
The urinary system, also called the renal system, is responsible for filtering and eliminating waste products from the body while maintaining the balance of fluids and electrolytes. This system is critical in regulating essential functions like blood pressure, pH levels, and the concentration of various substances in the body, ensuring the internal environment remains stable and healthy.
Table of contents
ToggleComponents of the Urinary System:
- Kidneys: The kidneys are the primary organs of the urinary system, responsible for filtering the blood. Each kidney contains around a million functional units called nephrons, which are responsible for removing waste products, reabsorbing necessary nutrients and water, and maintaining the balance of electrolytes.
- Ureters: These tubes carry urine from the kidneys to the bladder. They use peristalsis (muscle contractions) to move urine along and prevent backflow.
- Bladder: The bladder is a hollow, muscular organ that stores urine until it’s ready to be excreted. It expands as it fills and signals the brain when it’s time to empty it.
- Urethra: The urethra is the tube that transports urine from the bladder to the outside of the body. It also plays a role in sexual function in males, as it serves as the passageway for semen.
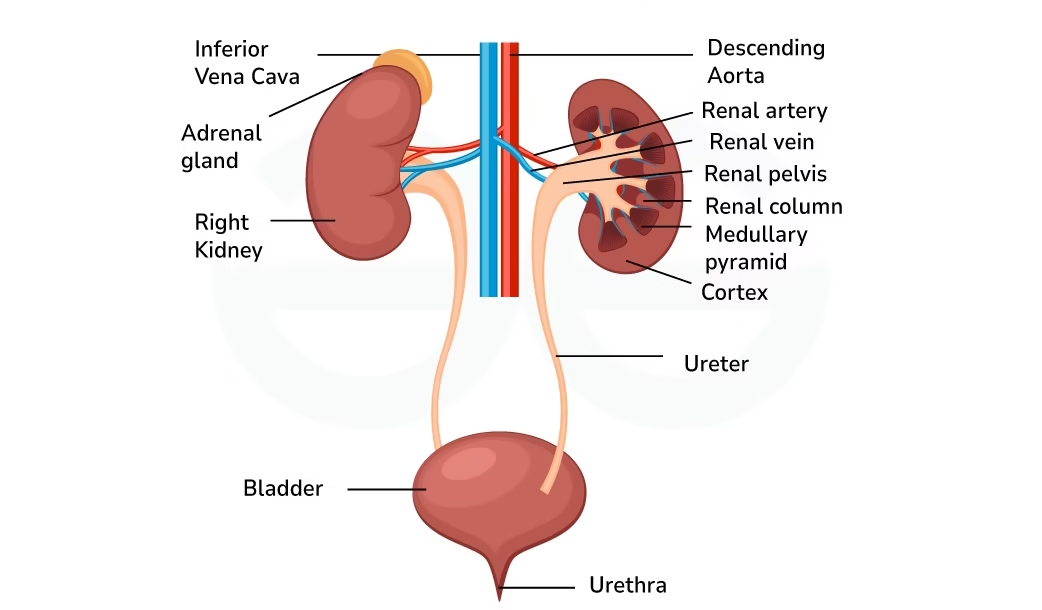
Anatomy of the Urinary System
Kidneys
The kidneys are crucial for filtering blood and excreting waste as urine. Each kidney is roughly the size of a fist and consists of several parts that work together to filter the blood and produce urine.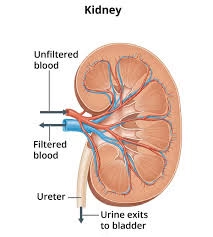
-
Location and Structure: The kidneys are located retroperitoneally (behind the abdominal cavity) on either side of the spine, with the right kidney usually positioned slightly lower than the left to accommodate the liver. A fibrous capsule surrounds each kidney, and a layer of fat (perirenal fat) surrounds this capsule, providing protection and insulation.
-
Kidney Layers:
- Renal Cortex: The outer layer of the kidney contains the renal corpuscles and most of the nephron structures (such as the proximal convoluted tubules).
