Introduction
The female reproductive system comprises a group of internal and external sex organs responsible for reproduction, hormonal regulation, and secondary sexual characteristics.
Components of the Female Reproductive System
Internal Sex Organs (Located in the Pelvic Cavity)
-
A pair of ovaries
-
A pair of uterine (Fallopian) tubes
-
Uterus
-
Vagina
External Sex Organs
-
External genitalia
-
Mammary glands (female breasts)
In addition, the mammary glands, placenta, and umbilical cord are functionally associated with the female reproductive system, as their development and activity are directly related to reproductive processes.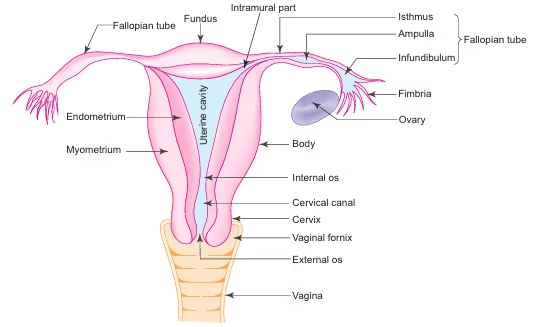
Reproductive Life Span In Females
-
The reproductive life of a female begins at puberty, usually between 13–15 years of age.
-
Puberty is characterized by structural and functional changes in the ovaries, uterus, and breasts.
-
The onset of reproductive activity is marked by the first menstrual cycle (menarche).
-
The menstrual cycle is typically 28 days in duration.
-
Reproductive life continues until menopause, which occurs between 45–55 years, when menstruation permanently ceases.
-
Thus, the fertile period of a woman spans approximately 30–40 years.
Ovarian Oocyte Reserve
-
At birth, the ovaries contain approximately 4,00,000 oocytes.
-
Most oocytes undergo degeneration (atresia) before puberty.
-
At puberty, around 40,000 oocytes remain.
-
During the entire reproductive life, only about 400 oocytes are released through ovulation.
-
The remaining oocytes degenerate at various stages.
Ovary
General Features
-
Ovaries are the female gonads.
-
Functions:
-
Production of ova
-
Secretion of female sex hormones such as oestrogen and progesterone
-
-
Shape: Almond-shaped
-
Location: Attached to the posterior layer of the broad ligament by a peritoneal fold called the mesovarium
-
Size:
-
Length: 3 cm
-
Width: 1.5 cm
-
Thickness: 1 cm
-
Structure Of Ovary
Surface Covering
-
The ovary is covered by simple cuboidal epithelium, known as germinal epithelium.
-
This epithelium is continuous with the mesothelium of the peritoneum.
-
The term germinal epithelium is a misnomer, as it does not produce germ cells (oocytes).
Tunica Albuginea
-
Beneath the germinal epithelium lies a layer of dense connective tissue called tunica albuginea.
Internal Organization
On sectioning, the ovary shows:
-
Peripheral cortex
-
Central medulla
(The boundary between cortex and medulla is indistinct.)
Medulla
-
Composed of loose fibroelastic connective tissue
-
Contains:
-
Blood vessels
-
Lymphatics
-
Nerves
-
-
Continuous with the mesovarium at the hilum
-
Contains hilus cells, similar to Leydig cells
-
These cells may act as a source of androgens in the ovary
Cortex
-
Occupies the major portion of the ovary
-
Contains:
-
Ovarian follicles at various stages of development and degeneration
-
Corpus luteum
-
Corpus albicans
-
-
Follicles are embedded in a highly cellular connective tissue stroma
-
Stromal cells are mainly large spindle-shaped fibroblasts
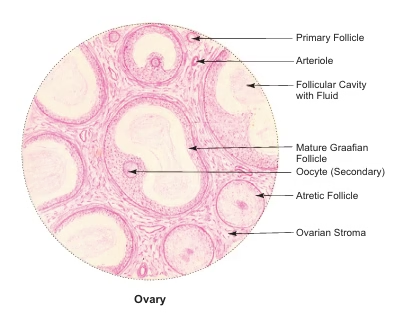
Follicular Development
-
During each menstrual cycle, a group of ovarian follicles begins to mature under the influence of follicle-stimulating hormone (FSH).
-
Usually, only one follicle reaches full maturity and ovulates.
-
The remaining follicles undergo atresia at different stages of development.
