Introduction
-
Cholesterol is a vital sterol lipid essential for normal structure and function of cell membranes, synthesis of steroid hormones, bile acids, and vitamin D.
-
The liver plays a central role in cholesterol metabolism, regulating its synthesis, utilization, storage, and transport through lipoproteins.
-
Disturbance in lipid metabolism leads to hypercholesterolemia, which is a major biochemical risk factor for atherosclerosis and coronary heart disease.
-
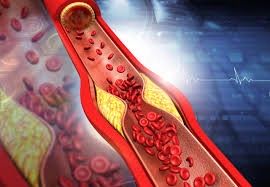
Atherosclerosis is a chronic inflammatory condition characterized by cholesterol and lipid deposition in arterial walls, resulting in reduced blood flow and ischemic complications.
-
Low-density lipoprotein (LDL) is atherogenic, whereas high-density lipoprotein (HDL) is cardioprotective, making lipid profile assessment clinically important.
-
Fatty liver disease develops due to abnormal accumulation of triglycerides in hepatocytes, commonly associated with metabolic disorders, malnutrition, and alcohol intake.
-
Lipotropic factors such as choline and methionine prevent fatty liver by promoting hepatic lipid mobilization and lipoprotein synthesis.
-
Lifestyle factors including diet, physical inactivity, obesity, and smoking significantly influence cholesterol levels and cardiovascular risk.
-
Dietary and lifestyle modifications are cornerstone preventive strategies for coronary heart disease and metabolic liver disorders.
-
Understanding cholesterol metabolism, atherosclerosis, and lipotropic factors is essential for prevention, diagnosis, and management of cardiovascular and hepatic diseases.
Cholesterol
-
Cholesterol is a sterol (steroid alcohol) containing a cyclopentanoperhydrophenanthrene nucleus with 27 carbon atoms.
-
It is an amphipathic molecule, having:
-
A hydroxyl (–OH) group → hydrophilic
-
A hydrocarbon ring and side chain → hydrophobic
-
-
Cholesterol is insoluble in water and therefore transported in plasma as lipoprotein complexes.
-
Sources of cholesterol:
-
Endogenous synthesis (70–80%) – mainly in the liver, intestine, adrenal cortex, and gonads
-
Dietary cholesterol (20–30%) – obtained from animal foods (eggs, milk, meat)
-
-
Site of synthesis:
-
Cytosol and endoplasmic reticulum of cells
-
Liver is the principal organ regulating whole-body cholesterol homeostasis
-
-
Rate-limiting step of synthesis:
-
Conversion of HMG-CoA to mevalonate
-
Catalyzed by HMG-CoA reductase (key regulatory enzyme)
-
-
Regulation of cholesterol synthesis:
-
Feedback inhibition by intracellular cholesterol
-
Hormonal control:
-
Insulin → increases synthesis
-
Glucagon → decreases synthesis
-
-
Inhibited by statin drugs
-
-
Plasma transport of cholesterol occurs via lipoproteins:
-
LDL → transports cholesterol from liver to peripheral tissues
-
HDL → removes excess cholesterol from tissues (reverse cholesterol transport)
-
-
Cholesterol exists in two forms in plasma:
-
Free cholesterol
-
Esterified cholesterol (cholesteryl esters)
-
-
Cholesterol esters are formed by:
-
LCAT enzyme in plasma
-
ACAT enzyme inside cells
-
-
Excretion of cholesterol:
-
Converted into bile acids and bile salts
-
Excreted via bile and feces
-
Cholesterol itself cannot be completely degraded to CO₂ and water
-
-
Physiological balance of synthesis, utilization, and excretion is essential to prevent hypercholesterolemia and atherosclerosis.
Functions of Cholesterol
-
Structural component of cell membranes
-
Cholesterol is an essential constituent of plasma membranes.
-
Maintains membrane fluidity, stability, and permeability.
-
Prevents excessive rigidity at low temperatures and excess fluidity at high temperatures.
-
-
Formation of lipid rafts
-
Cholesterol participates in lipid raft formation.
