Introduction
-
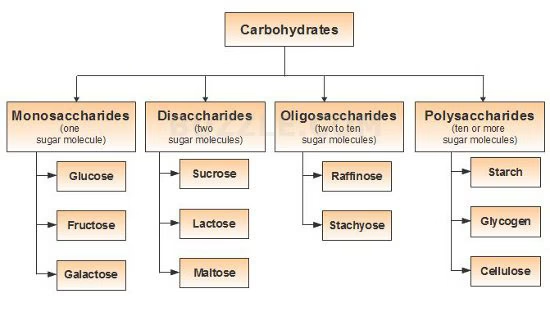
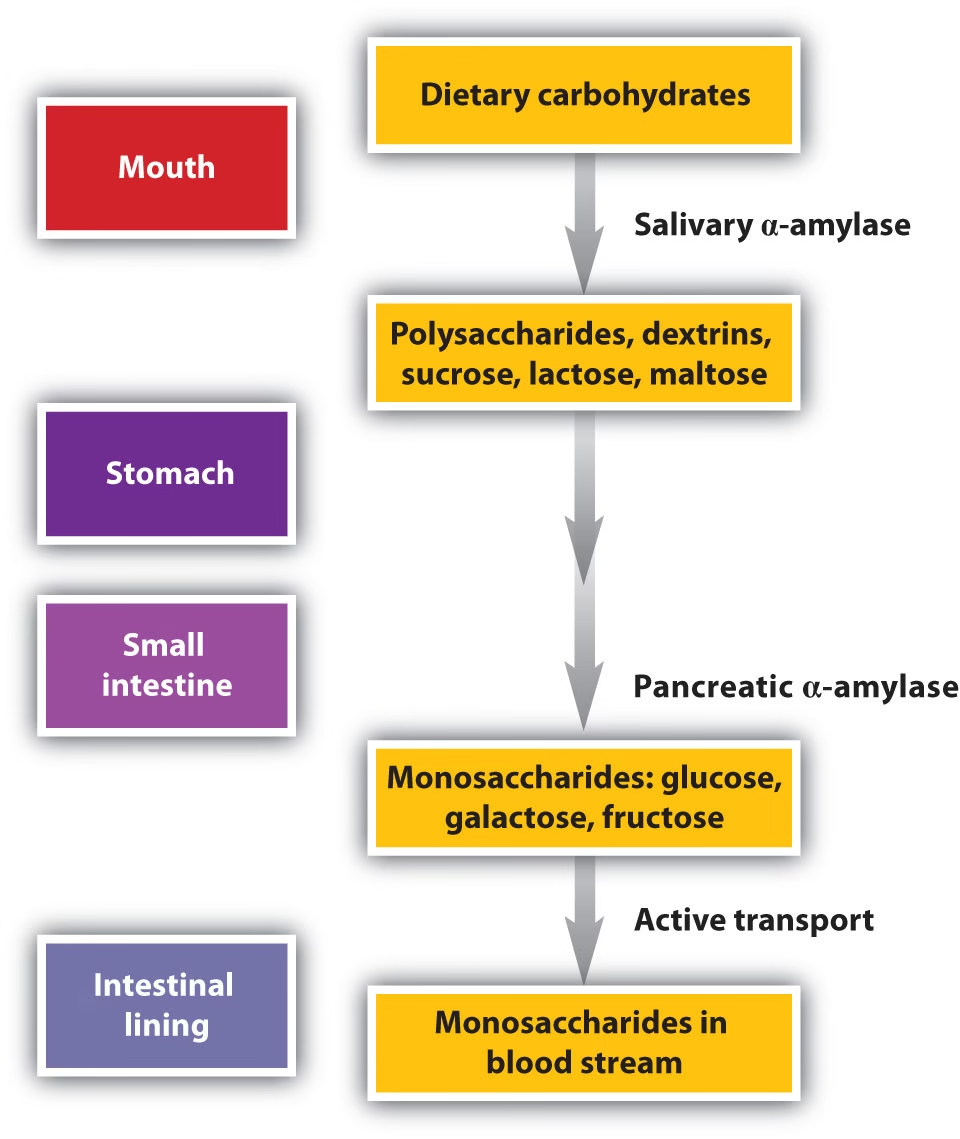
Carbohydrates are a major dietary energy source and must be broken into simple sugars before absorption.
