Introduction
-
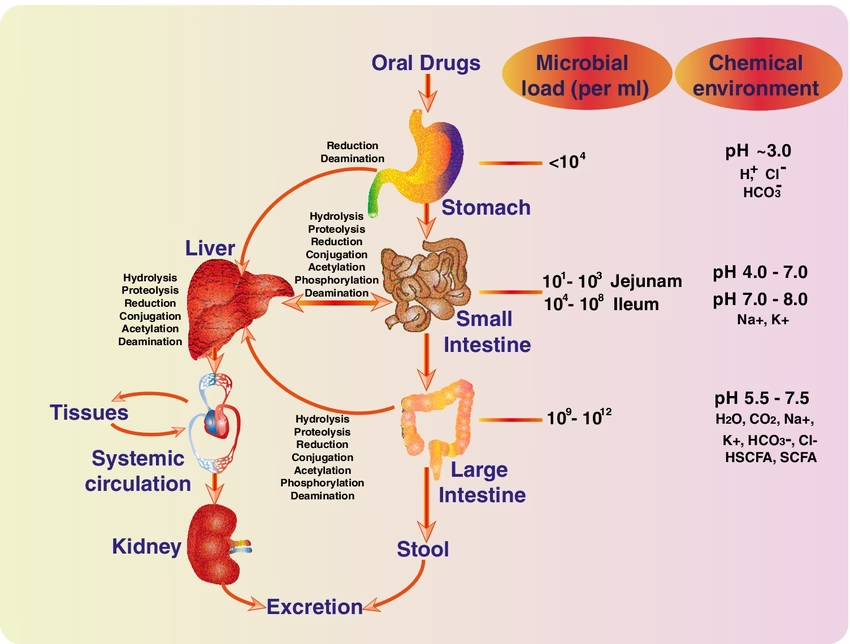
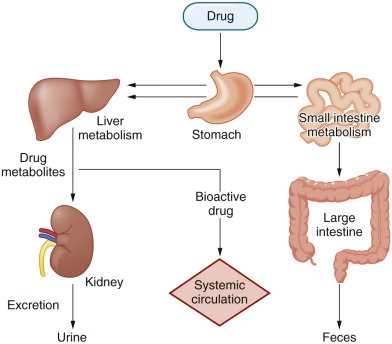
Liver
-
Principal and most important site of xenobiotic metabolism
-
Rich in microsomal and non-microsomal enzymes
-
Contains Cytochrome P450 enzyme system
-
Responsible for both Phase I and Phase II reactions
-
-
Kidneys
-
Involved in biotransformation and excretion of xenobiotics
-
Play an important role in water-soluble drug elimination
-
Some drugs undergo metabolic modification before excretion
-
-
Intestinal Mucosa
-
Contributes to first-pass metabolism of orally administered drugs
-
Contains metabolic enzymes similar to liver
-
Influences bioavailability of drugs
-
-
Lungs
-
Important for metabolism of volatile and gaseous substances
-
Rich in oxidizing enzymes
-
Major site for inhaled xenobiotics
-
-
Skin
-
Minor site of xenobiotic metabolism
-
Involved in detoxification of topically applied chemicals
-
-
Plasma (Blood)
-
Contains enzymes capable of hydrolysis of ester drugs
-
Plays a limited but significant role in drug metabolism
-
-
Other Tissues
-
Brain, placenta, and adrenal glands show limited metabolic activity
-
Important in local detoxification and protection
-
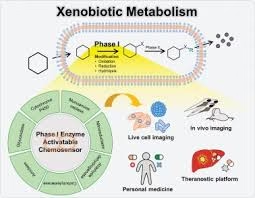
Phases of Xenobiotic Metabolism
Xenobiotic metabolism occurs in two major phases, often followed by a transport step (Phase III).
Phase I Reactions (Functionalization Reactions)
-
Phase I reactions are the first step in xenobiotic metabolism.
-
These reactions introduce or expose functional groups such as –OH, –NH₂, –COOH, or –SH on the xenobiotic molecule.
-
The main purpose is to increase chemical reactivity and prepare the compound for Phase II conjugation.
-
Phase I reactions may increase, decrease, or not change the toxicity of the xenobiotic.
-
Most Phase I reactions occur in the smooth endoplasmic reticulum of liver cells.