- Renal Medulla: The inner region, where the renal pyramids are found. These pyramids consist of collecting ducts and loops of Henle. The medulla is responsible for creating the osmotic gradient needed for water reabsorption.
- Renal Pelvis: The funnel-shaped structure collects urine from the calyces and channels it into the ureter.
-
Nephron (Functional Unit): Each kidney contains about 1 million nephrons, and each nephron is responsible for filtering blood, reabsorbing essential nutrients, and secreting waste products. The nephron consists of:
- Renal Corpuscle: Contains the glomerulus (a knot of capillaries) and Bowman’s capsule (a cup-shaped structure that surrounds the glomerulus). Blood enters the glomerulus, and the filtration of plasma occurs, creating glomerular filtrate.
- Renal Tubule: Divided into the proximal convoluted tubule (PCT), loop of Henle, and distal convoluted tubule (DCT). The PCT reabsorbs nutrients and ions, the loop of Henle creates an osmotic gradient in the medulla, and the DCT fine-tunes reabsorption and secretion.
- Collecting Duct: Final site where water reabsorption is regulated, and urine concentration is adjusted based on the body’s needs.
-
Blood Supply to the Kidneys:
- Renal Arteries: The kidneys receive blood from the renal arteries, which branch off from the abdominal aorta. This blood carries oxygen and nutrients to the kidneys.
- Renal Veins: After filtration, blood is returned to circulation through the renal veins, which drain into the inferior vena cava.
Ureters
The ureters are muscular tubes that transport urine from the kidneys to the bladder.
- Structure: Each ureter is about 25-30 cm long and has a diameter of about 4-7 mm. The inner lining is made of transitional epithelium, allowing it to stretch as urine flows through.
- Peristalsis: The walls of the ureter contain smooth muscle that contracts in rhythmic waves called peristalsis, which helps propel urine from the kidneys to the bladder. This process is essential because the flow of urine is often against gravity.
Bladder
The bladder is a hollow, distensible organ that stores urine until excreted.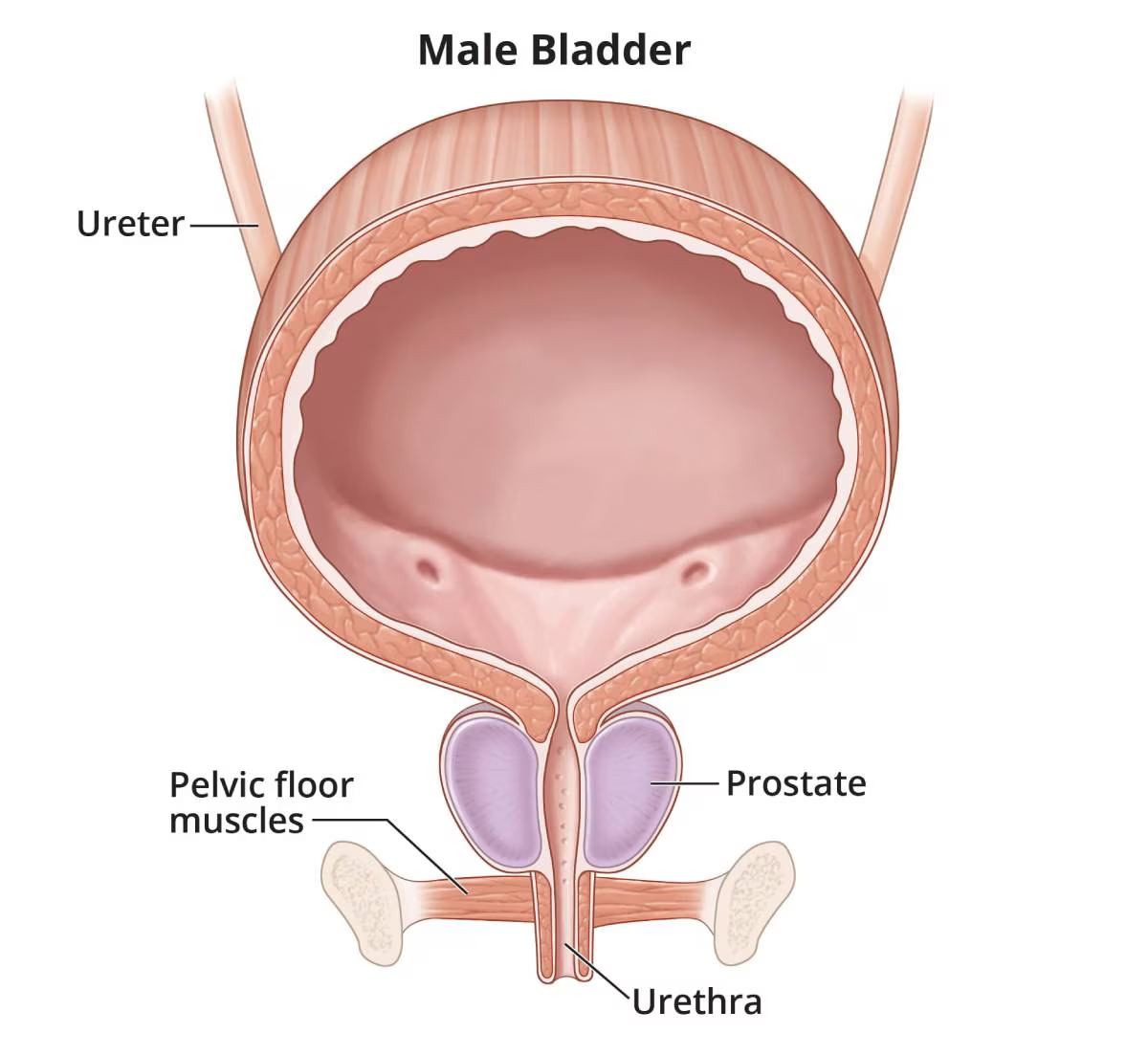
- Structure: The bladder is located in the pelvic cavity, behind the pubic bone. Its shape changes depending on its fill level, from a triangular shape when empty to a rounded shape as it fills. The bladder wall consists of smooth muscle called the detrusor muscle, which contracts to expel urine.