-
Lipid rafts are important for cell signaling, receptor function, and membrane trafficking.
-
-
Precursor of steroid hormones
-
Cholesterol is the parent molecule for all steroid hormones, including:
-
Glucocorticoids (cortisol)
-
Mineralocorticoids (aldosterone)
-
Sex hormones (estrogen, progesterone, testosterone)
-
-
-
Precursor of bile acids and bile salts
-
In the liver, cholesterol is converted into bile acids.
-
Bile salts aid in emulsification, digestion, and absorption of dietary fats and fat-soluble vitamins (A, D, E, K).
-
-
Precursor of vitamin D
-
7-dehydrocholesterol in skin is converted to vitamin D₃ on exposure to sunlight.
-
Vitamin D is essential for calcium and phosphorus homeostasis and bone health.
-
-
Role in nervous system
-
Cholesterol is a major component of myelin sheath.
-
Essential for rapid nerve impulse conduction and normal brain function.
-
-
Cell growth and differentiation
-
Cholesterol is required for cell division, growth, and tissue repair.
-
Plays a role in embryonic development.
-
-
Regulation of membrane-bound enzymes
-
Influences the activity of enzymes and receptors embedded in the cell membrane.
-
-
Source of biologically active molecules
-
Serves as a precursor for several biologically important molecules involved in metabolism and signaling.
-
-
Clinical relevance
-
Adequate cholesterol is essential for normal physiology.
-
Excess cholesterol, particularly LDL cholesterol, contributes to the development of atherosclerosis and coronary heart disease.
-
Atherosclerosis
Atherosclerosis is a chronic inflammatory disease of large and medium-sized arteries, characterized by lipid accumulation, fibrous plaque formation, and luminal narrowing, leading to ischemic heart disease and stroke.
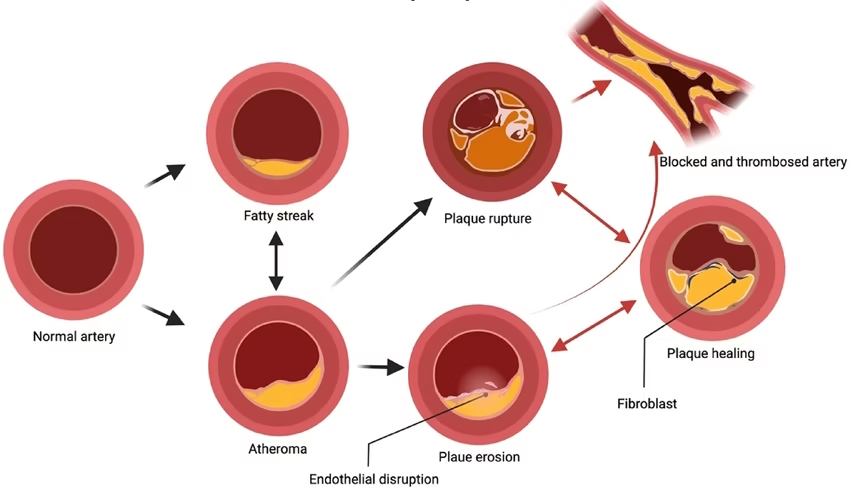
Pathogenesis of Atherosclerosis
-
Endothelial injury (smoking, diabetes, hypertension)
-
Increased permeability to LDL
-
Oxidation of LDL in subendothelial space
-
Macrophage uptake via scavenger receptors
-
Formation of foam cells
-
Development of fatty streaks
-
Smooth muscle proliferation
-
Fibrous plaque → arterial narrowing
Molecules Involved
-
Oxidized LDL
-
Cytokines (IL-1, TNF-α)
-
Adhesion molecules
-
Reactive oxygen species
Clinical Consequences
Atherosclerosis leads to progressive narrowing and hardening of arteries, resulting in reduced blood supply to vital organs.
