Introduction
-
Bone is a specialized connective tissue that provides mechanical support, protection, mineral storage, and metabolic regulation.
-
Bone is a dynamic connective tissue, not a static structure; it continuously undergoes resorption and formation throughout life.
-
Chemically, bone is composed of organic matrix, inorganic mineral salts, and water, which together provide strength, rigidity, and flexibility.
-
The organic component mainly consists of collagen type I and ground substance, giving bone its tensile strength.
-
The inorganic component is primarily calcium and phosphate in the form of hydroxyapatite crystals, responsible for hardness and compressive strength.
-
Bone serves as a reservoir of minerals, especially calcium and phosphate, playing a key role in mineral homeostasis.
-
Bone metabolism is tightly regulated by hormones, vitamin D, and local biochemical factors, ensuring normal growth and maintenance.
Functions of Bone
-
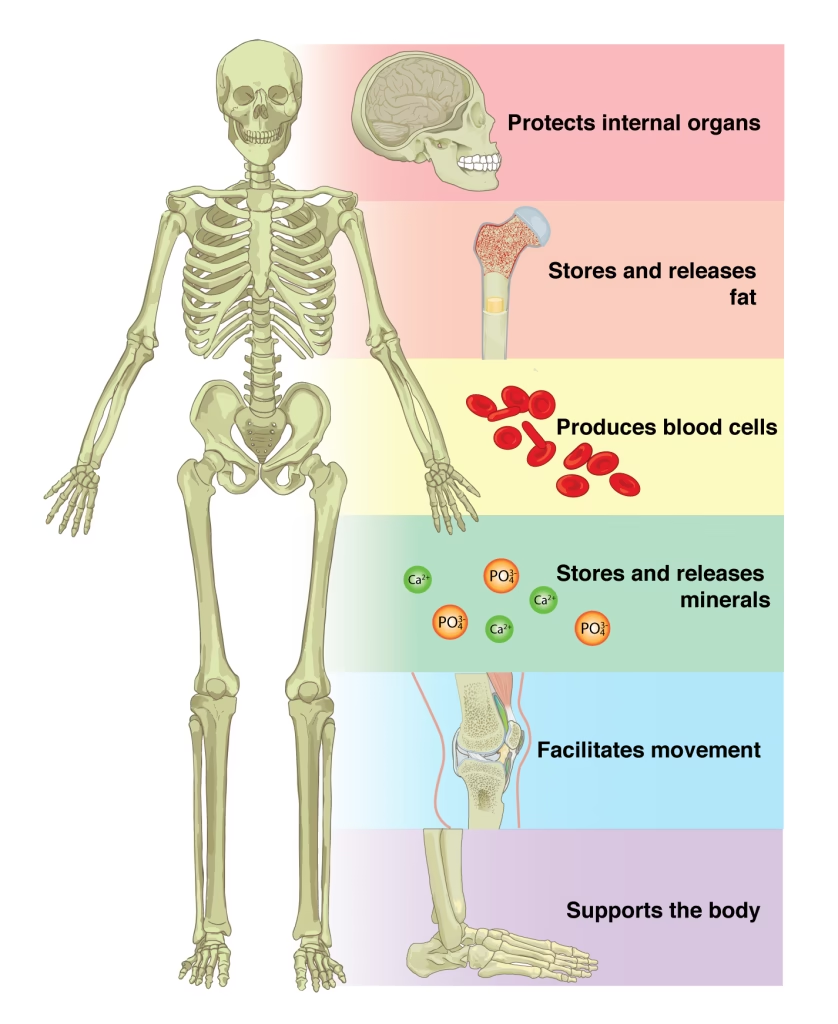
Structural support: Forms the rigid framework of the body and provides attachment for muscles and teeth, especially alveolar bone in dentistry.
-
Protection of vital organs: Protects brain, spinal cord, heart, and lungs through skull, vertebrae, and rib cage.
-
Mineral reservoir: It serves as the primary storage site for calcium and phosphate, thereby helping to maintain serum calcium homeostasis.
-
Mechanical function: Provides strength and rigidity to withstand compression and stress during mastication and locomotion.
-
Hematopoiesis: Bone marrow is the site of formation of red blood cells, white blood cells, and platelets.
-
Acid–base balance: Bone salts buffer excess acids and help maintain systemic pH balance.