Development of Ovarian Follicle
The growth and maturation of ovarian follicles occur through a series of well-defined stages. This entire process is known as folliculogenesis.
Follicular development is broadly divided into four stages, described below.
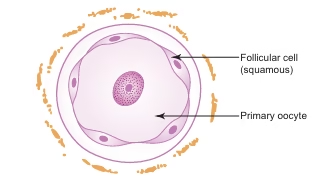
1. Primordial Follicle
-
The primordial follicle is the smallest and most primitive stage of follicular development.
-
It is located at the periphery of the ovarian cortex.
-
Each primordial follicle consists of:
-
A primary oocyte measuring approximately 20–25 μm in diameter
-
A single layer of flattened (squamous) follicular cells surrounding the oocyte
-
-
These follicles remain dormant until stimulated during the reproductive period.
-
Most primordial follicles undergo atresia, while only a few enter the growth phase.
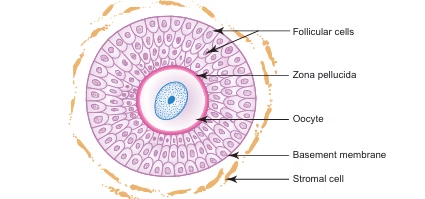
2. Primary Follicle
The primordial follicle transforms into a primary follicle under the influence of follicle-stimulating hormone (FSH). This stage is characterized by the following structural changes:
Changes In Primary Follicle
-
Increase in size of primary oocyte
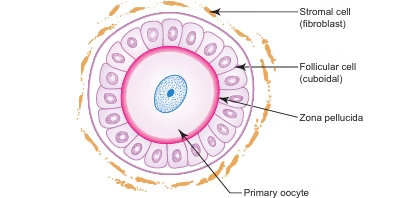
-
The primary oocyte enlarges from 20–25 μm to 50–80 μm in diameter.
-
-
Changes in follicular cells
-
Flattened squamous follicular cells become cuboidal, forming a unilaminar primary follicle.
-
These cuboidal cells further proliferate to form multiple layers, producing a multilaminar primary follicle.
-
The follicular cells are now called granulosa cells.
-
-
Basement membrane formation
-
The outermost layer of granulosa cells rests on a well-defined basement membrane.
-
This membrane separates the follicle from the ovarian stromal tissue.
-
-
Formation of zona pellucida
-
A glycoprotein layer, known as the zona pellucida, appears between the oocyte and surrounding granulosa cells.
-
It is derived from both the oocyte and follicular cells.
-
-
Formation of theca folliculi
-
The surrounding connective tissue stroma condenses around the follicle to form the theca folliculi.
-
The theca folliculi later differentiates into two distinct layers (described in later stages).
-
3. Secondary (Antral) Follicle
The primary follicle develops into a secondary (antral) follicle after undergoing the following characteristic changes:
Changes In Secondary Follicle
-
Increase in size of oocyte
-
The oocyte enlarges further and reaches its maximum size of about 125 μm in diameter.
-
-
Formation of antrum
-
Small irregular fluid-filled spaces appear between the granulosa cells.
-
These spaces gradually coalesce to form a crescent-shaped cavity called the antrum.
-
The antrum is filled with liquor folliculi.
-
-
Increase in follicular size
-
The follicle increases in diameter to about 2 mm, mainly due to:
-
Formation of the antrum
-
Accumulation of liquor folliculi
-
-
-
Differentiation of theca folliculi
-
The theca folliculi differentiates into two distinct layers:
-
Theca interna – inner, cellular, and vascular layer
-
Theca externa – outer, fibrous layer
-
-
-
Hormonal activity
-
Granulosa cells and cells of the theca interna actively secrete oestrogen, which plays a key role in follicular growth and endometrial proliferation.
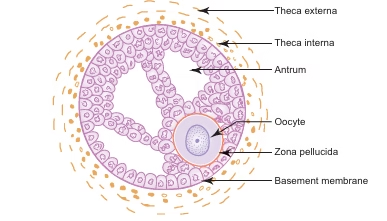
-
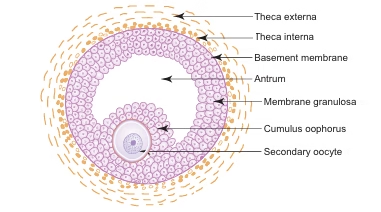
4. Mature Graafian (Tertiary) Follicle
-
With further development, the follicle enlarges due to increased accumulation of liquor folliculi in the antrum.
