Introduction
-
DiGeorge Syndrome (DGS) is a genetic disorder caused by a deletion on chromosome 22 (22q11.2 deletion).
-
It affects the development of the thymus, parathyroid glands, and heart, leading to immune deficiency, low calcium levels, and congenital heart defects.
-
The syndrome is part of a group of conditions known as 22q11.2 deletion syndromes, which also include Velocardiofacial syndrome and Conotruncal anomaly face syndrome.
-
It was first described by Dr. Angelo DiGeorge in 1965.
-
The condition varies in severity — some patients have mild symptoms, while others have life-threatening complications.
Genetic Basis (Cause)
| Feature | Details |
|---|---|
| Chromosomal abnormality | Deletion in chromosome 22 at band q11.2 |
| Type of mutation | Microdeletion (small piece of DNA missing) |
| Inheritance pattern | Autosomal dominant (but 90% are new mutations) |
| Genes involved | TBX1 gene is the most critical for symptoms |
| Recurrence risk | ~50% if one parent carries the deletion |
-
The missing region on chromosome 22 contains genes needed for the normal development of the thymus, parathyroid glands, and parts of the heart.
-
The deletion leads to:
-
T-cell deficiency due to thymic hypoplasia.
-
Hypocalcemia (low calcium) due to parathyroid underdevelopment.
-
Congenital heart defects due to abnormal heart formation.
-
Epidemiology
| Parameter | Details |
|---|---|
| Incidence | 1 in 4,000 live births |
| Gender | Affects both equally |
| Inheritance | Mostly sporadic (new mutations) |
| Risk factor | Parental 22q11.2 deletion (inherited cases) |
Clinical Features
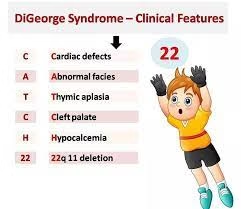
DiGeorge Syndrome affects multiple organ systems — remember the triad:
Cardiac defects + Hypocalcemia + Immune deficiency
A. Classic Triad
| System | Defect | Consequence |
|---|---|---|
| Thymus | Hypoplasia / Aplasia | ↓ T-cell production → Immunodeficiency |
| Parathyroid | Hypoplasia | ↓ PTH → Hypocalcemia → Tetany, seizures |
| Heart | Conotruncal defects | Cyanotic congenital heart disease |
B. Detailed Clinical Features
| Category | Features |
|---|---|
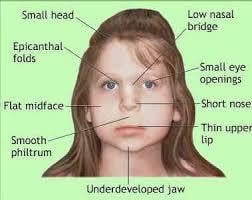
| Facial features | Small mouth, cleft palate, low-set ears, hypertelorism (wide eyes), micrognathia (small jaw) |
| Cardiac defects | Tetralogy of Fallot, Interrupted aortic arch, Truncus arteriosus, VSD |
| Immune system | Recurrent infections due to T-cell deficiency |
| Endocrine | Hypocalcemia, tetany, seizures due to low parathyroid hormone |
| Growth & Development | Delayed milestones, poor growth, learning disabilities |
| Psychiatric | Anxiety, ADHD, depression, schizophrenia (in older patients) |
| Renal / Skeletal | Kidney anomalies, scoliosis, skeletal malformations |
Pathophysiology
| Affected Organ | Result of Deletion |
|---|---|
| Thymus | Reduced T-lymphocyte production → immune deficiency |
| Parathyroid glands | Decreased PTH → hypocalcemia, muscle cramps |
| Heart (conotruncal region) | Defective cardiac septation → congenital heart disease |
| Face and palate | Abnormal neural crest cell migration → facial deformities |
Diagnosis
1. Clinical Evaluation
-
Characteristic facial appearance
-
Recurrent infections
-
Hypocalcemia symptoms (muscle spasms, seizures)
-
Congenital heart defects on echocardiography
2. Laboratory Tests
| Test | Findings |
|---|---|
| Serum calcium | ↓ Decreased |
| Parathyroid hormone (PTH) | ↓ Decreased |
| Lymphocyte count | ↓ T-lymphocytes (CD3+) |
| Immunoglobulin levels | May be normal or slightly low |
| Chest X-ray | Small or absent thymic shadow |
3. Genetic Tests
| Test | Purpose |
|---|---|
| FISH (Fluorescence in situ hybridization) | Detects 22q11.2 deletion |
| Microarray / MLPA | Confirms microdeletion |
| Prenatal diagnosis | Possible through amniocentesis if family history present |
Differential Diagnosis
| Condition | Difference from DGS |
|---|---|
| SCID (Severe Combined Immunodeficiency) | Both T and B cell defects |
| Hypoparathyroidism (non-genetic) | No thymic defect |
| Velocardiofacial syndrome | Overlaps but with mild immune defects |
Management
There is no cure, but early treatment can correct many problems.