-
The diet contains starches, disaccharides, and sugars, but only monosaccharides can be taken up by the intestine.
-
Digestion begins in the mouth and is completed in the small intestine through salivary, pancreatic, and brush-border enzymes.
-
These enzymes convert complex carbohydrates into glucose, fructose, and galactose.
-
Absorption occurs through specific transporters on intestinal cells using active and facilitated mechanisms.
-
The efficiency of this process depends on enzyme activity, pancreatic function, and intestinal mucosal health.
-
Any defect in enzymes or transporters leads to carbohydrate malabsorption and related clinical symptoms.
Composition of Dietary Carbohydrates
The carbohydrates consumed in a typical diet belong to different categories:
Polysaccharides
-
Starch (amylose, amylopectin) – major plant carbohydrate
-
Glycogen – animal storage form
-
Dextrins – partially digested starch fragments
Disaccharides
-
Sucrose → Glucose + Fructose
-
Lactose → Glucose + Galactose
-
Maltose → Glucose + Glucose
Monosaccharides
-
Glucose, fructose, galactose – directly absorbable
Non-digestible carbohydrates (Dietary fiber)
-
Cellulose
-
Hemicellulose
-
Pectins
-
Beta-glucans
These fibers contribute to gut health, stool bulk, slower glucose absorption, and a balanced microbiome.
Important Note:
Only monosaccharides are absorbed into the bloodstream; all complex carbohydrates must be broken down.
Digestion of Carbohydrates
Carbohydrate digestion involves three major phases: oral, gastric, and intestinal.
A. Oral Phase: Initial Hydrolysis
1. Enzyme Involved
Salivary α-Amylase (Ptyalin)
-
Secreted by the parotid and submandibular glands.
-
Optimal pH: 6.7–7.0 (neutral).
-
Inactivated when food reaches the acidic environment of the stomach (pH < 4).
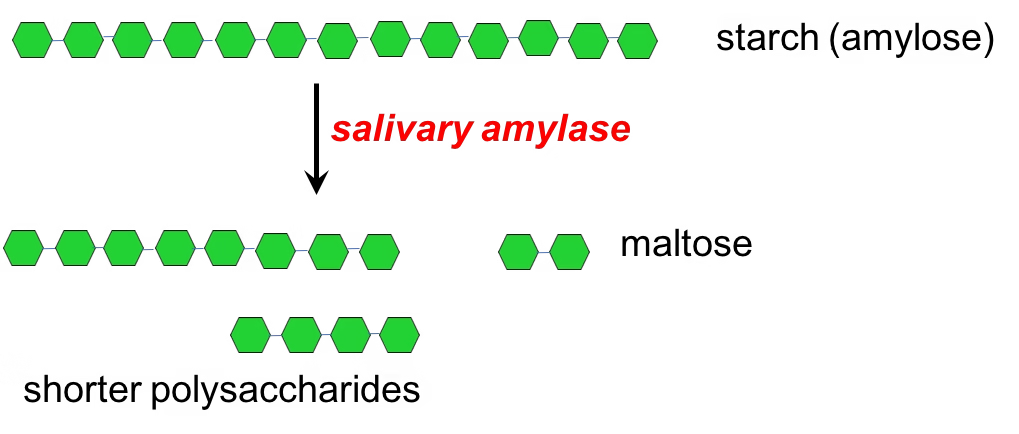
2. Substrate and Action
Acts on Starch (Amylose & Amylopectin)
-
Breaks internal α-1,4-glycosidic bonds in polysaccharides.
-
Does NOT act on:
-
α-1,6 bonds of branch points
-
Cellulose
-
Disaccharides (lactose, sucrose, maltose)
-
3. Products Formed
-
Maltose (disaccharide)
-
Maltotriose (trisaccharide)
-
α-Limit dextrins (small branched fragments)
These products require further digestion by intestinal enzymes.
4. Role of Mechanical Processing
-
Chewing (mastication) increases surface area of food.
-
Mixes amylase with food for efficient hydrolysis.
-
Forms a moist bolus that is easier to swallow.
5. Duration and Importance
-
Digestion in the mouth lasts only a few seconds.
-
Some activity continues briefly in the upper stomach until amylase is inactivated.