-
Follicular cells are divided into two groups:
-
Membrana granulosa – outer layer lining the follicular cavity
-
Cumulus oophorus – inner group of cells surrounding and attaching the ovum to one pole
-
-
The mature Graafian follicle measures 10 mm or more in diameter and bulges on the ovarian surface.
-
At this stage, the primary oocyte completes the first meiotic division to form a secondary oocyte.
-
Primary oocytes remain arrested in prophase of first meiotic division from fetal life until just before ovulation.
Ovulation
-
Occurs at mid-cycle (around day 14 of a 28-day cycle).
-
Caused by sudden increase in liquor folliculi under the influence of oestrogen.
-
Leads to rupture of the mature follicle and release of the secondary oocyte surrounded by corona radiata.
-
The ovum is released into the peritoneal cavity and is rapidly taken up by the uterine tube.
Atretic Follicle
-
Although many follicles begin to mature, only one ovulates.
-
Remaining follicles undergo atresia at various stages.
-
During atresia:
-
Granulosa cells and oocyte degenerate
-
Zona pellucida persists temporarily
-
Basement membrane thickens to form a hypertrophied glassy membrane
-
-
Ultimately, the follicle is replaced by connective tissue stroma.
Corpus Luteum
-
After ovulation, the ruptured follicle transforms into a temporary endocrine gland called corpus luteum.
-
Theca externa forms a thin capsule and blood vessels invade the structure.
-
Granulosa and theca interna cells enlarge and become lutein cells rich in lipid droplets.
-
Two types of lutein cells are present:
-
Granulosa lutein cells
-
Large, pale cells
-
Secrete progesterone
-
-
Theca lutein cells
-
Smaller, darker cells
-
Secrete oestrogen
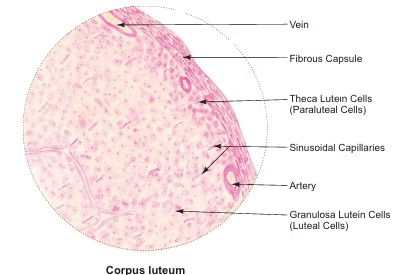
-
-
Uterine Tube
General Features
-
Uterine tubes are paired muscular tubes located in the upper free margin of the broad ligament, one on each side of the uterus.
-
Each tube measures about 10–12 cm in length.
-
Lateral end opens into the peritoneal cavity near the ovary.
-
Medial end opens into the uterine cavity.
-
Functions:
-
Nourishment of ovum/zygote
-
Transport of ovum or fertilized ovum (zygote) to the uterus
-
-
Transport of ovum occurs due to:
-
Ciliary movement of epithelial cells
-
Rhythmic contractions of the muscular wall
-
Parts of Uterine Tube
From lateral to medial, each uterine tube is divided into four parts:
-
Infundibulum
-
Funnel-shaped
-
Provided with fimbriae
-
Opens into the peritoneal cavity
-
-
Ampulla
-
Longest and widest part
-
Site of fertilization
-
-
Isthmus
-
Narrow, thick-walled segment
-
Lies just before the uterine wall
-
-
Intramural (Interstitial) Part
-
Passes through the wall of the uterus
-
Opens into the uterine cavity
-
Structure of Uterine Tube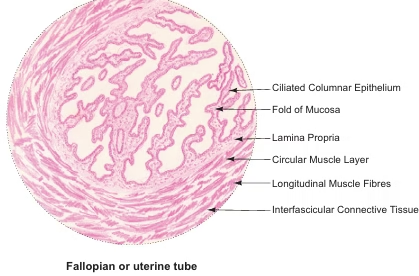
The wall of the uterine tube consists of three layers:
1. Mucosa
-
Consists of:
-
Lining epithelium
-
Thin lamina propria
-
-
Epithelium is simple ciliated columnar epithelium
-
Two types of epithelial cells:
-
Ciliated columnar cells – help in ovum transport
-
Non-ciliated peg (secretory) cells – provide nutritive secretions
-
-
Ciliated cells are shorter than peg cells, making the luminal surface uneven.
-
Proportion of cells varies with menstrual cycle:
-
More ciliated cells in proliferative phase
-
Fewer ciliated cells in secretory phase
-
-
Mucosa shows numerous branching folds, making the lumen irregular.