-
Metabolic activity: Bone is continuously remodeled through osteoblast and osteoclast activity, making it a metabolically active tissue.
-
Dental relevance: Essential for tooth anchorage, orthodontic tooth movement, implant osseointegration, and post-extraction healing.
Chemical Composition of Bone
Bone is a composite tissue composed of organic and inorganic components, arranged in a highly organized manner to provide strength, rigidity, and metabolic activity.
Composition
-
Organic matrix: ~30–35%
-
Inorganic mineral phase: ~65–70%
-
Water: Present in small amount, bound to matrix
1. Organic Matrix of Bone (Osteoid)
The organic matrix is responsible for flexibility and tensile strength.
Major Components
a) Collagen (≈ 90% of organic matrix)
-
Mainly Type I collagen
-
Synthesized by osteoblasts
-
Provides tensile strength and toughness
-
Acts as a scaffold for mineral deposition
b) Non-Collagenous Proteins
-
Osteocalcin – binds calcium, regulates mineralization
-
Osteonectin – links collagen with mineral
-
Bone sialoprotein – involved in crystal nucleation
-
Proteoglycans – regulate hydration and diffusion
Biochemical importance: Organic matrix controls rate and pattern of mineralization.
2. Inorganic Mineral Phase of Bone
The inorganic component provides hardness and rigidity.
Major Mineral
-
Hydroxyapatite crystals
Ca₁₀(PO₄)₆(OH)₂
Mineral Constituents
-
Calcium
-
Phosphate
-
Carbonate
-
Magnesium
-
Sodium
-
Fluoride (strengthens bone and teeth)
Functions of Inorganic Phase
-
Provides resistance to compression
-
Gives bone its rigid structure
-
Acts as a reservoir of calcium and phosphate
-
Maintains serum mineral homeostasis
3. Water in Bone
-
Present in hydration shells of collagen and crystals
-
Facilitates diffusion of ions and metabolites
-
Contributes to bone resilience
Composition Summary
| Component | Percentage | Function |
|---|---|---|
| Organic matrix | 30–35% | Flexibility, tensile strength |
| Inorganic minerals | 65–70% | Hardness, rigidity |
| Water | Minor | Metabolic exchange |
Bone Cells and Their Biochemical Role
Bone is a metabolically active tissue in which specialized cells continuously regulate bone formation, maintenance, and resorption through tightly controlled biochemical processes.
1. Osteoblasts – Bone-Forming Cells
Origin
-
Derived from mesenchymal stem cells
Biochemical Functions
-
Synthesize organic bone matrix (osteoid):
-
Type I collagen
-
Osteocalcin
-
Osteonectin
-
Bone sialoprotein
-
-
Secrete alkaline phosphatase, which:
-
Increases local phosphate concentration
-
Promotes mineralization
-
-
Initiate deposition of hydroxyapatite crystals
Fate of Osteoblasts
-
Become osteocytes
-
Remain as bone lining cells
-
Undergo apoptosis
Biochemical marker of osteoblast activity:
Serum alkaline phosphatase
2. Osteocytes – Bone-Maintaining Cells
Origin
-
Mature osteoblasts entrapped in bone matrix
Location
-
Reside in lacunae
-
Connected by canaliculi
Biochemical Functions
-
Maintain bone matrix integrity
-
Act as mechanosensors, responding to mechanical stress
-
Regulate mineral exchange between bone and blood
-
Secrete signaling molecules that influence:
-
Osteoblast activity
-
Osteoclast activation
-
Key role: Long-term maintenance of bone metabolism
3. Osteoclasts – Bone-Resorbing Cells
Origin
-
Derived from monocyte–macrophage lineage
Structure
-
Large, multinucleated cells
-
Possess ruffled border and sealing zone
Biochemical Functions
-
Resorb bone by:
-
Secretion of hydrochloric acid → dissolves hydroxyapatite
-
Release of lysosomal enzymes (e.g., cathepsin K) → degrade collagen
-
-
Create resorption lacunae (Howship’s lacunae)
Biochemical marker of osteoclast activity:
Increased urinary hydroxyproline
4. Bone Lining Cells
-
Flattened, inactive osteoblasts
-
Cover bone surface
-
Regulate mineral exchange
-
Important in initiating remodeling cycles
Summary
| Cell | Origin | Main Biochemical Role |
|---|---|---|
| Osteoblast | Mesenchymal | Bone formation, collagen synthesis |
| Osteocyte | Osteoblast | Bone maintenance, mechanosensing |
| Osteoclast | Monocyte lineage | Bone resorption |
| Lining cells | Osteoblast | Mineral regulation |
Bone Mineralization
-
Bone mineralization is the biochemical process by which calcium and phosphate salts are deposited on the organic bone matrix (osteoid) to form hard, mineralized bone.