1. Coronary Artery Disease (CAD)
-
Most common and serious consequence
-
Reduced blood flow to myocardium
-
Leads to:
-
Angina pectoris
-
Myocardial infarction (heart attack)
-
Sudden cardiac death
-
2. Cerebrovascular Disease
-
Atherosclerosis of carotid and cerebral arteries
-
Causes:
-
Transient ischemic attack (TIA)
-
Ischemic stroke
-
Cognitive impairment
-
3. Peripheral Arterial Disease (PAD)
-
Affects arteries of lower limbs
-
Clinical features:
-
Intermittent claudication
-
Rest pain
-
Non-healing ulcers
-
Gangrene
-
4. Renal Artery Atherosclerosis
-
Reduced renal blood flow
-
Causes:
-
Secondary hypertension
-
Chronic kidney disease
-
5. Aortic Atherosclerosis
-
Weakening of arterial wall
-
Leads to:
-
Aortic aneurysm
-
Aortic dissection
-
6. Thromboembolism
-
Rupture of atherosclerotic plaque
-
Platelet aggregation and thrombus formation
-
Acute vascular occlusion
Risk Factors
A. Non-Modifiable Risk Factors
-
Age – risk increases with advancing age
-
Sex – males are at higher risk; post-menopausal females also vulnerable
-
Genetic predisposition – family history of cardiovascular disease
-
Ethnicity – higher prevalence in certain populations
B. Modifiable Risk Factors
-
Hyperlipidemia
-
Increased LDL-cholesterol
-
Decreased HDL-cholesterol
-
-
Hypertension
-
Causes endothelial damage
-
-
Diabetes mellitus
-
Increases LDL oxidation
-
Accelerates plaque formation
-
-
Smoking
-
Increases oxidative stress
-
Reduces HDL
-
-
Obesity
-
Associated with dyslipidemia and insulin resistance
-
-
Sedentary lifestyle
-
Unhealthy diet
-
High saturated fat and trans fat intake
-
-
Psychological stress
-
Alcohol abuse
Prevention
Prevention focuses on risk factor modification, lifestyle changes, and dietary control.
A. Lifestyle Modifications
-
Regular physical activity (30–45 minutes/day)
-
Weight reduction and maintenance of normal BMI
-
Smoking cessation
-
Stress management (yoga, meditation)
-
Adequate sleep
-
Regular health check-ups
B. Dietary Modifications
-
Reduce intake of:
-
Saturated fats
-
Trans fats
-
Cholesterol-rich foods
-
-
Increase intake of:
-
Fruits and vegetables (antioxidants)
-
Whole grains (dietary fiber)
-
Omega-3 fatty acids (cardioprotective)
-
-
Prefer:
-
Unsaturated fats over saturated fats
-
-
Limit refined sugars and processed foods
C. Control of Metabolic Disorders
-
Proper management of:
-
Diabetes mellitus
-
Hypertension
-
Dyslipidemia
-
-
Regular lipid profile monitoring
D. Pharmacological Prevention (High-Risk Individuals)
-
Statins (reduce LDL-cholesterol)
-
Antihypertensive drugs
-
Antiplatelet therapy (as advised)
-
Glycemic control medications
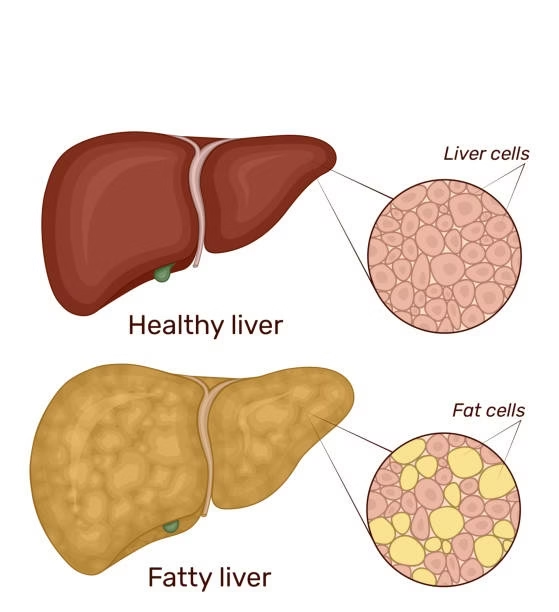
Hepatic Steatosis
-
Fatty liver is a metabolic disorder characterized by abnormal accumulation of triglycerides within hepatocytes.