-
Mucosal folds are most complex in the ampulla, aiding nutrition of the fertilized ovum.
2. Muscle Layer
-
Made of smooth muscle
-
Arranged into:
-
Inner circular layer
-
Outer longitudinal layer
-
-
Responsible for peristaltic movements of the tube
3. Serosa
-
Outer covering
-
Consists of mesothelium (peritoneum of broad ligament)
-
Supported by connective tissue
Uterus
General Features
-
The uterus is a thick, pear-shaped, muscular organ located in the pelvic cavity.
-
It provides a suitable site for implantation of the blastocyst and supports the growth and development of the foetus.
-
The uterus is divided into three parts:
-
Fundus
-
Body
-
Cervix
-
-
Average dimensions:
-
Length: 7.5 cm
-
Width: 5 cm
-
Thickness: 2.5 cm
-
-
During pregnancy, the uterus undergoes marked enlargement and extends into the abdominal cavity.
Structure of Uterus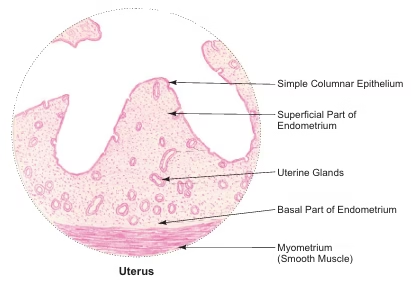
The uterine wall is composed of three layers:
1. Perimetrium
-
The outermost serous layer of the uterus.
-
Composed of:
-
Mesothelial lining (simple squamous epithelium)
-
Underlying connective tissue rich in blood vessels and elastic fibres
-
-
It is continuous with the broad ligament.
2. Myometrium
-
Forms the thick muscular middle layer, about 15 mm thick.
-
Composed of smooth muscle fibres arranged in three ill-defined layers:
-
Inner longitudinal layer
-
Middle circular layer
-
Outer longitudinal layer
-
-
The middle layer is highly vascular and contains numerous blood vessels and lymphatics.
-
Due to its vascularity, the middle layer is called the stratum vasculare.
-
During pregnancy, muscle fibres undergo:
-
Hyperplasia
-
Hypertrophy
-
3. Endometrium
-
The inner mucosal lining of the uterine cavity.
-
Consists of:
-
Lining epithelium: Simple columnar epithelium (partly ciliated)
-
Lamina propria: Highly cellular connective tissue with abundant ground substance and no collagen fibres
-
-
Contains:
-
Numerous blood vessels
-
Simple tubular uterine glands, coiled in the deeper region
-
Layers Of Endometrium
The endometrium is divided into two layers:
-
Stratum Functionalis (Superficial two-thirds)
-
Stratum Basalis (Deep one-third)
Blood Supply Of Endometrium
Two types of arteries are present:
-
Straight (Basal) arteries
-
Supply the stratum basalis
-
-
Spiral (Coiled) arteries
-
Supply the stratum functionalis
-
Highly sensitive to oestrogen and progesterone levels during the menstrual cycle
-
Cyclical Changes in Endometrium
-
The stratum functionalis undergoes cyclic structural changes under the influence of ovarian hormones.
-
These changes prepare the uterus for:
-
Implantation
-
Nourishment of embryo and foetus
-
-
If implantation does not occur:
-
The functional layer is shed during menstruation
-
The stratum basalis remains intact and regenerates a new functional layer.
-
Vagina
General Features
-
Vagina is a fibromuscular, elastic tube capable of marked distension during parturition.
-
Anterior wall measures about 7.5 cm and posterior wall about 9 cm.
-
The upper end of the vagina surrounds the cervix forming a circular recess called the fornix.
Structure of Vagina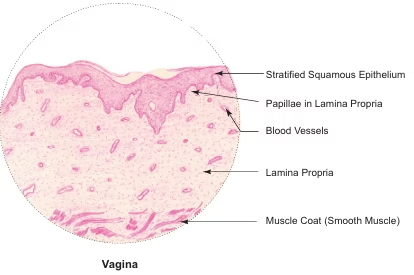
The vaginal wall consists of three layers:
1. Mucosa
-
Innermost layer with numerous transverse folds.
-
Lined by stratified squamous epithelium (150–200 μm thick), sometimes partially keratinized.