1. Medical Management
| Problem | Treatment |
|---|---|
| Hypocalcemia | Calcium and vitamin D supplements |
| Heart defects | Surgical repair of cardiac malformations |
| Immunodeficiency | Antibiotics, avoidance of live vaccines, thymus or bone marrow transplant in severe cases |
| Endocrine abnormalities | Lifelong monitoring of calcium and thyroid function |
| Seizures | Anti-epileptic drugs if needed |
2. Supportive Care
-
Speech and occupational therapy for learning and speech delays
-
Psychological counseling for behavioral problems
-
Regular follow-up for cardiac, endocrine, and immune function
3. Genetic Counselling
| Aspect | Details |
|---|---|
| Recurrence risk | 50% if one parent carries the deletion |
| Testing | Chromosome analysis for parents |
| Prenatal testing | FISH or microarray during pregnancy |
| Family advice | Genetic counselling before the next pregnancy |
Prognosis
| Severity | Outcome |
|---|---|
| Mild immune deficiency | Near normal life expectancy with treatment |
| Severe thymic aplasia | Life-threatening infections in infancy |
| Heart defects | Correctable by surgery |
| Neurodevelopmental delay | Improved by therapy and education |
MCQs
-
DiGeorge Syndrome is caused by a deletion in which chromosome?
A. Chromosome 13
B. Chromosome 18
C. Chromosome 22
D. Chromosome 21 -
The exact chromosomal location of the deletion in DiGeorge Syndrome is:
A. 22q11.2
B. 21q22
C. 13q14
D. 15q11 -
DiGeorge Syndrome is also known as:
A. Turner Syndrome
B. Velocardiofacial Syndrome
C. Edwards Syndrome
D. Cri-du-chat Syndrome -
The major organ systems affected in DiGeorge Syndrome include:
A. Liver and spleen
B. Thymus, heart, and parathyroid
C. Brain and kidneys
D. Skin and pancreas -
Which embryological structure is mainly affected in DiGeorge Syndrome?
A. 1st pharyngeal pouch
B. 2nd pharyngeal pouch
C. 3rd and 4th pharyngeal pouches
D. 5th pharyngeal pouch -
Defective development of the thymus in DiGeorge Syndrome leads to:
A. T-cell deficiency
B. B-cell deficiency
C. Both T and B cell deficiency
D. NK cell deficiency -
Hypocalcemia in DiGeorge Syndrome is due to:
A. Vitamin D deficiency
B. Hypoparathyroidism
C. Renal failure
D. Pancreatic insufficiency -
The most common cardiac defect in DiGeorge Syndrome is:
A. Atrial septal defect
B. Tetralogy of Fallot
C. Mitral valve prolapse
D. Patent ductus arteriosus -
Which gene is mainly responsible for DiGeorge Syndrome features?
A. BRCA1
B. TBX1
C. TP53
D. CFTR -
Which of the following best describes the inheritance pattern of DiGeorge Syndrome?
A. Autosomal recessive
B. Autosomal dominant
C. X-linked
D. Multifactorial -
Most cases of DiGeorge Syndrome occur due to:
A. Viral infection
B. New spontaneous mutation (de novo)
C. Radiation exposure
D. Drug toxicity -
The triad of DiGeorge Syndrome includes:
A. Cardiac defects, hypocalcemia, and immune deficiency
B. Renal failure, anemia, and edema
C. Diabetes, obesity, and hypertension
D. Skin rash, fever, and cough -
The thymus in DiGeorge Syndrome is usually:
A. Enlarged
B. Normal
C. Hypoplastic or absent
D. Inflamed -
The chest X-ray of a DiGeorge patient typically shows:
A. Enlarged thymic shadow
B. Absent thymic shadow
C. Calcified thymus
D. Normal findings -
Which immune cells are reduced in DiGeorge Syndrome?
A. Neutrophils
B. T-lymphocytes
C. B-lymphocytes
D. Platelets -
Hypocalcemia in DiGeorge Syndrome can lead to:
A. Tetany and seizures
B. Jaundice
C. Anemia
D. Muscle hypertrophy -
The facial appearance of a child with DiGeorge Syndrome may show:
A. Cleft palate and low-set ears
B. Large tongue and flat face
C. Bulging eyes and high nasal bridge
D. Thick lips and wide mouth -
Which diagnostic test confirms 22q11.2 deletion?
