
Purpura Disease
- Purpura refers to the appearance of purple or red spots on the skin or mucous membranes caused by bleeding underneath the skin.
- The bleeding occurs when small blood vessels, particularly capillaries, rupture and allow blood to leak into surrounding tissues.
- Purpura can manifest in various forms, from tiny pinpoint spots called petechiae to larger areas of bruising known as ecchymosis.
- These bleeding spots can appear on the skin, mucous membranes (mouth, nose, gastrointestinal tract), or internal organs.
- Purpura itself is not a diagnosis, but rather a clinical sign of an underlying condition that requires further investigation.
Types of Purpura
Purpura is classified into two main categories, based on platelet count and the underlying cause:
Thrombocytopenic Purpura
In this type of purpura, the platelet count is abnormally low, impairing the ability to form clots and increasing the risk of bleeding. Thrombocytopenic purpura can be caused by various conditions, including autoimmune diseases, clotting factor deficiencies, and certain drug reactions.
Key Forms:
-
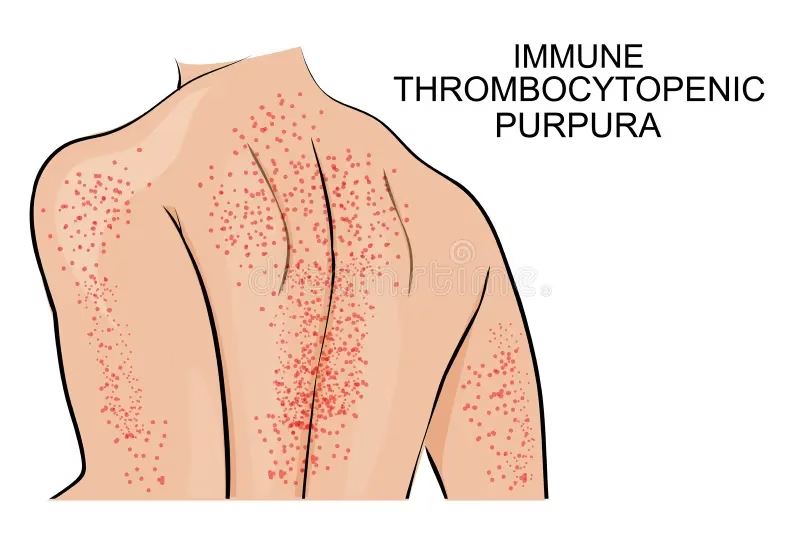
Immune Thrombocytopenic Purpura (ITP):
-
ITP is an autoimmune disorder where the immune system mistakenly attacks and destroys platelets. The condition is characterised by a low platelet count, resulting in an increased risk of bleeding and purpura.
-
Acute ITP is commonly seen in children and often follows viral infections (e.g., chickenpox, rubella).
-
Chronic ITP is more common in adults and can last for months or years. It is often associated with autoimmune disorders such as lupus or other systemic conditions.
-
Symptoms of ITP include easy bruising, petechiae (tiny red spots), heavy or prolonged bleeding from minor cuts, and spontaneous bleeding (nosebleeds, gum bleeding).
-
-
Thrombotic Thrombocytopenic Purpura (TTP):
-
TTP is a life-threatening condition characterized by small blood clots forming in blood vessels throughout the body, which consume platelets, leading to thrombocytopenia.
-
It is caused by a deficiency of the enzyme ADAMTS13, which is involved in the breakdown of von Willebrand factor (vWF), a protein involved in clotting. Without enough ADAMTS13, large vWF multimers cause excessive platelet aggregation, leading to clot formation and platelet depletion.
-
TTP often presents with a combination of purpura, hemolytic anemia (destruction of red blood cells), kidney failure, neurological symptoms (confusion, seizures), and fever.
-
TTP is a medical emergency and requires plasma exchange (plasmapheresis), which replaces the missing enzyme and removes the harmful antibodies.
-
-
Heparin-Induced Thrombocytopenia (HIT):
-
HIT occurs in patients treated with heparin, an anticoagulant medication. In this condition, antibodies form against a complex of heparin and platelet factor 4, which leads to platelet activation, increased clotting, and thrombocytopenia.
-
It may present with purpura at the injection site and other signs of thrombosis (e.g., deep vein thrombosis, pulmonary embolism).
-
Management includes discontinuation of heparin and the use of alternative anticoagulants (e.g., argatroban).
-
Non-Thrombocytopenic Purpura
In this form, the platelet count is typically normal, but purpura occurs due to abnormal blood vessel integrity, clotting factor deficiencies, or other systemic conditions that cause bleeding.
Key Forms:
-
Vasculitis:
-
Vasculitis is the inflammation of blood vessels that weakens their walls, making them prone to rupture and leakage of blood into surrounding tissues. Vasculitis can be classified as large vessel (e.g., temporal arteritis), medium vessel (e.g., polyarteritis nodosa), or small vessel (e.g., Henoch-Schönlein purpura).
-
Common vasculitides associated with purpura include:
-
Henoch-Schönlein Purpura (HSP): A small vessel vasculitis that typically affects children, often following an upper respiratory infection. It is characterized by purpura on the legs and buttocks, abdominal pain, joint pain (arthritis), and kidney involvement (glomerulonephritis).
-
Polyarteritis Nodosa (PAN): A systemic vasculitis that affects medium-sized arteries, often causing purpura, skin ulcers, abdominal pain, and muscle weakness. PAN can lead to renal and cardiac complications.