-
Although limited, this step primes carbohydrates for rapid digestion in the small intestine.
B. Gastric Phase: Mixing and Acid Inactivation
1. No Carbohydrate-Digesting Enzymes
-
The stomach does not secrete enzymes that hydrolyze carbohydrates.
-
No amylase, sucrase, maltase, or lactase are produced by gastric mucosa.
2. Inactivation of Salivary α-Amylase
-
Food mixed with gastric acid (pH < 4) causes rapid inactivation of salivary α-amylase.
-
Any starch digestion that began in the mouth ends within minutes of entering the stomach.
3. Mechanical Mixing (Churning)
-
Strong peristaltic movements mix food with gastric secretions.
-
Forms chyme, a semi-liquid mixture that enhances later intestinal digestion.
-
Breaks down large food particles, increasing surface area.
4. Controlled Gastric Emptying
-
The stomach regulates the delivery of chyme to the duodenum.
-
Slower emptying allows the small intestine adequate time for enzyme action.
-
Gastric emptying is influenced by:
-
Gastrin
-
CCK
-
Enteric nervous system
-
This regulation prevents overwhelming the small intestine with undigested carbohydrates.
5. Minor Continued Activity
-
Before complete acidification, some residual amylase activity may continue briefly in the upper stomach (fundus).
-
But this contribution is very small.
C. Intestinal Phase: Major Digestion
1. Neutralization of Gastric Chyme
When acidic chyme enters the duodenum:
-
Secretin stimulates the pancreas to release bicarbonate-rich pancreatic juice.
-
Neutral pH (6.8–7.4) is restored → optimal for enzyme function.
-
Protects intestinal mucosa from acid damage.
2. Pancreatic Amylase: Luminal Phase Digestion
Enzyme: Pancreatic α-amylase
Stimulated By:
-
CCK (Cholecystokinin) from intestinal cells
-
Vagal stimulation
Action:
Breaks α-1,4-glycosidic bonds in starch and glycogen.
Products Formed:
-
Maltose
-
Maltotriose
-
α-Limit dextrins
(Same end-products as salivary amylase, but in much larger quantity)
Pancreatic amylase is responsible for 70–80% of all carbohydrate digestion.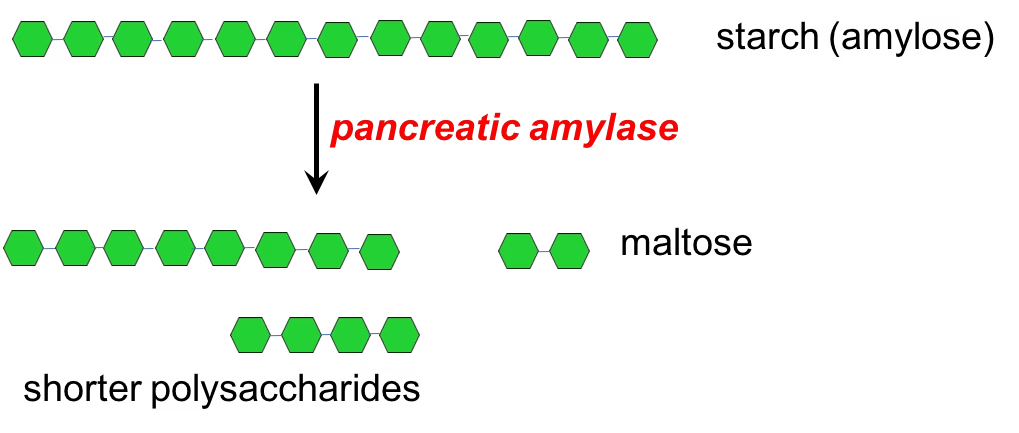
3. Brush-Border Enzymes: Final Hydrolysis
Microvilli of enterocytes contain membrane-bound disaccharidases that complete digestion.
Brush-Border Enzymes
A. Maltase
-
Maltose → Glucose + Glucose
B. Sucrase
-
Sucrose → Glucose + Fructose
C. Lactase
-
Lactose → Glucose + Galactose
-
Most sensitive enzyme; deficiency → lactose intolerance
D. Isomaltase (α-Dextrinase)
-
Breaks α-1,6 bonds in branched dextrins
-
Essential for complete digestion of amylopectin
E. Trehalase
-
Trehalose → Glucose
-
Important for digestion of mushrooms and insects
Importance of Brush-Border Enzymes
-
Without them, disaccharides remain undigested and cause osmotic diarrhea.