- Capacity: The bladder can hold approximately 300–500 mL of urine, but it can stretch to hold more if necessary.
- Internal and External Sphincters:
- Internal Urethral Sphincter: This smooth muscle sphincter is under involuntary control and prevents urine from leaking out of the bladder.
- External Urethral Sphincter: This sphincter is made of skeletal muscle and is under voluntary control, allowing us to control urination consciously.
Urethra
The urethra is the tube that carries urine from the bladder to the external environment.
- Male vs. Female Urethra: The urethra in males is about 18-20 cm long and serves as a passage for both urine and semen. In females, the urethra is about 4 cm long and is solely for the excretion of urine.
- Function: The urethra connects to the bladder and allows for the voluntary and involuntary release of urine during micturition (urination). The internal urethral sphincter contracts to prevent urine leakage, while the external sphincter is controlled consciously.
Physiology of the Urinary System
The urinary system filters blood and maintains homeostasis through several processes, including filtration, reabsorption, secretion, and excretion.
Filtration
Filtration occurs in the glomerulus of the nephron, where blood is initially filtered to remove waste products and excess substances.
-
Glomerular Filtration: Blood enters the glomerulus through the afferent arteriole under high pressure. The capillaries of the glomerulus are specialized to allow small molecules (such as water, ions, glucose, urea) to pass through, but larger molecules (like proteins and blood cells) are retained in the bloodstream.
-
Filtration Membrane: The filtration barrier consists of three layers:
- Endothelium: The inner lining of the capillaries, which has large pores that allow plasma and small solutes to pass.
- Basement Membrane: A gel-like layer that restricts the passage of larger proteins.
- Podocytes: Specialized cells that form the outer layer of the Bowman’s capsule and have foot-like extensions (pedicels) that form filtration slits to regulate what passes into the filtrate.
-
The product of filtration is called glomerular filtrate, which contains water, electrolytes, glucose, and waste products.
Reabsorption
After filtration, the renal tubules selectively reabsorb vital substances back into the bloodstream to maintain homeostasis.
