Introduction
Actinomyces are a group of filamentous, gram-positive, non-acid-fast, facultative anaerobic (or microaerophilic) bacteria that are part of the normal flora of the human oral cavity, gastrointestinal tract, and female genital tract. While generally nonpathogenic in healthy individuals, Actinomyces species can cause actinomycosis, a chronic, suppurative infection characterized by the formation of abscesses, draining sinus tracts, and sulfur granules.
Key Characteristics:
-
-
- Gram-positive, branching filaments resembling fungi.
- Commonly associated species: Actinomyces israelii, Actinomyces naeslundii, Actinomyces odontolyticus.
-
Epidemiology
-
- Global Distribution:
- Actinomyces infections occur worldwide and are not limited to specific geographic regions.
- Reservoir:
- Normal oral cavity flora, gastrointestinal tract, and female genital tract.
- Mode of Transmission:
- Not contagious; infection occurs due to disruption of mucosal barriers (e.g., trauma, surgery, dental procedures).
- At-Risk Populations:
- Poor dental hygiene and advanced dental disease.
- Trauma or surgical procedures (e.g., tooth extraction, IUD use).
- Immunocompromised individuals.
- Incidence:
- Rare but underreported due to its slow progression and nonspecific clinical features.
- Global Distribution:
Pathogenesis
-
- Disruption of Mucosal Barriers:
- Trauma or surgical procedures allow Actinomyces species to invade deeper tissues.
- Chronic Suppurative Infection:
- Once in deeper tissues, the bacteria proliferate, forming abscesses surrounded by fibrotic tissue.
- Sinus Tract Formation:
- Chronic inflammation leads to the development of sinus tracts that discharge sulfur granules (yellowish aggregates of bacterial colonies).
- Immune Evasion:
- Actinomyces species evade host defenses by walling off infections within a fibrous tissue, leading to a chronic indolent course.
- Spread:
- The infection can spread contiguously to adjacent tissues and rarely disseminates hematogenously.
- Disruption of Mucosal Barriers:
Clinical Manifestations
Actinomycosis is classified based on the site of infection:
- Cervicofacial Actinomycosis (Most Common)
-
- Presentation:
- Swelling, indurated masses along the jaw (“lumpy jaw”), with draining sinuses.
- Associated with poor dental hygiene, dental trauma, or procedures.
- Presentation:
- Thoracic Actinomycosis
-
- Presentation:
- Chest pain, fever, cough, and weight loss.
- It may mimic tuberculosis or lung cancer.
- The infection spreads from the oropharynx or through aspiration.
- Presentation:
- Abdominopelvic Actinomycosis
-
- Presentation:
- Nonspecific abdominal pain, fever, weight loss, and mass formation.
- Often associated with bowel perforation, appendicitis, or IUD use.
- Presentation:
- Pelvic Actinomycosis
-
- Presentation:
- Pelvic or lower abdominal pain, vaginal discharge, or adnexal masses.
- Associated with prolonged intrauterine device (IUD) use.
- Presentation:
- Central Nervous System (CNS) Actinomycosis
-
- Presentation:
- Brain abscess, meningitis, or subdural empyema.
- Rare but severe, resulting from hematogenous spread or contiguous extension.
- Presentation:
- Cutaneous Actinomycosis
-
- Presentation:
- Localized skin and subcutaneous infections, often secondary to trauma.
- Presentation:
Laboratory Diagnosis
Accurate diagnosis is challenging due to the indolent nature of the disease and its resemblance to other infections or malignancies.
- Specimen Collection
-
- Specimens: Pus, tissue biopsy, or sulfur granules from draining sinuses.
- Avoid contamination with normal flora during collection.
- Direct Microscopy
-
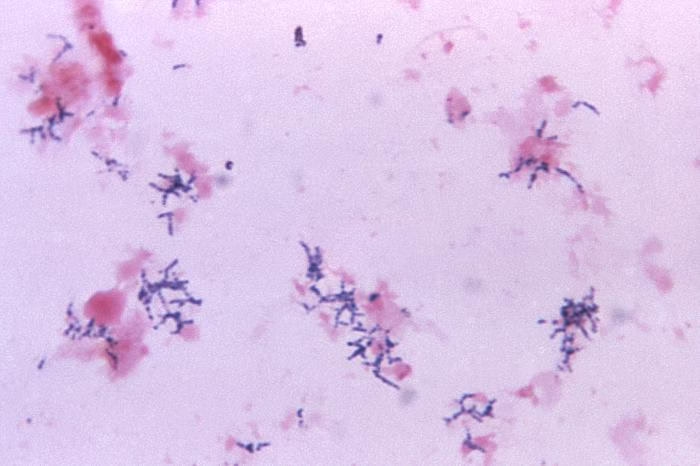
- Gram Stain:
- Filamentous, gram-positive branching rods.
- Sulfur Granules:
- Yellowish granules are visible macroscopically in pus; on microscopy, they appear as basophilic masses with peripheral clubbing of eosinophilic material.
- Gram Stain:
- Culture
-
- Media:
- Grows on enriched media such as blood agar.
- Conditions:
- Anaerobic or microaerophilic environment.
- Slow-growing, requiring 7–10 days or longer.
- Colony Morphology:
- Molar tooth appearance on solid media.
- Media:
- Histopathology
-
- Tissue biopsy shows chronic granulomatous inflammation with sulfur granules.
- Special stains like H&E, PAS, or Gomori methenamine silver may help visualize the organisms.
- Molecular Diagnostics
-
- PCR: Used for rapid detection of Actinomyces DNA, though not routinely available in many settings.
- Imaging
-
- X-rays/CT/MRI:
- Useful for identifying abscesses, sinus tracts, or bone involvement.
- Findings are nonspecific and may mimic malignancy or tuberculosis.
- X-rays/CT/MRI:
Common Species Causing Actinomycosis
-
- Actinomyces israelii (most common).
- Actinomyces naeslundii.
- Actinomyces odontolyticus.
- Actinomyces viscosus.