-
They determine how efficiently the intestine handles carbohydrate loads.
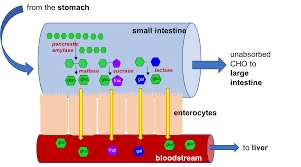
4. Coordination of Digestion and Absorption
As soon as monosaccharides are formed:
-
They are immediately absorbed by enterocyte transporters (SGLT-1, GLUT-5).
-
This prevents carbohydrate accumulation in the lumen.
-
Helps maintain osmotic balance and efficient nutrient uptake.
5. Hormonal and Neural Regulation
-
CCK: stimulates pancreatic amylase secretion.
-
Secretin: releases bicarbonate to optimize pH.
-
Enteric nervous system: regulates motility and mixing.
These mechanisms ensure that digestion is synchronized with gastric emptying.
Absorption of Carbohydrates
1. Site of Absorption
Carbohydrate absorption occurs in:
-
Duodenum and Jejunum – primary sites
-
Ileum – minimal absorption
-
Colon – absorbs only fermentation products like short-chain fatty acids, not carbohydrates
The small intestine contains millions of villi and microvilli, creating a vast surface area that maximizes absorption efficiency.
2. Forms of Carbohydrates Absorbed
Only three monosaccharides are absorbed:
-
Glucose
-
Galactose
-
Fructose
Disaccharides (lactose, maltose, sucrose) and polysaccharides (starch, glycogen) must be digested before absorption.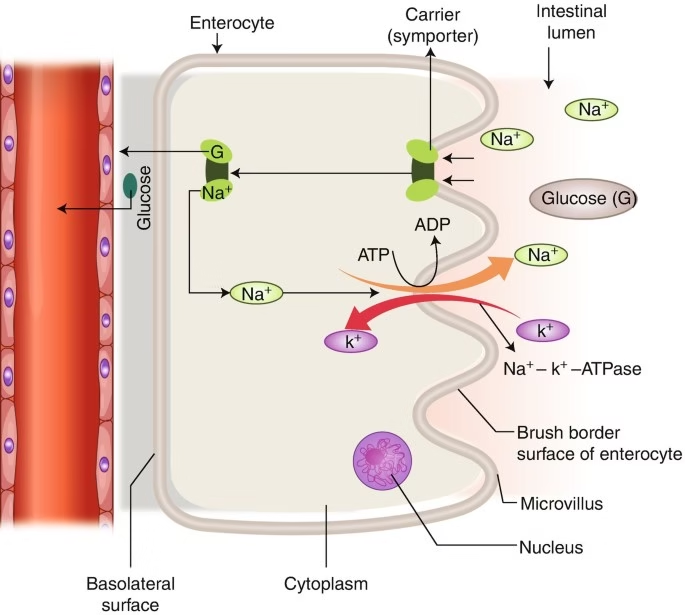
3. Mechanisms of Absorption
Carbohydrate absorption involves three major transporters:
-
SGLT-1 → absorbs glucose and galactose
-
GLUT-5 → absorbs fructose
-
GLUT-2 → transports all monosaccharides into the blood
Each transporter employs a distinct mechanism, ensuring efficient uptake even when concentration gradients fluctuate.
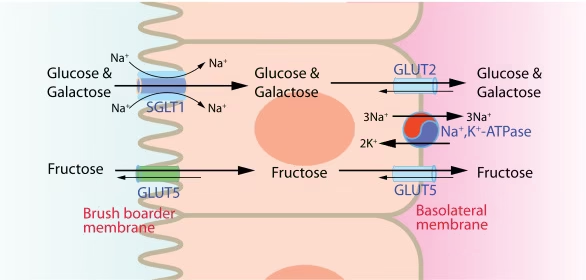
A. Glucose and Galactose Absorption (Active Transport)
Transporter: SGLT-1 (Sodium-Glucose Linked Transporter-1)
Mechanism:
-
Secondary active transport
-
Requires Na⁺ gradient, not direct ATP
-
Na⁺/K⁺ ATPase pump (on basolateral membrane) maintains this gradient
-
Glucose/galactose are co-transported with two sodium ions
Why is this important?
