Introduction
- Balantidium coli is a ciliate protozoan that primarily inhabits the large intestine of humans and other mammals.

- Although it can infect many animals, humans are typically infected by ingesting cysts through contaminated water, food, or hands.
- Balantidiasis (the disease caused by B. coli) is most common in tropical or subtropical regions, particularly where sanitation practices are poor.
- The infection is typically transmitted via the fecal-oral route, often through contaminated drinking water or food.
Morphology
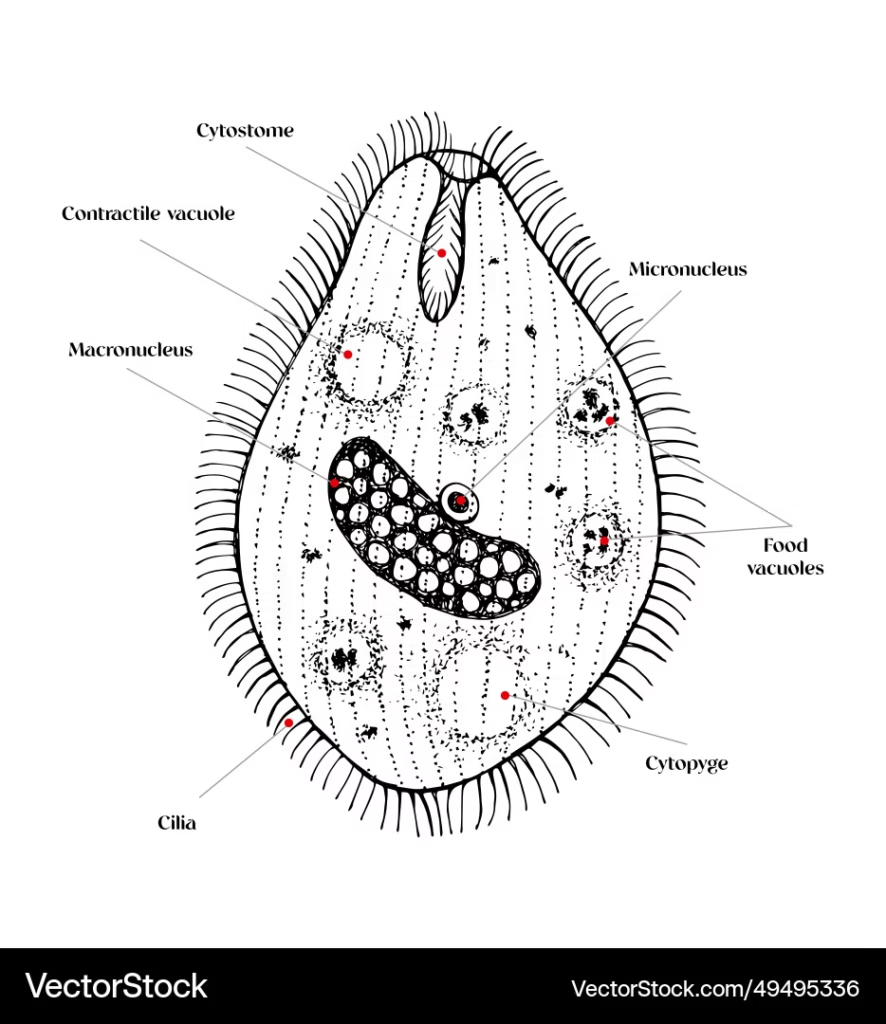
Trophozoite (Active Form)
- The trophozoite is the parasite’s motile, feeding, and dividing stage. It is typically found in the intestinal lumen and can cause infection in the host.
- Shape: Oval or pear-shaped, with a flattened ventral surface and a convex dorsal surface.
- Size: 30-200 micrometers in length and 20-150 micrometers in width (the largest protozoan parasite).
- Cilia: The cilia cover the trophozoite’s surface, enabling its movement and feeding (by pushing particles into the oral groove).
- Nucleus: The trophozoite has two nuclei:
- Macronucleus: Large, kidney-shaped, located centrally or slightly to the rear.
- Micronucleus: Smaller, round, and responsible for reproduction.
- Oral Groove and Cytostome: The oral groove is a depression that leads to the cytostome (mouth), where ingestion of food particles (usually bacteria or dead tissue) occurs.