-
Epithelium accumulates glycogen under oestrogen influence.
-
Glycogen is converted into lactic acid by Döderlein’s bacillus (Lactobacillus acidophilus).
-
Acidic vaginal pH inhibits growth of pathogenic microorganisms.
-
Lamina propria:
-
Loose connective tissue
-
Rich in elastic fibres and vascular plexus
-
No glands
-
-
Vaginal lubrication occurs due to:
-
Cervical gland secretions
-
Transudate from vascular plexus
-
2. Muscle Layer
-
Composed of smooth muscle fibres
-
Arranged in:
-
Thin inner circular layer
-
Thick outer longitudinal layer
-
3. Adventitia
-
Outer connective tissue layer
-
Rich in elastic fibres
-
Contains blood vessels, lymphatics, and nerve fibres
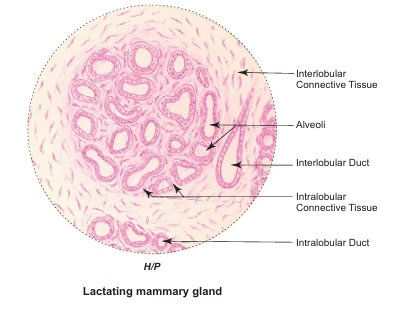
Mammary Gland
General Features
-
Mammary glands are modified apocrine sweat glands present only in mammals.
-
Function: Production of milk for nourishment of the newborn.
-
They are rudimentary in males.
-
In females, they:
-
Develop at puberty under hormonal influence
-
Reach maximum development during pregnancy and lactation
-
Undergo involution and atrophy after menopause
-
Gross Structure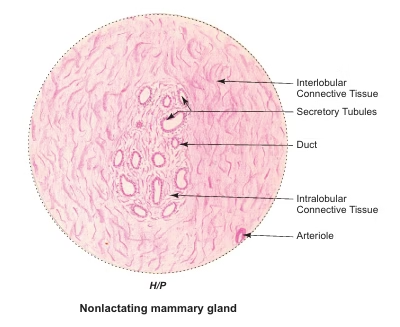
-
Each mammary gland consists of 15–20 independent lobes.
-
Lobes are separated by interlobular septa made of dense connective and adipose tissue.
-
Each lobe is a compound tubuloalveolar gland.
-
The duct of each lobe, called the lactiferous duct, opens on the nipple.
-
Thus, 15–20 lactiferous ducts open separately on the nipple.
-
Each duct shows a dilatation beneath the areola called the lactiferous sinus.
Areola And Nipple
-
Areola:
-
Dark pigmented skin surrounding the nipple
-
Pigmentation increases during pregnancy
-
Contains circular smooth muscle fibres
-
Presence of large sebaceous glands forming tubercles of Montgomery
-
-
Nipple:
-
Contains longitudinally arranged smooth muscle fibres
-
Muscle contraction causes erection of the nipple
-
Microscopic Organization
-
Within each lobe:
-
Lactiferous ducts divide into terminal ducts
-
Terminal ducts lead to lobules
-
-
Each lobule consists of numerous alveoli
-
Alveoli are embedded in loose intralobular connective tissue
-
Intralobular connective tissue contains:
-
Lymphocytes
-
Plasma cells
-
-
Plasma cells secrete IgA, which is released into colostrum near the end of pregnancy
-
IgA provides passive immunity to the newborn
-
Lobules are separated by moderately dense interlobular connective tissue septa.
Placenta
General Features
-
Placenta is a specialised extra-embryonic tissue that brings foetal blood vessels into close relation with maternal blood for nutrition, respiration, excretion, and metabolism during intrauterine life.
-
At term, it is discoidal, weighs about 500 g, measures 15–20 cm in diameter and 3 cm in thickness.
-
It is derived from:
-
Foetal part: Chorion
-
Maternal part: Decidua basalis
-
-
Foetal surface: Smooth and shiny, covered by amnion
-
Maternal surface: Rough, covered by decidua basalis, divided into 15–20 cotyledons by incomplete septa
Structure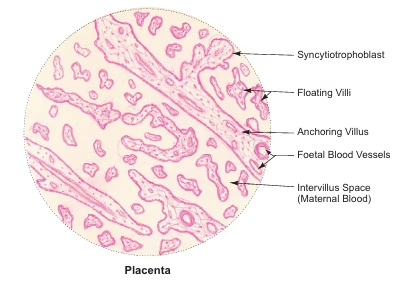
-
Placenta consists of numerous chorionic villi separated by intervillous space containing maternal blood from spiral arteries.