-
Allows absorption even when intestinal glucose concentration is low
-
Explanation for the success of Oral Rehydration Therapy (ORT) — glucose enhances sodium and water absorption
B. Fructose Absorption (Facilitated Diffusion)
Transporter: GLUT-5
Mechanism:
-
Facilitated diffusion, not energy-dependent
-
Works along the concentration gradient
Characteristics:
-
Slower than glucose absorption
-
Overconsumption of fructose can overwhelm GLUT-5 → bloating, diarrhea
C. Transport Into the Bloodstream
After entering the enterocyte:
Transporter: GLUT-2
Function:
-
Moves glucose, galactose, and fructose from the intestinal cell to the portal blood
-
Operates by facilitated diffusion
Pathway:
Enterocyte →
Basolateral membrane →
GLUT-2 →
Portal vein →
Liver →
Metabolic processing
The liver converts fructose and galactose into glucose derivatives for utilization.
Regulation of Carbohydrate Absorption
Carbohydrate absorption is regulated mainly by enzyme activity, transporter function, and intestinal health.
1. Brush-Border Enzyme Levels
- Adequate lactase, sucrase, maltase, and isomaltase are essential.
- Low enzyme activity reduces digestion → poor absorption (e.g., lactose intolerance).
2. Transporter Activity
- SGLT-1 regulates glucose and galactose uptake.
- GLUT-5 regulates fructose uptake.
- GLUT-2 regulates the exit of monosaccharides into the blood.
Their expression increases with high carbohydrate intake.
3. Intestinal Mucosal Health
- Diseases like celiac disease, Crohn’s disease, and infections damage villi → reducing absorption.
4. Hormonal Influence
- Incretins (GLP-1, GIP) and insulin can modulate transporter expression and glucose uptake rate.
5. Luminal Factors
- The presence of sodium enhances glucose absorption (via SGLT-1).
- Adequate pH and proper mixing improve enzyme efficiency.
Clinical Aspects of Carbohydrate Absorption
Clinical issues related to carbohydrate absorption usually arise when digestive enzymes, intestinal transporters, or intestinal mucosa are impaired. These disturbances lead to malabsorption, gastrointestinal symptoms, and metabolic imbalances.
1. Lactose Intolerance (Lactase Deficiency)
The most common clinical disorder of carbohydrate absorption.
Features
- Caused by reduced lactase enzyme activity.
- Unabsorbed lactose draws water into the intestine (osmotic effect).
- Fermentation by colonic bacteria produces gas.
Symptoms
- Bloating
- Flatulence
- Abdominal cramps
- Diarrhea
Biochemical Basis:
-
Reduced lactase enzyme on brush-border → incomplete breakdown of lactose into glucose + galactose
-
Lactose remains unabsorbed (cannot use SGLT-1 or GLUT transporters)
Consequence:
-
Osmotic diarrhea due to unabsorbed lactose
-
Bacterial fermentation → lactic acid, hydrogen gas
-
Symptoms: bloating, cramps, flatulence
2. Fructose Malabsorption
Occurs due to reduced capacity of the GLUT-5 transporter.
Clinical Manifestations
- Bloating
- Diarrhea
- Abdominal pain after consuming high-fructose foods (juices, honey, soft drinks)
Mechanism:
-
Decreased activity or saturation of GLUT-5 transporter
-
Fructose cannot be absorbed by SGLT-1 or GLUT-2 → remains in lumen
Clinical outcome:
-
Bloating, diarrhea, abdominal pain
-
Excessive fructose fermentation by colonic bacteria
3. Sucrase-Isomaltase Deficiency
A rare congenital or acquired defect.
Effects
- Incomplete digestion of sucrose and starch.
- Symptoms resemble those of lactose intolerance but are triggered by foods rich in sucrose.
Biochemical Problem:
-
Deficiency of sucrase–isomaltase complex → impaired hydrolysis of sucrose and α-limit dextrins
Effect:
-
Malabsorption of sucrose and starch breakdown products
-
Leads to osmotic diarrhea and post-meal discomfort
4. Malabsorption Syndromes Affecting Carbohydrates
Damage to the intestinal mucosa reduces enzyme activity and transporter expression.
