General features of the histology of bones
- Bone is a specialised connective tissue enriched with inorganic salts, making it rigid and hard.
- It is dynamic and constantly remodels throughout life in response to physical, biochemical, and hormonal changes.
- Functions:
-
Supports body weight
-
Provides muscle and tendon attachment for movement
-
Acts as a reservoir for minerals like calcium and phosphorus
-
Protects vital organs
-
Contains bone marrow, which produces blood cells
-
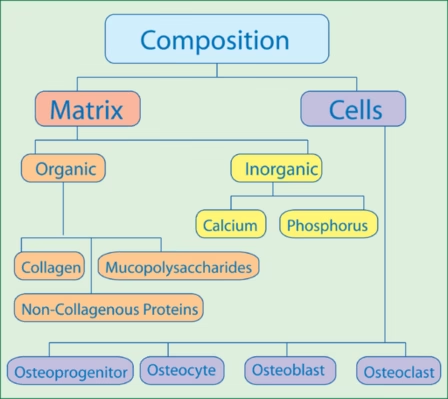
Composition of bone tissue
Cells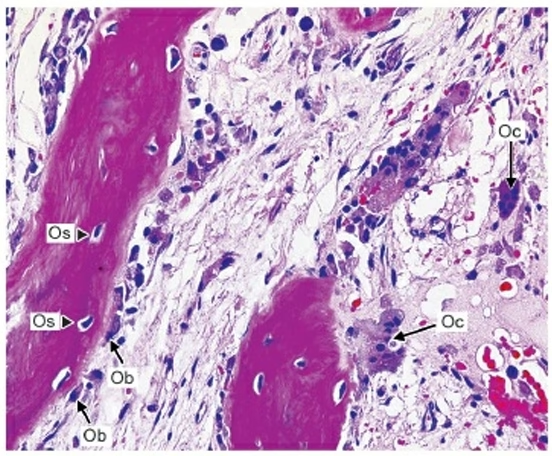
Osteoprogenitor cells
-
Osteoprogenitor cells are stem cells that come from mesenchymal tissue.
-
They can turn into osteoblasts (bone-forming cells) when needed.
-
They look like fibroblasts.
-
In the fetus, they are found in areas where bones are forming.
-
In adults, they are located on the surface of bones (both periosteal and endosteal surfaces).
Osteoblasts
-
Osteoblasts are bone-forming cells responsible for producing new bone tissue.
-
They originate from osteoprogenitor cells and become active when new bone needs to be created.
-
Osteoblasts produce and secrete an organic matrix made up of collagen and other proteins, which later mineralise to form bone.
-
Once they complete their bone-forming task, some osteoblasts become trapped in the matrix and turn into osteocytes.
-
They play a key role in bone growth, repair, and mineralisation.
-
Osteoblasts are found on the surface of bones, especially where new bone is being formed.
Osteocytes
-
Osteocytes are mature bone cells that maintain the bone tissue.
-
They develop from osteoblasts after they become surrounded by the bone matrix they created.
-
Osteocytes are embedded within the bone matrix and have long extensions that connect with other osteocytes, allowing them to communicate.
-
They help maintain bone strength by regulating the activity of osteoblasts and osteoclasts.
-
Osteocytes play a key role in detecting mechanical stress on bones and sending signals for bone remodelling.
-
They are the most abundant type of bone cell and are located within the bone’s lacunae (small spaces within the bone).
Osteoclasts
-
Osteoclasts are large, multinucleated cells responsible for breaking down bone tissue.
-
They play a crucial role in bone remodelling by resorbing old or damaged bone.
-
Osteoclasts secrete enzymes and acids that dissolve the mineralised bone matrix, releasing calcium and other minerals into the bloodstream.
-
These cells are derived from a different lineage than osteoblasts and osteocytes, originating from hematopoietic stem cells.
-
They are found on the surface of bone where bone resorption is occurring, often in areas of bone repair or remodelling.
-
Osteoclasts work in balance with osteoblasts to maintain healthy bone turnover and homeostasis.
Bone Lining Cells
-
Bone lining cells are flat, inactive cells that cover the surface of bones.
-
They are derived from osteoblasts and remain on the bone surface when bone formation is not occurring.