-
Normally, fat content of liver is <5% of liver weight; values above this indicate fatty liver.
-
It is a reversible condition in early stages, but may progress to inflammation, fibrosis, and cirrhosis if untreated.
Types of Fatty Liver
1. Alcoholic Fatty Liver Disease (AFLD)
-
Caused by chronic alcohol consumption
-
Alcohol increases NADH/NAD⁺ ratio
-
Inhibits fatty acid oxidation
-
Leads to triglyceride accumulation
2. Non-Alcoholic Fatty Liver Disease (NAFLD)
-
Occurs in non-alcoholics
-
Associated with:
-
Obesity
-
Type 2 diabetes mellitus
-
Dyslipidemia
-
Metabolic syndrome
-
-
Most common form in modern population
3. Nutritional Fatty Liver
-
Due to protein malnutrition
-
Deficiency of lipotropic factors
-
Seen in:
-
Kwashiorkor
-
Prolonged starvation
-
4. Drug- and Toxin-Induced Fatty Liver
-
Caused by drugs like:
-
Tetracycline
-
Corticosteroids
-
Chemotherapeutic agents
-
-
Exposure to toxins (carbon tetrachloride)
5. Pregnancy-Related Fatty Liver
-
Rare but severe
-
Due to mitochondrial dysfunction of fatty acid oxidation
Biochemical Basis of Fatty Liver
Fatty liver develops due to imbalance between lipid synthesis, utilization, and export.
Major Biochemical Mechanisms
-
Increased Fatty Acid Influx
-
Excess free fatty acids from adipose tissue
-
Common in obesity and diabetes
-
-
Increased Triglyceride Synthesis
-
Excess acetyl-CoA converted to fatty acids
-
Enhanced esterification in hepatocytes
-
-
Decreased β-Oxidation
-
Alcohol and toxins inhibit mitochondrial oxidation
-
Reduced fatty acid breakdown
-
-
Defective Lipoprotein Synthesis
-
Reduced synthesis of apoproteins
-
Impaired VLDL formation
-
-
Impaired Lipid Export
-
Triglycerides not transported out of liver
-
Accumulate within hepatocytes
-
-
Deficiency of Lipotropic Factors
-
Reduced phospholipid synthesis
-
Failure of triglyceride mobilization
-
Lipotropic Factors
-
Lipotropic factors are substances that promote removal of fat from the liver by enhancing lipid transport and metabolism.
-
They prevent or correct fatty liver.
Important Lipotropic Factors
| Lipotropic Factor | Biochemical Role |
|---|---|
| Choline | Phosphatidylcholine synthesis |
| Methionine | Methyl group donor |
| Inositol | Lipoprotein synthesis |
| Betaine | Transmethylation reactions |
| Vitamin B12 | One-carbon metabolism |
| Folic acid | Methyl transfer reactions |
| Protein | Apoprotein synthesis |
Mechanism of Action of Lipotropic Factors
-
Enhance synthesis of phospholipids, especially phosphatidylcholine
-
Promote formation of VLDL particles
-
Facilitate export of triglycerides from liver to circulation
-
Improve hepatic lipid mobilization
-
Prevent intracellular fat accumulation
-
Maintain normal liver structure and function
In deficiency states → triglycerides remain trapped in liver → fatty liver develops
Clinical Significance
-
Fatty liver is one of the earliest manifestations of metabolic disorders
-
Early diagnosis prevents progression to:
-
Steatohepatitis
-
Fibrosis
-
Cirrhosis
-
Hepatocellular carcinoma
-
-
Lipotropic factors have:
-
Preventive role in fatty liver
-
Therapeutic importance in malnutrition
-
-
Lifestyle modification and dietary correction are essential
-
Biochemically important in:
-
Diabetes
-
Obesity
-
Alcoholism
-
Cardiovascular risk assessment
-
MCQs
1. Cholesterol is best described as a
A. Fatty acid
B. Phospholipid
