
Introduction
- Giardia lamblia (also known as Giardia intestinalis or Giardia duodenalis) is a protozoan parasite and one of the most common causes of intestinal infections worldwide.
- It belongs to the class Zoomastigophorea and is responsible for giardiasis, a diarrheal disease that significantly affects humans and various animals.
- The parasite alternates between two forms: the motile trophozoite and the environmentally resistant cyst, facilitating survival and transmission.
- Giardiasis is prevalent in regions with poor sanitation but can also affect individuals in developed countries, especially hikers, travelers, or those exposed to untreated water.
- The disease is transmitted via the fecal-oral route, often through contaminated food, water, or person-to-person contact.
- Symptoms range from mild gastrointestinal discomfort to severe malabsorption and chronic diarrhea.
- Understanding Giardia’s biology and life cycle is crucial for effective diagnosis, treatment, and prevention.
Geographical Distribution
Giardia lamblia has a global distribution, affecting people across all continents.
- Endemic regions: The highest prevalence occurs in low-income countries with inadequate sanitation, including parts of Africa, Asia, Latin America, and Eastern Europe.
- Developed regions: In industrialized countries, outbreaks are often associated with contaminated water sources or food, especially during recreational activities (e.g., swimming in lakes or rivers).
- High-risk populations: Children in daycare centers, immunocompromised individuals, travelers, hikers, and refugees are particularly vulnerable.
Habitat
The habitat of Giardia lamblia varies based on its life cycle stage:
- Trophozoite:
- Resides in the small intestine, particularly the duodenum and jejunum.
- Attaches to intestinal epithelial cells using a ventral adhesive disc but does not invade tissue.
- Thrives in an anaerobic or microaerophilic environment.
- Cyst:
- Found in the colon during the encystation phase and excreted in feces.
- Survives in external environments, including water, soil, and food, for weeks to months due to its tough, protective wall.
Morphology
Giardia lamblia exhibits two distinct morphological forms:
- Trophozoite:
- Shape: Pear-shaped (teardrop-like).
- Size: 9–21 µm in length and 5–15 µm in width.
- Structure:
- Binucleate, with two prominent nuclei containing central karyosomes.
- Ventral adhesive disc for attachment to the intestinal mucosa.
- Four pairs of flagella (8 total) for motility.
- Function: Active feeding and reproduction stage in the host’s intestine.
- Cyst:
- Shape: Oval.
- Size: 8–14 µm in length and 7–10 µm in width.
- Structure:
- Protective thick wall, enabling survival in harsh conditions.
- Four nuclei (mature cyst).
- Internally contains retracted flagella and trophozoite precursors.
- Function: Infective stage; facilitates transmission between hosts.
Life Cycle
The life cycle of Giardia lamblia involves two stages and is completed in a single host:
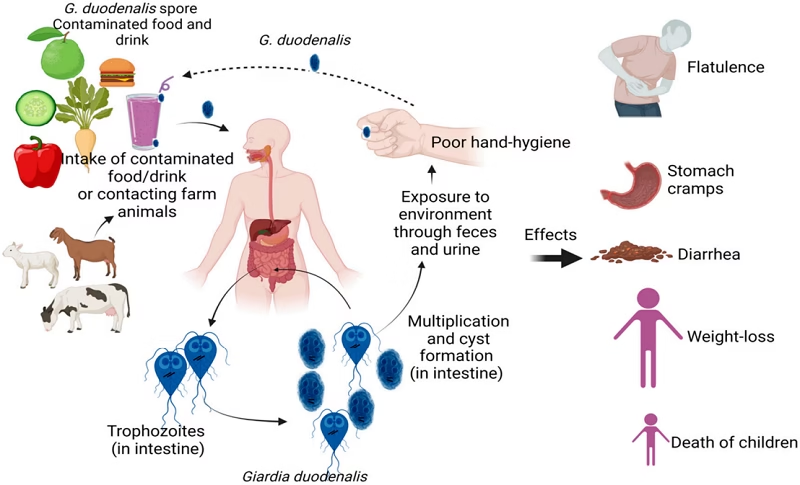
- Ingestion:
- Infection begins when cysts are ingested via contaminated water, food, or direct contact.
- Excystation:
- In the stomach and duodenum, gastric acid and intestinal enzymes trigger the release of trophozoites from cysts.
- Each cyst produces two trophozoites.