-
These cells help maintain the bone matrix and regulate the movement of minerals in and out of the bone.
-
Bone lining cells are found in both the periosteum (outer layer) and endosteum (inner layer) of bones.
-
They may also play a role in the regulation of osteoclast activity during bone remodelling.
Bone Matrix
Organic matrix
-
The organic matrix of bone, also known as osteoid, is primarily composed of collagen fibers, which provide flexibility and strength.
-
It also contains various proteins, such as osteocalcin and osteopontin, that help in bone mineralisation and cell attachment.
-
The organic matrix makes up about 30% of bone tissue and forms the scaffold for mineral deposition.
-
It plays a crucial role in the bone’s ability to resist tension and stress.
-
As bone matures, the organic matrix becomes mineralised with calcium and phosphate, forming the hard, rigid structure of bone.
Inorganic ions
-
Inorganic ions in bone primarily consist of calcium and phosphate, which combine to form hydroxyapatite crystals, giving bone its hardness and strength.
-
Calcium ions are essential for bone mineralisation and maintaining bone density.
-
Phosphate ions, in conjunction with calcium, contribute to the structure and rigidity of bones.
-
Other inorganic ions, such as magnesium, sodium, bicarbonate, and potassium, are also present in small amounts, supporting bone function and structure.
-
These ions are stored in the bone matrix and can be released into the bloodstream when needed to maintain mineral balance in the body.
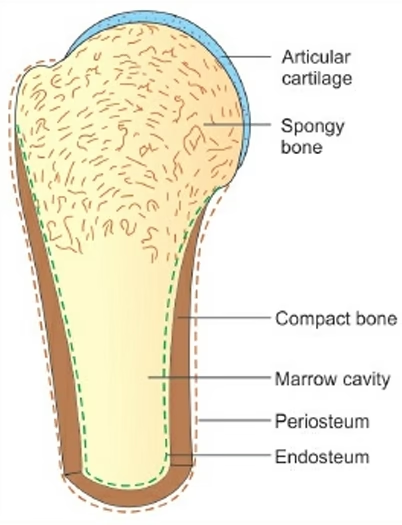
Classification and structure of bones
- Based on the gross appearance of bone: Compact bone and spongy bone.
- Based on maturity: Mature/lamellar bone and immature/ woven bone.
- Based on ossification: membranocartilaginous.
Based on the gross appearance of bone
Compact bone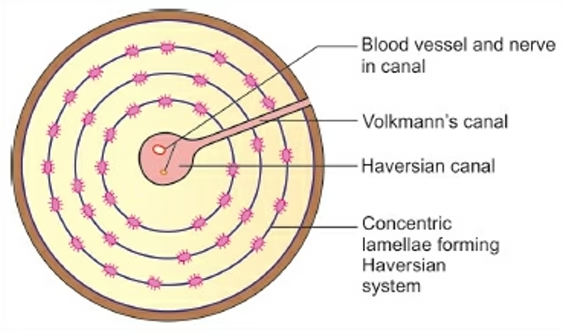
The histology of compact bone refers to its cellular and structural organisation at the microscopic level:
-
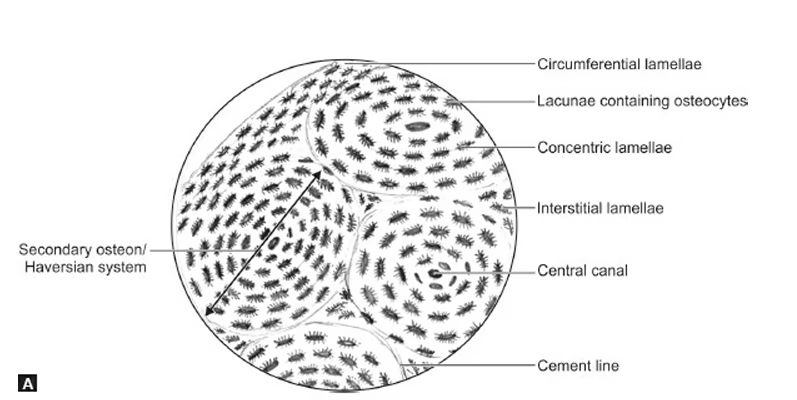
Osteons (Haversian Systems):
-
The basic functional unit of compact bone.