-
It converts soft osteoid into rigid bone through controlled hydroxyapatite crystal formation.
Phases of Bone Mineralization
Bone mineralization occurs in two main phases:
1. Primary Mineralization
-
Occurs rapidly after osteoid formation
-
Takes place within matrix vesicles released from osteoblasts
-
Characterized by initial deposition of calcium phosphate crystals
Role of Matrix Vesicles
-
Rich in:
-
Alkaline phosphatase
-
Calcium-binding proteins
-
Phospholipids
-
-
Function:
-
Increase local concentration of Ca²⁺ and PO₄³⁻
-
Provide a protected site for crystal nucleation
-
2. Secondary Mineralization
-
Slow and progressive process
-
Continues over weeks to months
-
Increases:
-
Bone density
-
Mechanical strength
-
-
Involves growth and maturation of hydroxyapatite crystals along collagen fibers
Biochemical Mechanism of Mineralization
-
Osteoblasts secrete osteoid (Type I collagen + non-collagenous proteins)
-
Alkaline phosphatase:
-
Hydrolyzes phosphate esters
-
Raises local phosphate concentration
-
-
Calcium and phosphate combine to form:
-
Hydroxyapatite crystals
-
Ca₁₀(PO₄)₆(OH)₂
-
-
Crystals align along collagen fibrils → rigid bone matrix
Factors Required for Normal Bone Mineralization
Minerals
-
Calcium
-
Phosphate
-
Magnesium (minor role)
Vitamins
-
Vitamin D – increases intestinal absorption of calcium and phosphate
-
Vitamin C – required for collagen synthesis
-
Vitamin K – activates osteocalcin for calcium binding
Enzymes
-
Alkaline phosphatase (key enzyme)
Hormones
-
Parathyroid hormone (PTH)
-
Calcitonin
-
Vitamin D (Calcitriol)
Inhibitors of Mineralization
-
Pyrophosphate
-
Low alkaline phosphatase activity
-
Deficiency of vitamin D or calcium
Clinical Correlation
| Disorder | Biochemical Defect |
|---|---|
| Rickets (children) | Defective mineralization due to vitamin D deficiency |
| Osteomalacia (adults) | Inadequate mineral deposition |
| Hypophosphatasia | Low alkaline phosphatase activity |
Hormonal Regulation of Bone Metabolism
Bone metabolism is a dynamic, hormonally regulated process that maintains bone strength and serum calcium–phosphate homeostasis through balanced bone formation and resorption.
1. Parathyroid Hormone (PTH)
Source
- Parathyroid glands
Biochemical Actions
- Increases serum calcium levels
- Stimulates osteoclast-mediated bone resorption (indirectly via osteoblasts)
- Increases renal calcium reabsorption
- Increases phosphate excretion
Mechanism
- PTH binds to osteoblast receptors
- Osteoblasts release RANKL
- RANKL activates osteoclasts → bone resorption
Clinical Correlation
- Excess PTH → bone demineralization
- Important cause of alveolar bone loss
2. Vitamin D (Calcitriol – 1,25-dihydroxyvitamin D₃)
Source
- Formed in skin → liver → kidney (active form)
Biochemical Actions
- Increases intestinal absorption of calcium and phosphate
- Promotes bone mineralization
- Enhances osteoblast function
- At high levels, may increase bone resorption
Clinical Correlation
- Deficiency → rickets (children), osteomalacia (adults)
- Affects alveolar bone density
3. Calcitonin
Source
- Parafollicular (C) cells of thyroid gland
Biochemical Actions
- Decreases serum calcium
- Directly inhibits osteoclast activity
- Reduces bone resorption
Clinical Importance
- Minor role in adults
- Protective during periods of high calcium load
- Therapeutic use in osteoporosis (limited)
4. Growth Hormone (GH)
Source
- Anterior pituitary
Biochemical Actions
- Stimulates bone growth via IGF-1
- Increases osteoblast activity
- Promotes protein synthesis in bone matrix
Clinical Correlation
- Excess → acromegaly
- Deficiency → reduced bone growth
5. Thyroid Hormones (T₃ and T₄)
Biochemical Actions
- Increase bone turnover
- Excess thyroid hormone:
- Increases bone resorption
- Leads to bone loss
Clinical Correlation
- Hyperthyroidism → osteoporosis risk
6. Sex Hormones (Estrogen & Testosterone)
Estrogen
- Inhibits osteoclast activity
- Maintains bone density
Testosterone
- Promotes bone formation
- Converted partly to estrogen in bone
Clinical Correlation
- Estrogen deficiency (post-menopause) → osteoporosis
- Important in alveolar bone preservation
Metabolic Disorders
Metabolic bone disorders arise due to disturbances in bone matrix formation, mineralization, or remodeling, often involving abnormalities in calcium, phosphate, vitamin D, hormones, or enzymes.