- Colonization:
- Trophozoites multiply asexually (binary fission) and attach to the intestinal epithelium.
- This leads to disruption of intestinal functions.
- Encystation:
- In the colon, trophozoites encyst under unfavorable conditions (e.g., dehydration).
- Excretion:
- Cysts are passed in feces, surviving in the environment until a new host ingests them.
Mode of Transmission
Giardia lamblia is transmitted via the fecal-oral route:
- Waterborne transmission:
- Drinking or recreational water contaminated with cysts is the most common mode.
- Outbreaks often occur in settings with untreated or poorly treated water supplies.
- Foodborne transmission:
- Consumption of food contaminated by infected handlers or exposure to untreated irrigation water.
- Person-to-person transmission:
- Common in daycare centers, nursing homes, and households due to poor hygiene.
- It can also occur through oral-anal contact, particularly in sexual practices.
- Zoonotic transmission:
- Cysts from infected animals (e.g., beavers, dogs, livestock) can contaminate water sources.
Incubation Time
The incubation period for giardiasis ranges from 1 to 2 weeks (commonly 7–10 days) after the ingestion of cysts. This variability depends on the infective dose, host immune status and other environmental factors.
Pathogenesis
The pathogenic mechanisms of Giardia lamblia involve both mechanical and biochemical effects:
- Adhesion to the intestinal mucosa:
- Trophozoites attach to epithelial cells using their ventral adhesive discs.
- This causes mechanical irritation and damage to the intestinal lining.
- Disruption of absorption:
- Villous atrophy and crypt hyperplasia reduce the absorptive surface area of the small intestine.
- Leads to the malabsorption of nutrients, particularly fats, carbohydrates, and vitamins (e.g., vitamin B12).
- Enzymatic dysfunction:
- Decreased activity of brush border enzymes (e.g., lactase) causes lactose intolerance and osmotic diarrhea.
- Immune response:
- The host’s immune response to the parasite can lead to inflammation, further exacerbating diarrhea and nutrient loss.
Clinical Manifestations:
- Acute giardiasis: Watery diarrhea, bloating, flatulence, nausea, and abdominal cramps.
- Chronic giardiasis: Prolonged malabsorption, weight loss, fatigue, and steatorrhea (fatty stools).
- Asymptomatic carriers: Many individuals remain asymptomatic but shed infectious cysts.
Laboratory Diagnosis
Accurate diagnosis of giardiasis involves the detection of Giardia lamblia in stool or intestinal samples:
- Microscopy:
- Direct stool examination for trophozoites or cysts.
- Concentration techniques (e.g., flotation, sedimentation) improve detection.
- Antigen detection:
- Enzyme-linked immunosorbent assay (ELISA) or immunochromatographic tests detect Giardia-specific antigens in stool.
- Molecular methods:
- Polymerase chain reaction (PCR) for detecting Giardia DNA in stool samples.
- Provides high sensitivity and specificity.
- String test (Enterotest):
- Evolving a gelatin capsule with a string to collect intestinal contents for analysis.
- Duodenal aspiration or biopsy:
- Used in rare, refractory cases to confirm the presence of trophozoites in the upper small intestine.
Treatment
Giardiasis treatment aims to eliminate the parasite, resolve symptoms, and prevent transmission.
- Antiparasitic Drugs:
- Metronidazole: First-line treatment (250 mg three times daily for 5–7 days in adults).
- Tinidazole: Single-dose therapy (2 g).
- Nitazoxanide: An effective alternative for children and adults.
- Albendazole: Occasionally used, particularly in cases of resistance or intolerance to other drugs.
- Supportive Therapy:
- Oral rehydration solutions to manage dehydration caused by diarrhea.
- Nutritional support to address malabsorption.
- Treatment of Asymptomatic Carriers:
- Recommended in high-risk settings to prevent transmission (e.g., daycare centers).
- Prevention of Resistance:
- Avoid overuse of antiparasitic drugs; follow proper dosing regimens.
Prevention and Control
Preventing giardiasis requires a combination of personal hygiene, sanitation, and environmental interventions:
- Hygiene practices:
- Handwashing with soap, especially after using the toilet and before eating.
- Water safety:
- Boil or filter drinking water, especially in endemic areas or during outdoor activities.
- Food safety:
- Wash raw fruits and vegetables thoroughly.
- Public health measures:
- Improved sanitation and wastewater management.
- Education campaigns to raise awareness about giardiasis transmission.