- Proximal Convoluted Tubule (PCT): The PCT is responsible for the majority of reabsorption. Around 65–70% of the filtrate’s water and 100% of glucose and amino acids are reabsorbed here. Additionally, sodium, chloride, and bicarbonate are reabsorbed in varying amounts.
- Loop of Henle: The loop is key for concentrating urine and establishing the osmotic gradient in the kidney medulla. The descending limb is permeable to water but not solutes, leading to water reabsorption. The ascending limb is impermeable to water but actively pumps sodium and chloride out, creating a concentration gradient.
- Distal Convoluted Tubule (DCT): The DCT further fine-tunes electrolyte balance by reabsorbing sodium and calcium, under the influence of hormones such as aldosterone and parathyroid hormone.
- Collecting Duct: The final site for water reabsorption, which is regulated by antidiuretic hormone (ADH). ADH increases water permeability in the collecting duct, leading to more concentrated urine during dehydration.
Secretion
Secretion is when the kidneys actively transport substances from the blood into the renal tubules to be excreted in urine.
- Substances Secreted:
- Hydrogen ions (H+): Secretion of hydrogen ions helps regulate blood pH by excreting excess acid.
- Potassium (K+): Potassium is secreted into the tubules, especially under the influence of aldosterone, to maintain electrolyte balance.
- Ammonium (NH4+): In response to acid-base imbalances, the kidneys excrete ammonium ions to help maintain pH balance.
- Drugs and Toxins: Certain medications and metabolic waste products that were not filtered initially may be secreted by the kidneys into the urine for excretion.
Excretion
Excretion refers to the removal of waste and excess substances from the body in the form of urine.
- Urine Composition: After the processes of filtration, reabsorption, and secretion, the final urine contains waste products like urea, creatinine, and uric acid, as well as excess ions like sodium, potassium, and chloride, depending on the body’s needs.
- Urine Concentration: The kidneys can concentrate urine under the influence of ADH, which promotes water reabsorption in the collecting duct, making the urine more concentrated during dehydration.
Regulation and Hormonal Control
Renin-Angiotensin-Aldosterone System (RAAS)
- The RAAS is activated when blood pressure or sodium levels drop. Renin, an enzyme released from specialized cells in the juxtaglomerular apparatus of the kidneys, converts angiotensinogen (from the liver) into angiotensin I, which is then converted to angiotensin II in the lungs by the enzyme ACE.
- Angiotensin II:
- Constricts blood vessels (vasoconstriction) to increase blood pressure.
- Stimulates aldosterone release from the adrenal glands, increasing sodium and water reabsorption in the kidneys.
- Increases thirst and fluid intake, further boosting blood volume and pressure.
Antidiuretic Hormone (ADH)
- ADH, also known as vasopressin, is produced by the hypothalamus and released by the pituitary gland. It regulates water balance by acting on the kidneys to increase water reabsorption in the collecting ducts.
- In dehydration, ADH release increases, reabsorbing more water, resulting in concentrated urine. Conversely, low ADH results in diluted urine.
Atrial Natriuretic Peptide (ANP)
- ANP is released by the heart when blood volume is high. It inhibits sodium reabsorption in the kidneys, promoting the excretion of sodium and water, which leads to a decrease in blood volume and blood pressure.
Functions of the Urinary System
- Excretion of Waste Products: The kidneys filter waste products like urea (from protein metabolism), creatinine (from muscle metabolism), and uric acid (from nucleic acid metabolism). These wastes are excreted in the urine.
- Regulation of Blood Volume and Pressure: The kidneys help maintain optimal blood pressure and volume by adjusting water and sodium reabsorption, influenced by hormones like aldosterone and ADH.
- Electrolyte Balance: The kidneys regulate electrolytes (like sodium, potassium, calcium) by selectively reabsorbing or excreting them as needed.
- Acid-Base Balance: The kidneys help maintain the pH of the blood by excreting hydrogen ions (acid) and reabsorbing bicarbonate ions (base), which buffers the blood’s pH.
- Detoxification: The kidneys also filter and excrete drugs, metabolic byproducts, and toxins, contributing to the body’s detoxification processes.