Major Types of Phase I Reactions
1. Oxidation (Most common)
-
Catalyzed mainly by Cytochrome P450 (CYP450) enzymes
-
Occurs in microsomes (SER)
Examples:
-
Hydroxylation (–OH addition)
-
N-dealkylation
-
O-dealkylation
-
Deamination
-
Sulfoxidation
Example reaction:
Benzene → Phenol
2. Reduction
-
Occurs under low oxygen conditions
-
Less common than oxidation
Examples:
-
Reduction of nitro (–NO₂) to amino (–NH₂)
-
Reduction of azo compounds
3. Hydrolysis
-
Catalyzed by esterases and amidases
-
Breaks ester or amide bonds
Examples:
-
Procaine → PABA + diethylaminoethanol
-
Aspirin → salicylic acid + acetic acid
Enzyme System
-
Cytochrome P450 monooxygenase system
-
Requires NADPH and molecular oxygen (O₂)
-
Found mainly in microsomes of hepatocytes
Examples of Phase I Reactions
-
Hydroxylation of aromatic compounds
-
Dealkylation of drugs
-
Reduction of nitro and azo compounds
-
Hydrolysis of ester and amide bonds
Clinical Significance
-
Responsible for drug activation or inactivation
-
Can generate reactive and toxic intermediates
-
Plays a key role in drug–drug interactions and chemical carcinogenesis
Phase II Reactions (Conjugation Reactions)
-
Phase II reactions are the second and major detoxification step in xenobiotic metabolism.
-
These reactions involve conjugation of xenobiotics or their Phase I metabolites with endogenous, polar molecules.
-
The primary aim is to increase water solubility and facilitate rapid excretion.
-
Phase II reactions usually reduce or abolish biological activity and toxicity.
-
Reactions occur mainly in the cytosol and partly in microsomes of liver cells.
Major Conjugation Reactions
1. Glucuronidation
-
Most important conjugation reaction
-
Occurs in liver microsomes
Conjugating agent: UDP-glucuronic acid
Enzyme: UDP-glucuronyl transferase
Substrates:
-
Bilirubin
-
Steroid hormones
-
Drugs (morphine, paracetamol)
2. Sulfation
-
Occurs in cytosol
-
High-affinity, low-capacity pathway
Conjugating agent: PAPS (3′-phosphoadenosine-5′-phosphosulfate)
3. Acetylation
-
Occurs in cytosol
-
Catalyzed by N-acetyl transferase
Clinical importance:
-
Genetic variation → slow and fast acetylators
-
Example drugs: Isoniazid, sulfonamides
4. Methylation
-
Does NOT increase water solubility significantly
-
Important for inactivation
Methyl donor: S-adenosyl methionine (SAM)
5. Glutathione Conjugation
-
Protective mechanism against toxic electrophiles
-
Enzyme: Glutathione-S-transferase (GST)
Clinical relevance:
-
Paracetamol toxicity
-
Depletion of glutathione causes liver damage
6. Amino Acid Conjugation
-
Conjugation with glycine, glutamine, taurine
Example:
-
Benzoic acid → Hippuric acid
Common Conjugating Agents
-
UDP-glucuronic acid
-
PAPS (3′-phosphoadenosine-5′-phosphosulfate)
-
Acetyl-CoA
-
S-adenosyl methionine (SAM)
-
Glutathione (GSH)
-
Glycine, taurine, glutamine
Phase III (Transport and Excretion)
-
Phase III represents the final step of xenobiotic detoxification, involving active transport and elimination of metabolites.
-
It mainly handles Phase II–conjugated xenobiotics, which are large and highly polar.
-
Transport across cell membranes requires energy-dependent carrier proteins.
-
These reactions do not chemically modify the xenobiotic but facilitate its removal from the body.
Major Transport Systems
-
ATP-binding cassette (ABC) transporters
-
P-glycoprotein (MDR transporter)
-
Multidrug resistance–associated proteins (MRPs)
Routes of Excretion
-
Urine (renal excretion)
-
Major route for small, water-soluble conjugates
-
-
Bile (hepatic excretion)
-
Large conjugated metabolites
-
-
Feces
-
Eliminated via bile into intestine
-
-
Sweat, saliva, breast milk
-
Minor routes
-
-
Expired air
-
Volatile substances
-
Clinical Significance
-
Determines duration of drug action
-
Plays a role in drug resistance (e.g., cancer chemotherapy)
-
Impairment leads to accumulation and toxicity
-
Important in drug–drug interactions
Fate of Xenobiotics
-
After undergoing Phase I and Phase II metabolism, xenobiotics are converted into water-soluble metabolites.