-
Exchange of gases and metabolites occurs between maternal blood and foetal capillaries across the placental barrier.
-
Each villus has:
-
A central connective tissue core with foetal blood vessels
-
Cytotrophoblast (present in early pregnancy, disappears later)
-
Syncytiotrophoblast, which secretes progesterone, oestrogen, hCG, and other placental hormones.
-
Umbilical Cord
General Features
-
Umbilical cord connects the foetus to the placenta.
-
It measures about 50 cm in length and 1–2 cm in width.
-
It is derived from the connecting stalk of the embryo.
Structure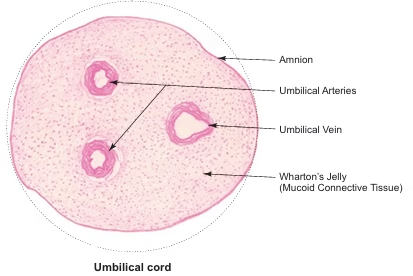
A cross-section at term shows:
-
One umbilical vein – thin wall, wide lumen; carries oxygenated blood from placenta to foetus
-
Two umbilical arteries – thick wall, narrow lumen; carry deoxygenated blood from foetus to placenta
-
Wharton’s jelly – gelatinous mucoid connective tissue supporting the vessels
-
Covering of amnion – simple cuboidal epithelium.
MCQs
-
The female reproductive system is primarily responsible for:
A. Digestion
B. Respiration
C. Reproduction and hormonal regulation
D. Excretion
Ans: C -
Which of the following is an internal sex organ?
A. Mammary gland
B. Labia majora
C. Ovary
D. Mons pubis
Ans: C -
All are internal sex organs EXCEPT:
A. Ovary
B. Uterus
C. Vagina
D. Mammary gland
Ans: D -
Mammary glands are functionally associated with:
A. Digestive system
B. Female reproductive system
C. Urinary system
D. Endocrine system only
Ans: B -
The reproductive life of a female begins at:
A. Birth
B. Puberty
C. Menopause
D. Childhood
Ans: B -
Puberty usually occurs between:
A. 8–10 years
B. 10–12 years
C. 13–15 years
D. 16–18 years
Ans: C -
First menstrual cycle is called:
A. Menopause
B. Ovulation
C. Menarche
D. Fertilization
Ans: C -
Average duration of menstrual cycle is:
A. 21 days
B. 24 days
C. 28 days
D. 35 days
Ans: C -
Menopause usually occurs between:
A. 35–40 years
B. 40–45 years
C. 45–55 years
D. 55–65 years
Ans: C -
Fertile period of a woman is approximately:
A. 10–15 years
B. 20–25 years
C. 30–40 years
D. 45–50 years
Ans: C
Ovarian Oocyte Reserve
-
Number of oocytes at birth is approximately:
A. 40,000
B. 1 lakh
C. 4 lakh
D. 4 million
Ans: C -
Number of oocytes remaining at puberty is about:
A. 4,000
B. 40,000
C. 4 lakh
D. 400
Ans: B -
Number of oocytes ovulated during entire reproductive life:
A. 40
B. 100
C. 400
D. 4000
Ans: C -
Degeneration of ovarian follicles is called:
A. Ovulation
B. Atresia
C. Fertilization
D. Implantation
Ans: B
Ovary
-
Ovaries are the female:
A. Ducts
B. Accessory glands
C. Gonads
D. External organs
Ans: C -
Main hormone secreted by ovary:
A. Testosterone
B. Progesterone
C. Estrogen
D. Both B and C
Ans: D -
Shape of ovary is:
A. Round
B. Pear-shaped
C. Almond-shaped
D. Oval
Ans: C -
Ovary is attached to broad ligament by:
A. Mesosalpinx
B. Mesometrium
C. Mesovarium
D. Ligamentum teres
Ans: C -
Germinal epithelium of ovary is:
A. Stratified squamous
B. Simple cuboidal
C. Simple columnar
D. Transitional
Ans: B -
Germinal epithelium is a misnomer because it:
A. Produces hormones
B. Produces ova
C. Does not produce germ cells
D. Is ciliated
Ans: C -
Tunica albuginea is made of:
A. Loose connective tissue
