
Introduction
- Ancylostoma is a genus of parasitic hookworms that infect the human intestine, primarily causing hookworm disease.
- The infection is commonly caused by Ancylostoma duodenale and Ancylostoma braziliense, responsible for human hookworm infections.
- Ancylostoma species are soil-transmitted helminths, and they primarily infect humans through skin penetration or ingesting contaminated food or water.
- These parasites significantly impact public health, especially in regions with poor sanitation and hygiene practices.
Geographical Distribution
Ancylostoma species are found worldwide, particularly in regions with tropical and subtropical climates. The geographical distribution of hookworm infections is most common in:
-
- Sub-Saharan Africa
- Southeast Asia
- South and Central America
- India
- Middle East
- Southern United States
Ancylostoma duodenale has a wide distribution, while Ancylostoma braziliense is found in South America, Southeast Asia, and parts of Africa. The prevalence of infection is especially high in areas with poor sanitation, inadequate hygiene, and lack of access to clean water. The transmission rate is also higher in communities with high rates of barefoot walking and in rural areas where individuals have direct contact with contaminated soil.
Habitat
The adult Ancylostoma worms reside in the small intestine of humans, particularly in the duodenum and jejunum. The larvae hatch in the soil, and their journey to the host involves migrating through the skin and into the bloodstream, ultimately reaching the lungs, where they ascend to the throat and are swallowed to mature in the intestine.
-
- Adults: In the human host, adult hookworms are embedded in the intestinal lining. They attach to the intestinal walls using specialized mouthparts, which allow them to feed on blood.
- Larvae: The larvae live in the soil or may infect the host through skin contact or ingestion. The larvae can survive for weeks to months in the soil, awaiting contact with a suitable host.
Morphology
- Adult Hookworms:
- Size: Adult female Ancylostoma worms are larger than the males. Females measure around 10-13 mm long, and males are approximately 8-10 mm.
- Shape: The body is cylindrical and tapered, with a curved, hook-like shape at the anterior end, hence the name “hookworm.”
- Mouthparts: The mouth is equipped with cutting plates or teeth, which help the hookworms anchor to the intestinal wall and feed on blood.
- Color: The body of the adult is typically white or cream-colored.
- Larvae:
- The larvae are small, transparent, and non-segmented. They can migrate through the skin or lungs to reach the intestines.
- Filariform larvae are the infective form, capable of penetrating the skin, while the rhabditiform larvae are the first-stage larvae excreted in feces.
Life Cycle
The life cycle of Ancylostoma involves several stages: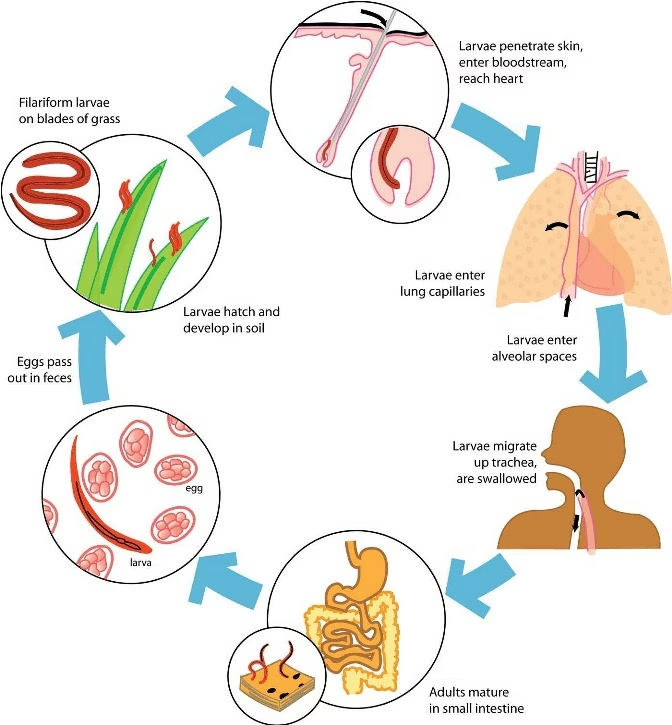
-
- Eggs in the Environment: Adult female worms lay eggs in the human intestine, passed in the stool. These eggs are oval, thin-walled, and contain an embryonated zygote.
- Larvae Development: In the soil, the eggs hatch into rhabditiform larvae, further developing into filariform larvae. The filariform larvae are in the infective stage.
- Infection via Skin Penetration: The filariform larvae can penetrate the skin, typically through bare feet or contact with contaminated soil. Once the larvae penetrate the skin, they enter the bloodstream and migrate to the lungs.