-
Osteons are cylindrical structures that run parallel to the bone’s long axis.
-
Each osteon consists of concentric layers of bone matrix called lamellae.
-
-
Haversian Canal:
-
The central canal within each osteon.
-
Contains blood vessels, nerves, and lymphatic vessels that supply nutrients to the bone and remove waste.
-
Also called the central canal.
-
-
Lamellae:
-
Concentric rings of bone matrix that surround the Haversian canal.
-
Lamellae are made up of collagen fibers and inorganic minerals like calcium and phosphate.
-
They provide strength and resistance to torsional forces.
-
-
Osteocytes:
-
Mature bone cells located in small spaces called lacunae within the lamellae.
-
Osteocytes maintain bone tissue and communicate with each other through tiny channels known as canaliculi.
-
-
Canaliculi:
-
Small channels that radiate from the lacunae and connect osteocytes to each other and to the Haversian canal.
-
Canaliculi allow for the exchange of nutrients and waste products between osteocytes.
-
-
Volkmann’s Canals:
-
Horizontal canals that connect adjacent Haversian canals.
-
They allow for the passage of blood vessels and nerves across the bone, ensuring the bone is well-supplied.
-
-
Interstitial Lamellae:
-
The remnants of old osteons that have been partially resorbed during bone remodeling.
-
Found between intact osteons, they help fill in gaps within the bone structure.
-
-
Perforating Fibers (Sharpey’s Fibers):
-
Collagen fibers that anchor the periosteum (bone’s outer layer) to the underlying compact bone.
-
These fibers penetrate the bone matrix and strengthen the attachment of tissues to the bone.
-
Spongy/Cancellous Bone
The histology of spongy (or cancellous) bone refers to its microscopic structure, which is more porous and less dense compared to compact bone. Here’s a breakdown of its key features: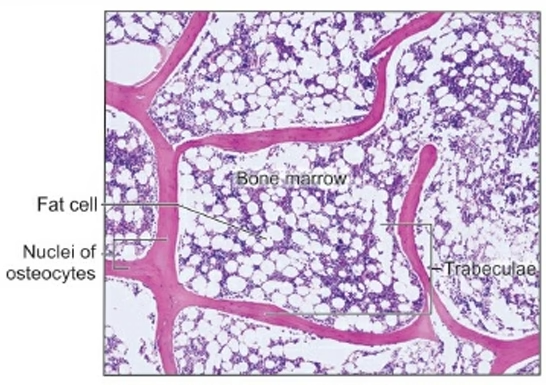
-
Trabeculae:
-
Spongy bone is made up of a network of trabeculae (thin, branching bone plates or struts).
-
The trabeculae form a lattice-like structure that provides strength while reducing the overall weight of the bone.
-
They are oriented along lines of stress to help the bone resist forces from various directions.
-
-
Bone Marrow:
-
The spaces between the trabeculae are filled with bone marrow (either red or yellow, depending on the age and type of bone).
-
Red bone marrow is involved in the production of blood cells.
-
Yellow bone marrow consists mostly of adipocytes (fat cells) and serves as a storage for fat.
-
-
Osteocytes:
-
Like compact bone, spongy bone contains osteocytes, which are mature bone cells.
-
Osteocytes are housed in small cavities called lacunae within the trabeculae.
-
These cells maintain bone tissue and communicate with each other through tiny channels called canaliculi.
-
-
Lamellae:
-
Spongy bone also has lamellae, but they are arranged in a less organized manner compared to the compact bone’s osteons.
-
Lamellae in spongy bone form thin plates or layers, and the arrangement is more irregular.
-
-
No Haversian Systems:
-
Unlike compact bone, spongy bone does not have Haversian systems (osteons).
-
Instead of central Haversian canals, spongy bone relies on diffusion through the trabecular network to nourish its cells.
-
-
Endosteum:
-
The inner surface of the trabeculae is covered by a layer of cells called the endosteum.
-
These cells are involved in the growth, repair, and remodelling of bone.