1. Rickets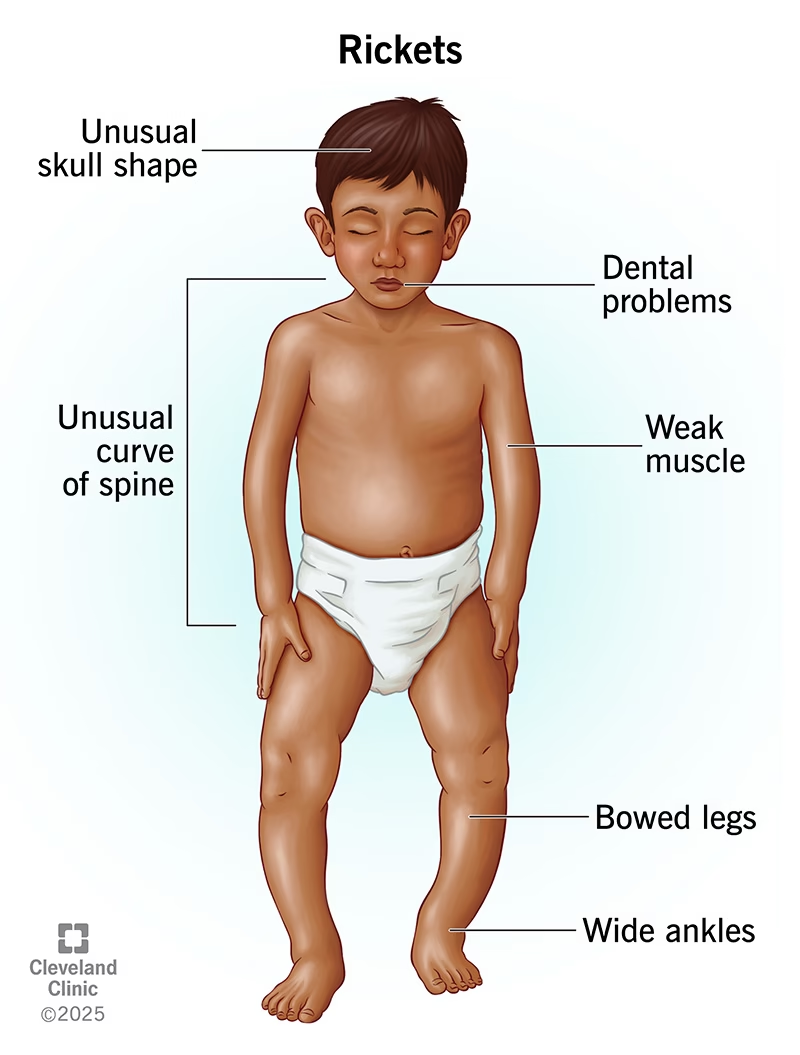
-
Age group: Children
-
Primary cause: Vitamin D deficiency
-
Biochemical defect:
-
Reduced intestinal absorption of calcium and phosphate
-
Defective mineralization of osteoid
-
-
Laboratory findings:
-
↓ Serum calcium (late)
-
↓ Serum phosphate
-
↑ Alkaline phosphatase
-
-
Clinical features:
-
Bone deformities (bowed legs)
-
Delayed tooth eruption
-
-
Dental relevance:
-
Defective alveolar bone formation
-
2. Osteomalacia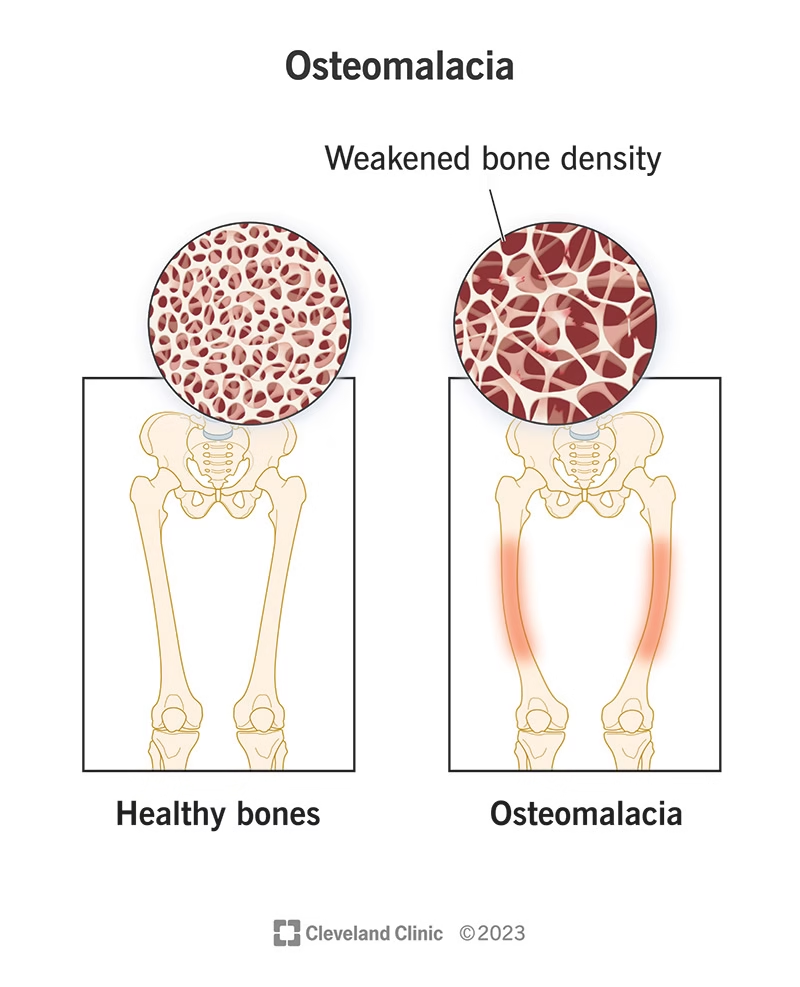
-
Age group: Adults
-
Primary cause: Vitamin D deficiency or phosphate deficiency
-
Biochemical defect:
-
Inadequate mineralization of bone matrix
-
-
Laboratory findings:
-
↓ Calcium
-
↓ Phosphate
-
↑ Alkaline phosphatase
-
-
Clinical features:
-
Bone pain
-
Increased fracture risk
-
-
Dental relevance:
-
Reduced bone density affecting implant stability
-
3. Osteoporosis
-
Primary cause:
-
Estrogen deficiency (post-menopause)
-
Aging, immobilization
-
-
Biochemical defect:
-
Decreased bone mass with normal mineralization
-
-
Laboratory findings:
-
Usually normal calcium and phosphate
-
-
Clinical features:
-
Fragile bones
-
Vertebral and hip fractures
-
-
Dental relevance:
-
Loss of alveolar bone
-
Increased tooth mobility
-
4. Hyperparathyroidism
-
Cause: Excess parathyroid hormone (PTH)
-
Biochemical defect:
-
Increased osteoclast-mediated bone resorption
-
-
Laboratory findings:
-
↑ Serum calcium
-
↓ Serum phosphate
-
↑ Alkaline phosphatase
-
-
Clinical features:
-
Bone pain
-
Osteitis fibrosa cystica
-
-
Dental relevance:
-
Jaw bone resorption
-
Loosening of teeth
-
5. Hypophosphatasia
-
Cause: Deficiency of alkaline phosphatase
-
Biochemical defect:
-
Failure of bone mineralization
-
-
Laboratory finding:
-
↓ Serum alkaline phosphatase
-
-
Clinical features:
-
Soft bones
-
Premature loss of teeth
-
-
Dental relevance:
-
Early exfoliation of deciduous teeth
-
6. Paget’s Disease of Bone
-
Biochemical defect:
-
Excessive and disorganized bone remodeling
-
-
Laboratory finding:
-
Markedly ↑ alkaline phosphatase
-
-
Clinical features:
-
Bone enlargement and deformity
-
-
Dental relevance:
-
Jaw enlargement
-
Malocclusion
-
MCQs
1. Bone is best described as:
A. Inert connective tissue
B. Specialized epithelial tissue
C. Metabolically active connective tissue
D. Muscular tissue
2. The major organic component of bone matrix is:
A. Elastin
B. Type I collagen
C. Type II collagen
D. Proteoglycan
3. The inorganic mineral of bone is mainly:
A. Calcium carbonate
B. Calcium phosphate
C. Hydroxyapatite
D. Calcium oxalate
4. Chemical formula of hydroxyapatite is:
A. Ca₃(PO₄)₂
B. Ca₁₀(PO₄)₆(OH)₂
C. CaCO₃
D. CaHPO₄
5. Percentage of inorganic matter in bone is approximately:
A. 20–30%
B. 30–40%
C. 50–55%
D. 65–70%
6. Organic matrix of bone is also called:
A. Osteon
B. Osteoid
C. Lamella
D. Canaliculus
7. Which bone cell is responsible for bone formation?
A. Osteoclast
B. Osteocyte
C. Osteoblast
D. Chondrocyte
8. Osteoclasts are derived from:
A. Mesenchymal stem cells
B. Osteoblast lineage
C. Monocyte–macrophage lineage
D. Fibroblasts
9. Which enzyme is a biochemical marker of bone formation?
A. Acid phosphatase
B. Alkaline phosphatase
C. Creatine kinase
D. Lactate dehydrogenase
10. Bone resorption involves secretion of:
A. Bicarbonate
B. Hydrochloric acid
C. Lactic acid
D. Sulfuric acid
11. Major collagen type in bone is:
A. Type II
B. Type III
C. Type I
D. Type IV
12. Bone mineralization begins in:
A. Osteocytes
B. Canaliculi
C. Matrix vesicles
D. Haversian canals
13. Matrix vesicles are rich in:
A. Acid phosphatase
B. Alkaline phosphatase
C. ATPase
D. Transaminases
14. Primary mineralization is characterized by:
A. Slow crystal growth
B. Rapid initial mineral deposition
C. Bone resorption
D. Osteoclast activation
15. Secondary mineralization leads to:
A. Bone softening
B. Increased bone density
C. Loss of collagen
D. Bone resorption
16. Vitamin D primarily increases:
A. Bone resorption
B. Renal phosphate excretion
C. Intestinal calcium absorption
D. Osteoclast apoptosis
17. Deficiency of vitamin D in children causes:
A. Osteomalacia
B. Osteoporosis
C. Rickets
D. Paget’s disease
18. Adult counterpart of rickets is:
A. Osteoporosis
B. Osteomalacia
C. Scurvy
D. Hypophosphatasia
19. Osteoporosis is characterized by:
A. Defective mineralization
B. Low bone mass with normal mineralization
C. Increased bone density
D. Excess collagen deposition
20. Serum calcium level in osteoporosis is usually:
A. Increased
B. Decreased
C. Normal
D. Zero
21. Hormone that increases serum calcium is:
A. Calcitonin
B. Parathyroid hormone
C. Estrogen
D. Thyroxine
22. PTH increases bone resorption by stimulating:
A. Osteocytes directly
B. Osteoclasts directly
C. Osteoblast-mediated RANKL release
D. Chondrocytes
23. Calcitonin is secreted by:
A. Parathyroid gland
B. Adrenal gland
C. Thyroid C cells
D. Pituitary gland
24. Effect of calcitonin on bone:
A. Increases resorption
B. Inhibits osteoclast activity
C. Increases calcium release
D. Inhibits mineralization
25. Estrogen deficiency leads to:
A. Increased bone formation
B. Reduced osteoclast activity
C. Increased bone resorption
D. Rickets
26. Growth hormone affects bone mainly via:
A. Calcitonin
B. Vitamin D
C. IGF-1
D. Parathyroid hormone