-
The ultimate fate of xenobiotics is their elimination from the body through various excretory routes.
Major Routes of Elimination
-
Urinary Excretion
-
Most common route
-
Water-soluble and low-molecular-weight compounds
-
Excreted via glomerular filtration and tubular secretion
-
-
Biliary Excretion
-
Large, polar conjugates (e.g., glucuronides)
-
Excreted into bile and eliminated in feces
-
May undergo enterohepatic circulation
-
-
Fecal Excretion
-
Non-absorbed xenobiotics
-
Biliary metabolites eliminated through intestine
-
-
Pulmonary Excretion
-
Volatile substances such as anesthetic gases
-
Eliminated via expired air
-
-
Minor Routes
-
Sweat and saliva
-
Breast milk (clinically important for drug safety in infants)
-
Factors Affecting Xenobiotic Metabolism
-
Age
-
Neonates have immature enzyme systems
-
Elderly individuals show reduced metabolic capacity
-
-
Genetic Factors
-
Genetic polymorphism leads to fast and slow metabolizers
-
Influences drug response and toxicity
-
-
Nutritional Status
-
Protein deficiency reduces enzyme synthesis
-
Vitamin deficiencies (B-complex, antioxidants) impair detoxification
-
-
Liver Function
-
Liver diseases (hepatitis, cirrhosis) reduce metabolism
-
Leads to drug accumulation and toxicity
-
-
Renal Function
-
Impaired excretion affects overall clearance
-
Prolongs half-life of xenobiotics
-
-
Enzyme Induction
-
Some drugs and chemicals increase enzyme synthesis
-
Results in faster drug metabolism and reduced effect
-
-
Enzyme Inhibition
-
Certain drugs inhibit metabolizing enzymes
-
Causes increased drug levels and toxicity
-
-
Drug Interactions
-
Concurrent drug use alters metabolism
-
Clinically important in polypharmacy
-
-
Environmental Factors
-
Smoking, alcohol, and pollutants modify enzyme activity
-
Chronic exposure enhances metabolism of some drugs
-
-
Disease Conditions
-
Endocrine disorders and infections can alter enzyme activity
-
Affect pharmacokinetics and drug response
-
Clinical Significance
-
Determines drug dosage, dosing interval, and duration of action.
-
Plays a key role in drug safety and prevention of toxicity.
-
Explains individual variation in drug response due to genetic differences.
-
Responsible for drug–drug interactions through enzyme induction or inhibition.
-
Essential for activation of prodrugs into their active forms.
-
Involved in the formation of toxic or reactive intermediates causing organ damage.
-
Important in understanding paracetamol and other drug toxicities.
-
Reduced metabolism in liver disease leads to drug accumulation.
-
Helps in managing poisoning and overdose cases.
-
Crucial in environmental and occupational toxicology.
-
Plays a role in chemical carcinogenesis due to metabolic activation of carcinogens.
-
Influences therapeutic efficacy and adverse drug reactions.