-
-
Perforating Fibers (Sharpey’s Fibers):
-
These fibers also exist in spongy bone, helping to anchor the periosteum (the outer membrane of the bone) to the bone’s surface.
-
Formation of bones
- Bone formation, or ossification, is the process by which bone tissue is created.
- There are two main types of ossification:
- Intramembranous ossification
- Endochondral ossification.
- Both processes involve several key steps, and the histology of each shows how different types of cells work together to create bone.
Intramembranous Ossification
This process occurs in flat bones, such as those of the skull, and involves the direct transformation of connective tissue (mesenchyme) into bone.
Steps in Intramembranous Ossification:
-
Mesenchymal Cells Differentiate:
-
Mesenchymal cells (undifferentiated cells) gather in certain areas where bone is to form.
-
These cells change into osteoblasts, the bone-forming cells.
-
-
Osteoid Secretion:
-
Osteoblasts start producing a soft, unmineralized bone matrix called osteoid.
-
The osteoid is mostly made of collagen, which gives the bone flexibility and strength.
-
-
Mineralization:
-
The osteoid becomes mineralized as calcium and phosphate crystals form, hardening the osteoid into solid bone tissue.
-
-
Formation of Trabeculae:
-
As more osteoid is secreted and mineralized, small struts or plates of bone form, called trabeculae.
-
These trabeculae form the inner part of the bone, also known as spongy bone or cancellous bone.
-
-
Periosteum Formation:
-
The outer surface of the bone becomes covered by a layer of connective tissue called the periosteum.
-
This layer contains osteoblasts that continue to add new bone on the surface.
-
-
Compact Bone Formation:
-
Eventually, the trabecular bone is remodelled, and some of it becomes compact bone, which is dense and forms the outer layer of the bone.
-
Endochondral Ossification
This process occurs in most bones of the body, especially long bones like the femur and tibia, and involves the replacement of cartilage with bone.
Steps in Endochondral Ossification:
-
Formation of Cartilage Model:
-
Initially, the developing bone is made of hyaline cartilage.
-
Mesenchymal cells differentiate into chondrocytes (cartilage cells), which form a cartilage model of the bone.
-
-
Cartilage Growth and Hypertrophy:
-
The cartilage grows through a process called interstitial growth (expansion from within) and appositional growth (growth from the surface).
-
The chondrocytes in the center of the cartilage model start to hypertrophy (enlarge) and the surrounding matrix begins to calcify (harden).
-
-
Blood Vessel Invasion:
-
Blood vessels begin to invade the center of the cartilage model, bringing osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells).
-
This area becomes the primary ossification center where bone starts replacing cartilage.
-
-
Bone Formation in the Diaphysis:
-
Osteoblasts lay down the osteoid, which is mineralized to form bone tissue.
-
The cartilage in the center is replaced by bone, and a hollow space called the medullary cavity forms in the middle of the diaphysis (shaft).
-
-
Formation of Secondary Ossification Centers:
-
After birth, secondary ossification centers form in the epiphyses (ends) of the bones.
-
Bone formation continues in these areas, but the center of the epiphysis remains cartilage, forming the epiphyseal plate (growth plate).
-
-
Epiphyseal Plate:
-
The epiphyseal plate allows the bone to grow in length during childhood and adolescence. As the body matures, the cartilage in this plate is replaced by bone, and the growth plate closes.
-
-
Mature Bone:
-
As the ossification process completes, the bone is fully formed, and the periosteum and endosteum (inner bone lining) help maintain the bone structure.
-
Applied Histology
Bone Disease Diagnosis
-
Osteoporosis:
-
Histology helps diagnose osteoporosis, a condition where bones become weak and brittle. By looking at bone samples under a microscope, doctors can observe thinning of the bone structure, a decrease in bone density, and a loss of trabeculae (the tiny bone struts in spongy bone).
-
This helps determine how severe the disease is and guide treatment options.
-
-
Bone Cancer (Osteosarcoma):
-
Histological examination of bone tissue can help identify osteosarcoma, a type of bone cancer. Abnormal, cancerous bone cells are often seen with irregular shapes and unorganized growth patterns in tissue samples.
-
This helps in identifying the type of cancer, its stage, and the best course of treatment.