-
-
-
Scurvy:
-
Scurvy is caused by a vitamin C deficiency, which impairs collagen synthesis and weakens the blood vessel walls. This leads to easy bruising, bleeding gums, joint pain, and purpura.
-
Other symptoms of scurvy include fatigue, poor wound healing, and anemia.
-
The treatment for scurvy involves vitamin C supplementation.
-
-
Drug-Induced Purpura:
-
Certain medications can cause purpura through their effects on platelets or blood vessels. Common drugs include:
-
Corticosteroids: Long-term use can weaken blood vessels.
-
Anticoagulants: Drugs like warfarin or heparin can impair clotting and increase bleeding risk.
-
Chemotherapy drugs: These can suppress bone marrow production of platelets, leading to purpura.
-
-
-
Leukemia:
-
Leukemia, a cancer of the blood and bone marrow, can present with purpura due to reduced platelet production in the bone marrow or due to the abnormal white blood cells affecting the blood vessels.
-
Symptoms include purpura, fatigue, paleness, and infections.
-
Symptoms of Purpura
The most common symptom of purpura is the appearance of purplish or red spots on the skin. The symptoms may vary based on the underlying cause, but common features include:
-
Petechiae: Tiny, pinpoint red or purple spots that do not blanch when pressed.
-
Ecchymosis: Larger areas of bruising (often associated with trauma) that can appear as purplish-blue discolorations.
-
Purpuric Rash: Larger, irregular patches of purpura, usually seen on the lower limbs.
-
Spontaneous Bleeding: Bleeding from the gums, nosebleeds, or blood in the stool or urine.
-
Fatigue: Often seen in association with anemia or severe inflammation.
-
Pain and Swelling: In conditions like HSP or PAN, purpura may be associated with joint pain and swelling.
Laboratory Diagnosis
A comprehensive diagnostic workup is essential to determine the underlying cause of purpura. The key tests include:
1. Complete Blood Count (CBC)
-
Platelet Count: A low platelet count is indicative of thrombocytopenic purpura (e.g., ITP, TTP), while a normal count suggests a non-thrombocytopenic cause (e.g., vasculitis, scurvy).
-
Hemoglobin and Hematocrit: To assess for anemia that may occur due to blood loss or hemolysis.
-
White Blood Cell Count (WBC): Elevated levels may point to an infection or inflammatory process.
2. Peripheral Blood Smear
-
The peripheral smear can help evaluate abnormal blood cells:
-
In ITP, large platelets may be present.
-
In TTP, fragmented red blood cells (schistocytes) may indicate microangiopathic hemolysis.
-
In leukemia, abnormal white blood cells can be seen.
-
3. Coagulation Studies
-
Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT) are tests to evaluate clotting ability. Prolonged PT or aPTT can indicate a clotting factor deficiency, such as in DIC or liver disease.
-
D-dimer: Elevated in conditions like DIC where there is both clotting and bleeding.
4. Bone Marrow Biopsy
-
Bone marrow biopsy may be required if there is suspicion of bone marrow failure (e.g., leukemia, aplastic anemia).
5. Autoimmune Tests
-
Antiplatelet Antibodies: In autoimmune conditions like ITP, antibodies targeting platelets may be present.
-
Antinuclear Antibody (ANA): Elevated levels suggest systemic lupus erythematosus (SLE) or other autoimmune diseases that could cause vasculitis.
6. Specific Tests for TTP
-
ADAMTS13 Activity: A deficiency in ADAMTS13 is a diagnostic marker for TTP.
7. Infection Workup
-
Blood cultures, urine cultures, or other tests to identify infections like meningococcal infections that can lead to purpura.
Treatment and Management
The treatment of purpura depends entirely on its underlying cause. The main goals are to manage the bleeding and treat the root cause of the condition.
1. Treatment of Thrombocytopenic Purpura (Low Platelet Count)
-
Immune Thrombocytopenic Purpura (ITP):
-
Corticosteroids (e.g., prednisone) are used to suppress the immune system and increase platelet count.
-
Intravenous Immunoglobulin (IVIg): A more effective therapy in severe cases, where the immune system attacks platelets.
-
Splenectomy: In cases of chronic ITP that do not respond to medication, removal of the spleen may be considered as the spleen is responsible for platelet destruction.
-
-
Thrombotic Thrombocytopenic Purpura (TTP):
-
Plasmapheresis (plasma exchange): This is the first-line treatment for TTP, removing autoantibodies and replenishing ADAMTS13 enzyme levels.
-
Steroids and immunosuppressive agents (e.g., cyclophosphamide) may be used in more severe cases.
-
-
Heparin-Induced Thrombocytopenia (HIT):
-
Discontinuation of heparin and switching to a non-heparin anticoagulant like argatroban or fondaparinux.
-
2. Treatment of Non-Thrombocytopenic Purpura
-
Vasculitis:
-
Corticosteroids to reduce inflammation, and immunosuppressive drugs (e.g., cyclophosphamide, methotrexate) for more severe or systemic vasculitis.
-
-
Scurvy:
-
Vitamin C supplementation is the mainstay of treatment.
-
-
Drug-Induced Purpura:
-
Discontinuation of the causative drug is critical, followed by supportive treatment (e.g., corticosteroids or IVIg for more severe cases).
-
3. Supportive Management
-
Blood Transfusions may be needed in cases of significant bleeding or anemia.
-
Pain management and wound care to manage bleeding or bruising.
-
Monitoring organ function (especially in TTP, PAN, or vasculitis) to detect complications early.