C. Sterol
D. Triglyceride
Answer: C
2. The major site of cholesterol synthesis is
A. Kidney
B. Liver
C. Muscle
D. Brain
Answer: B
3. Rate-limiting enzyme in cholesterol synthesis is
A. Acetyl-CoA carboxylase
B. HMG-CoA reductase
C. LCAT
D. ACAT
Answer: B
4. LDL cholesterol is termed atherogenic because it
A. Removes cholesterol from tissues
B. Transports cholesterol to tissues
C. Inhibits plaque formation
D. Activates lipoprotein lipase
Answer: B
5. HDL cholesterol is protective due to its role in
A. Fat absorption
B. Reverse cholesterol transport
C. Triglyceride synthesis
D. LDL oxidation
Answer: B
6. Normal total cholesterol level is
A. <150 mg/dL
B. <180 mg/dL
C. <200 mg/dL
D. <250 mg/dL
Answer: C
7. Cholesterol is a precursor of all except
A. Steroid hormones
B. Bile acids
C. Vitamin D
D. Insulin
Answer: D
8. Atherosclerosis primarily affects
A. Veins
B. Capillaries
C. Large and medium arteries
D. Lymphatics
Answer: C
9. Initial lesion of atherosclerosis is
A. Fibrous plaque
B. Thrombus
C. Fatty streak
D. Calcification
Answer: C
10. Foam cells are derived from
A. Neutrophils
B. Macrophages
C. Lymphocytes
D. Platelets
Answer: B
11. Oxidized LDL contributes to atherosclerosis by
A. Reducing inflammation
B. Activating macrophage scavenger receptors
C. Increasing HDL synthesis
D. Inhibiting platelet aggregation
Answer: B
12. Major lipid present in atherosclerotic plaque is
A. Phospholipid
B. Triglyceride
C. Cholesteryl ester
D. Free fatty acid
Answer: C
13. Most common clinical consequence of atherosclerosis is
A. Renal failure
B. Coronary heart disease
C. Liver cirrhosis
D. Anemia
Answer: B
14. Angina pectoris results from
A. Complete coronary occlusion
B. Reduced myocardial blood supply
C. Valve stenosis
D. Arrhythmia
Answer: B
15. A non-modifiable risk factor for atherosclerosis is
A. Smoking
B. Obesity
C. Age
D. Diet
Answer: C
16. Smoking increases atherosclerosis by
A. Increasing HDL
B. Reducing oxidative stress
C. Causing endothelial damage
D. Lowering LDL
Answer: C
17. Diabetes mellitus accelerates atherosclerosis due to
A. Hypoglycemia
B. Increased LDL oxidation
C. Increased HDL
D. Reduced inflammation
Answer: B
18. Best lifestyle measure to increase HDL is
A. High sugar intake
B. Regular physical exercise
C. Smoking
D. Trans fats
Answer: B
19. Omega-3 fatty acids are beneficial because they
A. Increase LDL
B. Reduce inflammation and triglycerides
C. Promote plaque formation
D. Increase cholesterol synthesis
Answer: B
20. Coronary heart disease prevention primarily involves
A. Surgery
B. Lifestyle modification
C. Antibiotics
D. Steroids
Answer: B
21. Fatty liver is characterized by accumulation of
A. Cholesterol
B. Phospholipids
C. Triglycerides
D. Free glucose
Answer: C
22. Normal fat content of liver is
A. <2%
B. <5%
C. <10%
D. <15%
Answer: B
23. Most common type of fatty liver worldwide is
A. Alcoholic fatty liver
B. Drug-induced fatty liver
C. Non-alcoholic fatty liver disease
D. Pregnancy-related fatty liver
Answer: C
24. Alcohol causes fatty liver mainly by
A. Increasing β-oxidation
B. Decreasing NADH
C. Increasing NADH/NAD⁺ ratio
D. Increasing lipoprotein export
Answer: C
25. NAFLD is commonly associated with
A. Tuberculosis
B. Metabolic syndrome
C. Anemia
D. Vitamin A deficiency
Answer: B
26. Fatty liver is reversible in
A. All stages
B. Early stages
C. Cirrhosis
