Introduction
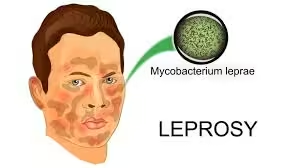
- Leprosy, or Hansen’s disease, is a chronic infectious disease primarily caused by Mycobacterium leprae.
- This intracellular bacterium primarily affects the skin, peripheral nerves, mucosal surfaces, and eyes, leading to significant morbidity.
- While the global burden of leprosy has declined, it remains endemic in certain regions, necessitating effective diagnostic strategies for early detection and treatment.
Clinical Presentation
Common Symptoms
Leprosy manifests in several forms, primarily categorized into:
- Tuberculoid Leprosy (Paucibacillary):
- Characterized by a few well-defined skin lesions that are often numb.
- The immune response is strong, limiting bacterial proliferation.
- Lepromatous Leprosy (Multibacillary):
- Characterized by numerous lesions, nodules, and diffuse skin thickening.
- A weaker immune response leads to widespread bacterial dissemination.
Other Symptoms
- Peripheral Nerve Damage: Resulting in weakness, loss of sensation, and deformities (e.g., claw hand, foot drop).
- Mucosal Lesions: May affect the nasal passages, leading to nasal obstruction or epistaxis.
- Ocular Involvement: This can result in keratitis or blindness if untreated.
Sample Collection
- Skin Biopsy
- Method: A punch biopsy from the edge of a lesion is ideal, as this area is most likely to contain viable bacteria.
- Handling: Samples should be transported in sterile conditions to prevent contamination.
- Smears
- Direct Smears: Skin scrapings or lesions can be examined directly under a microscope for the presence of AFB.
- Other Specimens
- Nerve Biopsy: In specific cases, biopsies of affected nerves may be performed to assess nerve involvement.
Laboratory Techniques
Histopathology
A. Microscopic Examination
- Staining Techniques:
- Ziehl-Neelsen Stain: A traditional stain that identifies AFB. Although effective, it may not be the most sensitive method for detecting M. leprae.
- Fite-Faraco Stain: Specifically designed for M. leprae, this stain enhances the visibility of the bacteria in tissue sections.
B. Pathological Findings
- Tuberculoid Leprosy:
- Characterized by well-formed granulomas, epithelioid cells, and lymphocytes, often with few or no bacilli.
- Lepromatous Leprosy:
- Diffuse infiltration of macrophages with large numbers of bacilli, often presenting as foamy macrophages.
Bacteriological Examination
A. Direct Smear Preparation
- Skin Scrapings: These are prepared from lesions, stained, and examined for AFB.
- Interpretation: A positive direct smear confirms the presence of M. leprae.
Molecular Methods
A. Nucleic Acid Amplification Tests (NAATs)
- PCR: This technique is increasingly used to detect the presence of M. leprae DNA in clinical samples.
- Advantages: High sensitivity and specificity, rapid results compared to culture.
B. Gene-Based Techniques
- LAMP (Loop-Mediated Isothermal Amplification): A newer method that amplifies specific regions of M. leprae DNA, showing promise for point-of-care diagnostics.
Serological Tests
- Antibody Detection Tests: Various tests detect antibodies against specific antigens of M. leprae:
- Anti-PGL-1 Test: Detects antibodies against phenolic glycolipid-1, associated with lepromatous leprosy.
- Lepromin Test: A skin test to assess the immune response to M. leprae antigens. A positive reaction indicates tuberculoid leprosy and a robust immune response.
Interpretation of Results
- Histopathological Findings
- Presence of AFB: A definitive sign of leprosy; numerous bacilli indicate lepromatous leprosy, while few or none suggest tuberculoid leprosy.
- Granuloma Formation: The type of immune response can be inferred from the histological pattern.
- Bacteriological Examination
- Positive Smear: Confirms the diagnosis of leprosy, particularly in multibacillary forms.
- Negative Smear: Does not exclude leprosy, especially in early or paucibacillary cases.
- Molecular Testing
- Positive PCR Result: Indicates the presence of M. leprae DNA, confirming the diagnosis.
- Negative PCR Result: A negative result may occur in cases with low bacterial loads.
- Serological Tests
- Positive Results: Indicate exposure but must be interpreted contextually, as they do not confirm active disease.
- Negative Results: This can occur in early leprosy or certain forms of the disease.
Clinical Implications
Treatment
- The World Health Organization (WHO) recommends a multi-drug therapy (MDT) regimen:
- Paucibacillary Leprosy: Rifampicin and dapsone for 6 months.
- Multibacillary Leprosy: Rifampicin, dapsone, and clofazimine for 12 months.
- Treatment is highly effective and can halt disease progression and transmission.
Follow-Up
- Regular clinical assessments are essential to monitor treatment response and manage potential side effects.
- Patients may need rehabilitation services for disabilities resulting from nerve damage.
Public Health Considerations
- Leprosy is a notifiable disease; healthcare providers must report cases to public health authorities.
- Community education is vital to reduce stigma and encourage early treatment.
Challenges in Diagnosis
- Stigma: Societal misconceptions about leprosy can delay diagnosis and treatment.
- Misdiagnosis: The clinical presentation can overlap with other skin diseases, leading to misdiagnosis.
- Access to Healthcare: In endemic regions, healthcare facilities may be limited.
Advances in Leprosy Diagnostics
Emerging Techniques
- Point-of-Care Tests: Development of rapid tests for M. leprae detection in resource-limited settings.
- Whole Genome Sequencing: Increasingly used in research to understand genetic variations of M. leprae, antibiotic resistance, and epidemiology.
Research Directions
- Ongoing studies are focused on improving serological tests and developing vaccines against leprosy.
- Enhanced understanding of the immune response to M. leprae may lead to novel diagnostic approaches and treatments.