- Cytoplasm: Granular with small vacuoles, which can contain ingested food particles. The parasite also has contractile vacuoles to expel excess water.
Cyst (Infective Form)
- The cyst is the infective form that allows the parasite to survive outside the host in harsh environments, facilitating transmission to new hosts.
- Shape: Oval or spherical.
- Size: 40-60 micrometers in length and 30-50 micrometers in width.
- Wall: The cyst has a thick, resistant wall that provides protection against environmental factors like dehydration and acidic pH.
- Contents: The cyst contains the macronucleus and micronucleus. It is highly resistant to external conditions and can survive in the environment for several months.
- Cysts are excreted in the stool of infected individuals and can contaminate food and water supplies, perpetuating the transmission cycle.
Life Cycle 
The life cycle of Balantidium coli involves both a trophozoite (active) and a cyst (infective) stage:
-
Ingestion of Cysts: Humans or other hosts ingest cysts from contaminated food, water, or hands. The cysts are typically found in fecally contaminated sources.
-
Excystation: After reaching the small intestine, the cyst undergoes excystation, where the thick cyst wall breaks down, releasing the trophozoites.
-
Colonization: The trophozoites move into the large intestine (where they preferentially colonize the cecum and colon).
- Trophozoites are active and feed on bacteria, cellular debris, and, occasionally, host tissues. They can also divide asexually via binary fission.
- In the intestines, trophozoites attach to the epithelial cells, leading to possible ulceration and inflammation of the gut lining.
-
Encystation: As trophozoites travel through the intestines, some undergo encystation (transformation into cysts) in the distal colon and rectum.
- These cysts are excreted in the stool, ready to be ingested by a new host, completing the cycle.
Clinical Features
Many infections with Balantidium coli are asymptomatic, but when symptoms do occur, they can range from mild to severe, including:
Asymptomatic Infections:
- In many cases, individuals may be infected but show no symptoms. The immune system may control the parasite, preventing any noticeable signs of disease.
Symptomatic Infections:
- Acute Balantidiasis: This occurs when trophozoites invade and cause inflammation in the colon.
- Symptoms:
- Diarrhea (which may be bloody in severe cases)
- Abdominal cramps
- Nausea and vomiting
- Fever
- Weight loss
- Rectal tenesmus (a feeling of needing to pass stool even when the rectum is empty)
- Symptoms:
- Severe Infection:
- In severe cases, trophozoites can invade the intestinal mucosa, leading to ulcers, perforation, peritonitis, and possibly sepsis.
- Extra-intestinal manifestations are rare, including liver abscesses, pneumonia, or peritonitis.
Lab Diagnosis
Diagnosing Balantidium coli infection involves detecting the parasite’s cysts or trophozoites in clinical samples (usually stool samples). Here are common diagnostic methods:
Microscopic Examination of Stool Samples:
- Direct Microscopy: Fresh stool samples can be examined for the characteristic trophozoites or cysts.
- A wet mount is often prepared, and the sample can be examined under a light microscope. The cilia of trophozoites allow them to be easily recognized.
- Iodine staining can help visualize the cysts, as iodine stains them, making them more visible.
Fecal Smear:
- A fecal smear can be made by spreading a small portion of stool on a glass slide and examining it under the microscope.
- Cysts will appear as spherical or oval structures with a thick wall.
- Trophozoites may be seen moving and exhibiting their cilia under high magnification.
Stool Culture:
- Stool cultures can grow trophozoites in a special medium, which is not typically done in routine clinical settings.
Molecular Diagnostic Methods:
- PCR (Polymerase Chain Reaction) can detect DNA from the parasite, providing a more sensitive and specific test than microscopy.
Serology:
- While serological tests are not routinely used for Balantidium coli infections, ELISA (Enzyme-Linked Immunosorbent Assay) or indirect hemagglutination tests could be used to detect specific antibodies or antigens related to B. coli.
Treatment
- Metronidazole is the most commonly used drug for treating Balantidium coli infections. It targets the anaerobic nature of the parasite and kills both the trophozoite and cyst forms.
- Tetracycline is also effective, though not as commonly used as metronidazole.
- Supportive care: For severe cases, fluid and electrolyte replacement may be required to manage dehydration and other complications.