D. Hepatocellular carcinoma
Answer: B
27. Increased free fatty acid influx to liver occurs in
A. Starvation
B. Obesity
C. Hypothyroidism
D. All of the above
Answer: D
28. Defective VLDL formation leads to
A. Hypolipidemia
B. Fatty liver
C. Increased HDL
D. Ketosis
Answer: B
29. Lipotropic factors primarily prevent fatty liver by
A. Increasing fat intake
B. Inhibiting triglyceride synthesis
C. Enhancing lipid export from liver
D. Decreasing bile secretion
Answer: C
30. Most important lipotropic factor is
A. Vitamin C
B. Choline
C. Vitamin A
D. Calcium
Answer: B
31. Choline deficiency leads to fatty liver due to impaired
A. β-oxidation
B. Phospholipid synthesis
C. Glycogen synthesis
D. Cholesterol excretion
Answer: B
32. Methionine acts as a lipotropic factor by
A. Acting as antioxidant
B. Providing methyl groups
C. Reducing cholesterol absorption
D. Inhibiting LDL
Answer: B
33. Vitamin B12 is important in fatty liver prevention due to
A. Energy production
B. One-carbon metabolism
C. Calcium absorption
D. Antioxidant activity
Answer: B
34. Inositol helps prevent fatty liver by
A. Enhancing bile secretion
B. Promoting lipoprotein synthesis
C. Increasing insulin secretion
D. Decreasing fatty acid uptake
Answer: B
35. Protein deficiency causes fatty liver due to
A. Increased oxidation
B. Decreased apoprotein synthesis
C. Increased bile acid formation
D. Increased HDL
Answer: B
36. Fatty liver seen in malnutrition is due to deficiency of
A. Carbohydrates
B. Lipotropic factors
C. Fat-soluble vitamins
D. Electrolytes
Answer: B
37. Lipotropic factors mainly help in formation of
A. LDL
B. HDL
C. VLDL
D. Chylomicrons
Answer: C
38. Failure of triglyceride export results in
A. Hypolipidemia
B. Hepatic steatosis
C. Atherosclerosis
D. Ketosis
Answer: B
39. Early fatty liver is usually
A. Irreversible
B. Asymptomatic
C. Painful
D. Fatal
Answer: B
40. Long-standing fatty liver may progress to
A. Hepatitis
B. Fibrosis
C. Cirrhosis
D. All of the above
Answer: D
41. Best dietary approach to prevent fatty liver is
A. High fat diet
B. Balanced diet with adequate protein
C. High sugar intake
D. Fasting
Answer: B
42. HDL protects against atherosclerosis by
A. Increasing LDL uptake
B. Removing cholesterol from plaques
C. Increasing triglycerides
D. Causing vasoconstriction
Answer: B
43. Statins reduce cholesterol by inhibiting
A. ACAT
B. LCAT
C. HMG-CoA reductase
D. Lipoprotein lipase
Answer: C
44. Atherosclerosis is now considered a
A. Pure lipid disorder
B. Infectious disease
C. Chronic inflammatory disease
D. Genetic disorder only
Answer: C
45. Major dietary risk factor for CHD is
A. Fiber
B. Omega-3 fatty acids
C. Saturated and trans fats
D. Antioxidants
Answer: C
46. Peripheral arterial disease commonly presents as
A. Chest pain
B. Shortness of breath
C. Intermittent claudication
D. Jaundice
Answer: C
47. Lipotropic factors are especially important in
A. Kidney diseases
B. Liver disorders
C. Lung diseases
D. Brain tumors
Answer: B
48. Reverse cholesterol transport is mediated mainly by
A. LDL
B. VLDL
C. HDL
D. Chylomicrons
Answer: C
49. Most effective preventive strategy for CHD is
A. Drugs alone
B. Surgery
C. Early lifestyle modification
D. Antibiotics
Answer: C
50. Key biochemical event in atherosclerosis initiation is
A. Cholesterol synthesis
B. LDL oxidation
C. HDL formation
D. Triglyceride hydrolysis
Answer: B