MCQs
1. Xenobiotics are best defined as
A. Endogenous metabolites
B. Nutrients required by the body
C. Foreign substances to the body
D. Hormones
Answer: C
2. The major organ involved in xenobiotic metabolism is
A. Kidney
B. Lung
C. Liver
D. Spleen
Answer: C
3. The primary purpose of xenobiotic metabolism is to
A. Increase lipid solubility
B. Increase toxicity
C. Facilitate excretion
D. Store chemicals
Answer: C
4. Most xenobiotics are initially
A. Water soluble
B. Protein bound
C. Lipid soluble
D. Ionic
Answer: C
5. Xenobiotic metabolism mainly occurs in
A. Mitochondria
B. Nucleus
C. Smooth endoplasmic reticulum
D. Lysosome
Answer: C
6. Phase I reactions are also known as
A. Conjugation reactions
B. Functionalization reactions
C. Transport reactions
D. Elimination reactions
Answer: B
7. Which of the following is NOT a Phase I reaction?
A. Oxidation
B. Reduction
C. Hydrolysis
D. Glucuronidation
Answer: D
8. The most important enzyme system involved in Phase I reactions is
A. Transferase
B. Dehydrogenase
C. Cytochrome P450
D. Isomerase
Answer: C
9. Cytochrome P450 enzymes are mainly located in
A. Cytosol
B. Mitochondria
C. Microsomes
D. Lysosomes
Answer: C
10. Phase I reactions generally
A. Always detoxify drugs
B. Always inactivate drugs
C. Introduce functional groups
D. Conjugate drugs
Answer: C
11. Phase I reactions may sometimes
A. Reduce toxicity only
B. Increase toxicity
C. Prevent excretion
D. Store drugs
Answer: B
12. Phase II reactions are also called
A. Functionalization reactions
B. Activation reactions
C. Conjugation reactions
D. Transport reactions
Answer: C
13. The main purpose of Phase II reactions is to
A. Increase lipid solubility
B. Decrease polarity
C. Increase water solubility
D. Activate xenobiotics
Answer: C
14. Which is the most common Phase II reaction?
A. Sulfation
B. Acetylation
C. Methylation
D. Glucuronidation
Answer: D
15. UDP-glucuronic acid is required for
A. Sulfation
B. Glucuronidation
C. Acetylation
D. Methylation
Answer: B
16. Glutathione conjugation is important for
A. Steroid synthesis
B. Protein synthesis
C. Detoxification of reactive intermediates
D. DNA replication
Answer: C
17. Phase II reactions usually occur in
A. Mitochondria
B. Cytosol
C. Nucleus
D. Lysosome
Answer: B
18. Phase III of xenobiotic metabolism involves
A. Oxidation
B. Reduction
C. Conjugation
D. Transport and excretion
Answer: D
19. Phase III transporters are mainly
A. Passive diffusion channels
B. ATP-dependent transporters
C. Ion channels
D. Nuclear receptors
Answer: B
20. P-glycoprotein is involved in
A. Drug activation
B. Drug conjugation
C. Drug transport and efflux
D. Drug hydrolysis
Answer: C
21. The most common route of xenobiotic excretion is
A. Feces
B. Sweat
C. Urine
D. Breath
Answer: C
22. Biliary excretion is mainly for
A. Small nonpolar molecules
B. Large polar conjugates
C. Gaseous substances
D. Water-insoluble drugs
Answer: B
23. Enterohepatic circulation results in
A. Rapid elimination
B. Drug degradation
C. Prolonged drug action
D. Reduced absorption
Answer: C
24. Volatile xenobiotics are eliminated mainly through
A. Urine
B. Bile
C. Feces
D. Lungs
Answer: D
25. Genetic polymorphism affects
A. Drug storage
B. Drug absorption
C. Drug metabolism rate
D. Drug solubility
Answer: C
26. Neonates have reduced xenobiotic metabolism due to
A. Increased enzyme activity
B. Immature enzyme systems
C. Increased renal clearance
D. Increased bile secretion
Answer: B
27. Enzyme induction leads to
A. Decreased drug metabolism
B. Increased drug toxicity
C. Faster drug metabolism
D. Drug accumulation
Answer: C
28. Enzyme inhibition causes
A. Faster drug clearance
B. Reduced drug action
C. Increased drug levels
D. Increased excretion
Answer: C
29. Liver disease affects xenobiotic metabolism by
A. Increasing enzyme activity
B. Reducing detoxification capacity
C. Enhancing excretion
D. Increasing bioavailability
Answer: B
30. Smoking influences xenobiotic metabolism by
A. Inhibiting all enzymes
B. Inducing drug-metabolizing enzymes
C. Blocking Phase II reactions
D. Reducing excretion
Answer: B
31. Paracetamol toxicity is due to formation of
A. Inactive metabolites
B. Reactive intermediates
C. Conjugated metabolites
D. Sulfated products
Answer: B
32. Xenobiotic metabolism is important in
A. Drug discovery only
B. Clinical pharmacology
C. Toxicology and therapeutics
D. All of the above
Answer: D
33. Which factor does NOT affect xenobiotic metabolism?
A. Age
B. Nutrition
C. Genetic makeup
D. Blood group
Answer: D
34. Reduced Phase II reactions are commonly seen in
A. Adults
B. Athletes
C. Neonates
D. Smokers
Answer: C
35. The ultimate goal of xenobiotic metabolism is
A. Drug storage
B. Drug activation
C. Detoxification and elimination
D. Energy production
Answer: C