-
-
Paget’s Disease:
-
In Paget’s disease of bone, histology can show excessive bone breakdown followed by abnormal bone formation, leading to weak and misshapen bones. Examining bone samples can reveal the areas where bone remodeling is too rapid.
-
Bone Repair and Regeneration
-
Fracture Healing:
-
Histology is used to study the healing process of fractured bones. In the early stages, fibrocartilage forms around the break, and over time, it is replaced by bone through a process called ossification.
-
Understanding how bone heals at the cellular level helps in developing better treatments for bone fractures, including bone grafts or stem cell therapy.
-
-
Bone Grafting and Tissue Engineering:
-
Histology is important in developing bone grafts (from a donor or synthetic bone) to repair large bone defects. By studying how bone cells grow and integrate into the graft, researchers can improve bone healing.
-
In bone tissue engineering, histology is used to assess how effectively lab-grown tissues form functional bone.
-
Bone Development and Growth
-
Bone Growth in Children and Adolescents:
-
Histological studies of epiphyseal plates (growth plates) in growing children help doctors understand how bones lengthen during growth. The epiphyseal plate is made of cartilage, and histology can reveal how it gradually turns into bone, allowing bones to grow.
-
Understanding this process can help diagnose growth-related issues such as dwarfism or gigantism, where growth plate function is abnormal.
-
-
Congenital Bone Disorders:
-
Histology is used to understand genetic bone disorders like osteogenesis imperfecta (brittle bone disease) and achondroplasia (a form of dwarfism). Microscopic examination of bones from these patients shows abnormal bone formation or structure, aiding in diagnosis.
-
Monitoring Bone Health in Older Adults
-
Osteoarthritis:
-
In osteoarthritis, histology can show the breakdown of cartilage in the joints and the formation of abnormal bone growth. This helps doctors track how the disease progresses and how well treatments are working.
-
Histology can reveal bone spurs or subchondral sclerosis (thickening of the bone beneath cartilage), common in osteoarthritis.
-
-
Osteomalacia:
-
This is a condition where bones become soft due to vitamin D deficiency. Histology of bone tissue shows increased unmineralized osteoid and abnormal bone structure. This helps doctors treat the underlying cause, often through vitamin D supplementation.
-
Bone Infections and Inflammation
-
Osteomyelitis:
-
Osteomyelitis is a bone infection, usually caused by bacteria. Histology can show the presence of pus or abscesses in bone tissue, as well as the breakdown of bone material.
-
This helps in identifying the infection and determining the best treatment, such as antibiotics or surgery.
-
-
Bone Inflammation:
-
Inflammatory conditions like rheumatoid arthritis can affect bones. Histology helps to examine the synovium (lining of joints) and the periosteum (outer layer of bone) to identify signs of chronic inflammation and bone erosion, providing clues to the disease’s progression.
-
Bone Aging and Remodeling
-
Bone Remodeling in Aging:
-
Bone remodeling is the process by which old bone is replaced with new bone tissue. This process slows down with age. Histology allows us to study how bone density and structure change in older adults.
-
In conditions like osteoporosis, histology can reveal how osteoclasts (cells that break down bone) become overactive, leading to a loss of bone mass and making bones more fragile.
-
-
Monitoring Bone Changes During Hormonal Changes:
-
Histology is used to study how hormones like estrogen (in women) and testosterone (in men) affect bone structure. For example, after menopause, women experience a decrease in estrogen, leading to bone loss. Histology can reveal changes in bone density and structure during these hormonal shifts.
-
Forensic Analysis
-
Forensic Histology of Bones:
-
In forensic science, histology is used to examine bone tissue in cases of suspected trauma, such as fractures from accidents or violence. Histology can reveal healed fractures, trauma-induced changes, or signs of bone disease that may have contributed to a person’s death.
-
Histology also helps determine age estimation from bones in cases where the identity of a deceased person is unknown.
-
Bone Biopsy in Disease Diagnosis
-
Bone Marrow Biopsy:
-
A bone marrow biopsy, often taken from the hip bone, is analyzed using histology to diagnose conditions like leukemia, lymphoma, or anemia. Histological examination of the bone marrow can show the presence of abnormal cells or deficiencies in blood cell production.
-