- Migration to the Lungs and Throat: The larvae travel through the bloodstream to the lungs, ascending through the pulmonary vessels to the bronchi and trachea. The larvae then migrate up the throat to be swallowed.
- Maturation in the Small Intestine: After being swallowed, the larvae reach the small intestine, where they mature into adult worms. They attach to the intestinal wall and begin feeding on blood, causing damage to the mucosal lining.
- Egg Laying: The adult female hookworms lay eggs in the small intestine, and the cycle continues with the eggs being passed in the feces.
The life cycle of Ancylostoma is approximately 4-8 weeks, from the time of infection to egg production.
Mode of Transmission
Ancylostoma is transmitted via the fecal-oral route or by skin penetration:
-
- Skin Penetration: The most common transmission route is contact with infected soil, where the filariform larvae penetrate the skin, often through bare feet. The larvae then migrate through the body, eventually reaching the small intestine.
- Ingestion of Contaminated Food or Water: In some cases, Ancylostoma larvae may be ingested if the soil or water is contaminated, though this is less common.
- Auto-Infection: In rare cases, larvae can cause auto-infection if they hatch inside the intestines and re-enter the body through the intestinal walls.
Incubation Time
The incubation period for Ancylostoma infection varies depending on the route of infection:
-
- After skin penetration, the larvae may take approximately 1-2 weeks to reach the lungs and ascend the respiratory tract to the intestines. From there, they mature into adult worms and begin laying eggs.
- Once the larvae mature in the intestines, they start producing eggs within 4-6 weeks post-infection.
Pathogenesis
The pathogenesis of Ancylostoma infection primarily involves the damage caused by hookworms as they feed on blood and penetrate tissues. The main pathogenic effects include:
-
- Intestinal Damage: The adult worms attach to the intestinal mucosa using their mouthparts, leading to blood loss. This can result in iron deficiency anemia, especially in heavy infections.
- Inflammation and Ulceration: The worms’ feeding activities can lead to local inflammation and ulceration in the intestines, causing discomfort, pain, and bleeding.
- Pulmonary Symptoms: As the larvae migrate through the lungs, they can cause a condition known as Löffler’s syndrome, which includes cough, fever, and eosinophilia (an increase in eosinophils in the blood).
- Chronic Anemia: Due to continuous blood loss, heavy hookworm infections can lead to chronic anemia, particularly in children and individuals with poor nutritional status.
- Growth Impairment: In children, chronic infections can result in growth retardation and cognitive impairment due to nutritional deficiencies (particularly iron and protein).
Laboratory Diagnosis
Diagnosis of Ancylostoma infection is primarily made by detecting hookworm eggs or larvae in stool samples:
-
- Microscopic Examination of Stool: The most common diagnostic method is the microscopic examination of stool samples to detect hookworm eggs. The eggs are oval and thin-walled, with the developing larvae visible under a microscope.
- Stool Culture for Larvae: In some cases, stool cultures can be used to hatch larvae from eggs, which can then be identified as either Ancylostoma duodenale or Ancylostoma braziliense.
- Peripheral Blood Smear: A blood test may show eosinophilia, an increased number of eosinophils, often seen in parasitic infections like hookworm disease.
- Fecal Examination for Hookworm Larvae: If the larvae are present in the stool (less common), they can be identified under a microscope.
Treatment
Treatment for Ancylostoma infections involves antihelminthic medications:
-
- Mebendazole: A common and effective treatment for hookworm infections, mebendazole inhibits the worms’ ability to absorb glucose, effectively killing them. A single dose is usually sufficient, though a second dose may be given after 2 weeks.
- Albendazole: Similar to mebendazole, albendazole is another effective drug for treating hookworm infections. It also works by disrupting the worms’ metabolic processes.
- Pyrantel Pamoate: This medication is another option for treating hookworm infections. It works by paralyzing the worms, allowing the body to expel them.
- Iron Supplementation: Iron supplements are often given to help treat iron-deficiency anemia due to the blood loss associated with hookworm infections.
- Blood Transfusion: In severe cases of anemia, blood transfusions may be necessary to restore blood volume and improve oxygen delivery.
Prevention
Preventing Ancylostoma infections involves improving hygiene and sanitation practices:
-
- Improved Sanitation: Ensuring access to clean, safe water and proper sanitation facilities helps reduce soil and water contamination with hookworm larvae.
- Use of Footwear: Wearing shoes, particularly in areas with poor sanitation, can prevent larvae from penetrating the skin.
- Health Education: Educating individuals, particularly in rural areas, about hookworm transmission and the importance of handwashing, clean water, and wearing shoes is crucial for prevention.
- Mass Deworming Programs: In endemic areas, mass deworming programs using antihelminthic medications can help control the spread of hookworm infections.