A. ELISA
B. FISH (Fluorescence In Situ Hybridization)
C. Karyotyping only
D. Coombs test -
What is the most common cause of death in untreated DiGeorge Syndrome?
A. Cardiac defect and infection
B. Anemia
C. Dehydration
D. Renal stones -
The main immunological defect in DiGeorge Syndrome is due to absence of:
A. Bone marrow
B. Thymus
C. Spleen
D. Lymph nodes -
Which endocrine gland is underdeveloped in DiGeorge Syndrome?
A. Thyroid
B. Parathyroid
C. Adrenal
D. Pituitary -
Parathyroid gland hypoplasia in DiGeorge Syndrome results in:
A. Hypercalcemia
B. Hypocalcemia
C. Hyperkalemia
D. Hypoglycemia -
Which of the following is a mnemonic for remembering DiGeorge Syndrome features?
A. CATCH-22
B. WAGR
C. CAH
D. TORCH -
In the mnemonic CATCH-22, “C” stands for:
A. Cleft lip
B. Cardiac defects
C. Cataract
D. Cystic fibrosis -
The “T” in CATCH-22 represents:
A. Thymic hypoplasia
B. Thyroid enlargement
C. Tetanus
D. Tumor formation -
The “H” in CATCH-22 stands for:
A. Hypocalcemia
B. Hypothyroidism
C. Hypertension
D. Hyperglycemia -
Which cardiac defect is commonly associated with DiGeorge Syndrome?
A. Truncus arteriosus
B. Mitral stenosis
C. Aortic regurgitation
D. Coarctation of aorta -
The most likely electrolyte imbalance in DiGeorge Syndrome is:
A. High calcium
B. Low calcium
C. High sodium
D. Low potassium -
In DiGeorge Syndrome, which type of infections are most frequent?
A. Viral and fungal infections
B. Bacterial only
C. Parasitic
D. Protozoal -
Which of the following laboratory findings supports the diagnosis?
A. High calcium, low PTH
B. Low calcium, low PTH
C. Low calcium, high PTH
D. Normal calcium, high PTH -
The FISH test detects deletion on chromosome 22 by using:
A. Radiolabeled isotopes
B. Fluorescent DNA probes
C. Enzyme-linked antibodies
D. Histological staining -
The recurrence risk if one parent carries 22q11.2 deletion is:
A. 0%
B. 10%
C. 25%
D. 50% -
Children with DiGeorge Syndrome should avoid:
A. Inactivated vaccines
B. Live attenuated vaccines
C. Vitamin D supplements
D. Calcium intake -
Which treatment is used to correct hypocalcemia in DiGeorge Syndrome?
A. Iron supplements
B. Calcium and Vitamin D therapy
C. Insulin therapy
D. Antihistamines -
Prognosis of DiGeorge Syndrome mainly depends on:
A. Severity of heart defects and immune deficiency
B. Hair color
C. Eye color
D. Height of patient
Answer Key
-
C — Chromosome 22
-
A — 22q11.2
-
B — Velocardiofacial Syndrome
-
B — Thymus, heart, and parathyroid
-
C — 3rd and 4th pharyngeal pouches
-
A — T-cell deficiency
-
B — Hypoparathyroidism
-
B — Tetralogy of Fallot
-
B — TBX1
-
B — Autosomal dominant
-
B — New spontaneous mutation (de novo)
-
A — Cardiac defects, hypocalcemia, and immune deficiency
-
C — Hypoplastic or absent
-
B — Absent thymic shadow
-
B — T-lymphocytes
-
A — Tetany and seizures
-
A — Cleft palate and low-set ears
-
B — FISH (Fluorescence In Situ Hybridization)
-
A — Cardiac defect and infection
-
B — Thymus
-
B — Parathyroid
-
B — Hypocalcemia
-
A — CATCH-22
-
B — Cardiac defects
-
A — Thymic hypoplasia
-
A — Hypocalcemia
-
A — Truncus arteriosus
-
B — Low calcium
-
A — Viral and fungal infections
-
B — Low calcium, low PTH
-
B — Fluorescent DNA probes
-
D — 50%
-
B — Live attenuated vaccines
-
B — Calcium and Vitamin D therapy
-
A — Severity of heart defects and immune deficiency