27. Which vitamin is required for osteocalcin activation?
A. Vitamin A
B. Vitamin C
C. Vitamin D
D. Vitamin K
28. Copper deficiency affects bone by impairing:
A. Collagen synthesis
B. Collagen cross-linking
C. Mineral deposition
D. Calcium absorption
29. Major function of inorganic bone matrix is:
A. Flexibility
B. Tensile strength
C. Hardness and rigidity
D. Elastic recoil
30. Major function of organic matrix is:
A. Compression resistance
B. Rigidity
C. Tensile strength and flexibility
D. Electrical conduction
31. Bone remodeling involves:
A. Only osteoblasts
B. Only osteoclasts
C. Balanced osteoblast and osteoclast activity
D. Osteocytes only
32. Alkaline phosphatase level is markedly increased in:
A. Osteoporosis
B. Rickets
C. Hypothyroidism
D. Scurvy
33. Hypophosphatasia is due to deficiency of:
A. Vitamin D
B. Calcium
C. Alkaline phosphatase
D. Phosphate
34. Early loss of teeth is seen in:
A. Osteoporosis
B. Rickets
C. Hypophosphatasia
D. Osteomalacia
35. Paget’s disease of bone shows:
A. Low ALP
B. Normal ALP
C. Markedly elevated ALP
D. No biochemical change
36. Which mineral strengthens bone and teeth?
A. Sodium
B. Potassium
C. Fluoride
D. Chloride
37. Bone acts as a reservoir mainly for:
A. Sodium and potassium
B. Calcium and phosphate
C. Magnesium and iron
D. Zinc and copper
38. Acid–base balance is maintained by bone through:
A. Protein synthesis
B. Buffering with bone salts
C. Hormone secretion
D. Enzyme activation
39. Osteocytes are mainly involved in:
A. Bone resorption
B. Bone formation
C. Bone maintenance and mechanosensing
D. Mineral absorption
40. Urinary hydroxyproline reflects:
A. Bone formation
B. Collagen synthesis
C. Collagen breakdown
D. Mineral deposition
41. Bone mineralization requires all EXCEPT:
A. Calcium
B. Phosphate
C. Alkaline phosphatase
D. Vitamin A
42. Which condition shows normal calcium but low bone mass?
A. Rickets
B. Osteomalacia
C. Osteoporosis
D. Hypoparathyroidism
43. Excess PTH causes:
A. Increased bone density
B. Osteitis fibrosa cystica
C. Reduced serum calcium
D. Inhibition of osteoclasts
44. Dental implant stability depends mainly on:
A. Enamel hardness
B. Dentin thickness
C. Alveolar bone quality
D. Cementum formation
45. Orthodontic tooth movement occurs due to:
A. Enamel resorption
B. Dentin remodeling
C. Bone remodeling
D. Pulp fibrosis
46. Bone softening in adults is termed:
A. Rickets
B. Osteoporosis
C. Osteomalacia
D. Scurvy
47. Osteocalcin is produced by:
A. Osteoclasts
B. Osteocytes
C. Osteoblasts
D. Fibroblasts
48. Which hormone decreases serum calcium?
A. PTH
B. Vitamin D
C. Calcitonin
D. Growth hormone
49. Bone chemistry is clinically important in dentistry because of:
A. Tooth color
B. Caries formation
C. Alveolar bone support
D. Saliva secretion
50. Bone is best described chemically as:
A. Pure mineral tissue
B. Pure protein tissue
C. Composite of organic and inorganic matrix
D. Fluid tissue
✅ Answer Key
-
C
-
B
-
C
-
B
-
D
-
B
-
C
-
C
-
B
-
B
-
C
-
C
-
B
-
B
-
B
-
C
-
C
-
B
-
B
-
C
-
B
-
C
-
C
-
B
-
C
-
C
-
D
-
B
-
C
-
C
-
C
-
B
-
C
-
C
-
C
-
C
-
B
-
B
-
C
-
C
-
D
-
C
-
B
-
C
-
C
-
C
-
C
-
C
-
C
-
C