard test for toxin detection is:
A. PCR
B. ELISA
C. Elek’s test
D. Agglutination
Answer: C
30. Elek’s test is based on:
A. Agglutination
B. Complement fixation
C. Gel precipitation
D. Hemagglutination
Answer: C
31. Treatment of diphtheria includes all EXCEPT:
A. Antibiotics
B. Antitoxin
C. Vaccination only
D. Supportive care
Answer: C
32. Drug of choice for diphtheria treatment is:
A. Penicillin or erythromycin
B. Ciprofloxacin
C. Tetracycline
D. Vancomycin
Answer: A
33. Diphtheria antitoxin acts by:
A. Killing bacteria
B. Neutralizing circulating toxin
C. Preventing colonization
D. Stimulating immunity
Answer: B
34. Antitoxin is most effective when given:
A. Late in disease
B. After complications
C. Early in disease
D. Only after culture confirmation
Answer: C
35. Diphtheria vaccine is a:
A. Live attenuated vaccine
B. Killed vaccine
C. Toxoid
D. Subunit vaccine
Answer: C
36. Diphtheria toxoid is given as part of:
A. BCG
B. OPV
C. DPT
D. Hepatitis B vaccine
Answer: C
37. Booster doses are required because:
A. Vaccine is weak
B. Natural immunity is strong
C. Immunity wanes with time
D. Bacteria mutate rapidly
Answer: C
38. Cutaneous diphtheria presents as:
A. Vesicles
B. Bullae
C. Chronic non-healing ulcers
D. Papules
Answer: C
39. Nasal diphtheria commonly occurs in:
A. Adults
B. Elderly
C. Infants
D. Pregnant women
Answer: C
40. Systemic toxicity in diphtheria is due to:
A. Bacterial invasion
B. Capsule
C. Circulating toxin
D. Immune complex deposition
Answer: C
41. Removal of pseudomembrane is discouraged because it may cause:
A. Healing
B. Bleeding and toxin absorption
C. Pain only
D. Scar formation
Answer: B
42. C. diphtheriae grows best in:
A. Anaerobic conditions
B. Aerobic conditions
C. Microaerophilic conditions
D. CO₂-free environment
Answer: B
43. Which is NOT a complication of diphtheria?
A. Myocarditis
B. Neuritis
C. Acute renal failure
D. Bronchial asthma
Answer: D
44. Case fatality rate is highest in:
A. Immunized adults
B. Unimmunized children
C. Vaccinated adolescents
D. Carriers
Answer: B
45. Isolation of diphtheria patient is important to:
A. Reduce pain
B. Prevent toxin action
C. Prevent transmission
D. Increase immunity
Answer: C
46. Chemoprophylaxis is recommended for:
A. General population
B. Hospital staff only
C. Close contacts
D. Recovered patients
Answer: C
47. Diphtheria is best prevented by:
A. Early antibiotics
B. Good nutrition
C. Immunization
D. Isolation alone
Answer: C
48. Which organ is most commonly affected by diphtheria toxin?
A. Liver
B. Heart
C. Lung
D. Spleen
Answer: B
49. Palatal paralysis is due to:
A. Muscle damage
B. Bone involvement
C. Peripheral neuritis
D. Edema
Answer: C
50. Diphtheria is a:
A. Viral disease
B. Protozoal disease
C. Toxin-mediated bacterial disease
D. Fungal infection
Answer: C