B. Dense connective tissue
C. Muscle tissue
D. Epithelium
Ans: B -
Medulla of ovary contains all EXCEPT:
A. Blood vessels
B. Lymphatics
C. Nerves
D. Ovarian follicles
Ans: D -
Hilus cells resemble:
A. Sertoli cells
B. Leydig cells
C. Granulosa cells
D. Theca cells
Ans: B -
Ovarian follicles are located in:
A. Medulla
B. Cortex
C. Hilum
D. Mesovarium
Ans: B
Follicular Development
-
Folliculogenesis refers to:
A. Ovulation
B. Fertilization
C. Development of ovarian follicles
D. Implantation
Ans: C -
Primordial follicles are located in:
A. Medulla
B. Hilum
C. Periphery of cortex
D. Mesovarium
Ans: C -
Primordial follicle contains:
A. Secondary oocyte
B. Primary oocyte
C. Ovum
D. Zygote
Ans: B -
Follicular cells of primordial follicle are:
A. Cuboidal
B. Columnar
C. Squamous
D. Stratified
Ans: C -
Zona pellucida appears first in:
A. Primordial follicle
B. Primary follicle
C. Secondary follicle
D. Graafian follicle
Ans: B -
Antrum is filled with:
A. Blood
B. Mucus
C. Liquor folliculi
D. Lymph
Ans: C -
Site of estrogen secretion in follicle:
A. Zona pellucida
B. Theca externa
C. Granulosa and theca interna
D. Medulla
Ans: C -
Mature Graafian follicle size is about:
A. 2 mm
B. 5 mm
C. 10 mm or more
D. 20 mm
Ans: C -
Ovulation occurs around:
A. Day 7
B. Day 10
C. Day 14
D. Day 21
Ans: C -
Ovum released during ovulation is:
A. Primary oocyte
B. Secondary oocyte
C. Ovogonium
D. Zygote
Ans: B
Corpus Luteum
-
Corpus luteum is formed from:
A. Atretic follicle
B. Ruptured follicle
C. Primordial follicle
D. Secondary follicle
Ans: B -
Granulosa lutein cells secrete:
A. Estrogen
B. Progesterone
C. FSH
D. LH
Ans: B -
Theca lutein cells secrete:
A. Progesterone
B. Estrogen
C. Prolactin
D. Oxytocin
Ans: B
Uterine Tube
-
Site of fertilization is:
A. Infundibulum
B. Ampulla
C. Isthmus
D. Intramural part
Ans: B -
Epithelium of uterine tube is:
A. Stratified squamous
B. Simple cuboidal
C. Simple ciliated columnar
D. Transitional
Ans: C -
Non-ciliated cells of uterine tube are called:
A. Goblet cells
B. Peg cells
C. Basal cells
D. Clara cells
Ans: B
Uterus
-
Highly vascular layer of myometrium is called:
A. Stratum basale
B. Stratum functionalis
C. Stratum vasculare
D. Perimetrium
Ans: C -
Endometrium is lined by:
A. Stratified squamous epithelium
B. Simple cuboidal epithelium
C. Simple columnar epithelium
D. Transitional epithelium
Ans: C -
Spiral arteries supply:
A. Myometrium
B. Stratum basalis
C. Stratum functionalis
D. Cervix
Ans: C
Vagina, Placenta & Umbilical Cord
-
Vaginal epithelium is:
A. Simple columnar
B. Stratified squamous
C. Transitional
D. Cuboidal
Ans: B -
Acidic pH of vagina is due to:
A. Estrogen
B. Progesterone
C. Lactic acid
D. Mucus
Ans: C -
Placenta is derived from:
A. Foetal tissue only
B. Maternal tissue only
C. Both foetal and maternal tissues
D. Endometrium only
Ans: C -
Functional unit of placenta is:
A. Cotyledon
B. Villus
C. Lobule
D. Alveolus
Ans: B -
Hormone secreted by syncytiotrophoblast:
A. FSH
B. LH
C. hCG
D. Prolactin
Ans: C -
Number of umbilical arteries present is:
A. One
B. Two
C. Three
D. Four
Ans: B -
Wharton’s jelly is a type of:
A. Fibrous tissue
B. Adipose tissue
C. Gelatinous connective tissue
D. Cartilage
Ans: C