Common Causes
- Celiac disease
- Tropical sprue
- Crohn’s disease
- Infectious enteritis
- Chemotherapy or radiation-induced injury
Consequences
- Poor absorption of all carbohydrates
- Weight loss
- Nutrient deficiencies
- Chronic diarrhea
Biochemical Impact:
-
Loss of brush-border enzymes
-
Decreased SGLT-1, GLUT-5, and GLUT-2 expression
-
Reduced surface area for absorption
Result:
-
Malabsorption of all carbohydrates
-
Nutrient loss, diarrhea, weight loss
5. Dumping Syndrome
Seen after gastric surgery.
Mechanism
- Rapid entry of hyperosmolar carbohydrates into the small intestine
- Causes massive fluid shifts and hormonal changes
Symptoms
- Nausea
- Dizziness
- Palpitations
- Diarrhea
Mechanism:
-
Rapid delivery of hyperosmolar carbohydrates into small intestine
-
Sudden fluid shifts and exaggerated insulin response
Biochemical Effect:
-
Rapid glucose absorption → high blood glucose → reactive hypoglycemia
6. Diabetes and Carbohydrate Absorption
- Absorption rates are normal, but utilization is impaired due to insulin deficiency/resistance.
- High carbohydrate loads can cause exaggerated post-meal glucose spikes.
7. Oral Rehydration Therapy (ORT)
A major clinical success based on SGLT-1 transporter physiology.
Concept
- Glucose promotes sodium and water absorption → life-saving in diarrhea
- Used globally to prevent dehydration in children and adults
Scientific Basis:
-
SGLT-1 co-transports glucose + sodium, enhancing water absorption
-
Used even when diarrhea impairs other absorption processes
Importance:
-
A life-saving application of carbohydrate transport physiology
8. Small Intestinal Bacterial Overgrowth (SIBO)
Bacteria ferment unabsorbed carbohydrates before they reach the colon.
Effects
- Gas production
- Bloating
- Diarrhea
- Malnutrition in severe cases
MCQs
1. The major site for carbohydrate digestion is:
A. Stomach
B. Oral cavity
C. Small intestine
D. Large intestine
2. Salivary amylase is inactivated in the stomach mainly due to:
A. Pepsin action
B. Low pH (1–2)
C. Bile salts
D. Gastrin
3. The optimum pH for pancreatic amylase is:
A. 2
B. 4
C. 7–8
D. 10
4. Which of the following enzymes hydrolyzes α-1,6 linkages in starch?
A. Pancreatic amylase
B. Sucrase
C. Isomaltase
D. Maltase
5. Lactase enzyme is located in which part of the intestine?
A. Crypts of Lieberkühn
B. Brush border of jejunum
C. Brush border of duodenum
D. Brush border of ileum
6. Glucose absorption in the intestine occurs mainly via:
A. Simple diffusion
B. SGLT-1 transporter
C. GLUT-2
D. Pinocytosis
7. SGLT-1 uses which mechanism?
A. Na⁺-independent facilitated diffusion
B. H⁺-dependent co-transport
C. Na⁺-dependent secondary active transport
D. Passive diffusion
8. Fructose is mainly absorbed by:
A. SGLT-1
B. GLUT-5
C. GLUT-2
D. Na⁺/K⁺ ATPase
9. GLUT-2 is primarily involved in:
A. Brush-border fructose uptake
B. Basolateral transport of monosaccharides
C. H+/glucose co-transport
D. Starch digestion
10. Sucrase-isomaltase deficiency will affect the digestion of:
A. Lactose
B. Starch branch points
C. Sucrose
D. Both B and C
11. Trehalase hydrolyzes trehalose into:
A. Glucose + fructose
B. Glucose + glucose
C. Galactose + glucose
D. Glucose + mannose
12. Which of the following is not a product of pancreatic amylase?
A. Maltose
B. Maltotriose
C. Dextrins
D. Free glucose
13. Lactose intolerance occurs due to deficiency of:
A. Maltase
B. Sucrase
C. β-galactosidase
D. Amylase
14. The earliest enzyme to act on dietary carbohydrates is:
A. Pancreatic amylase
B. Salivary amylase
C. Sucrase
D. Maltase
15. Which enzyme is reduced first in aging?
A. Lactase
B. Sucrase
C. Maltase
D. Isomaltase
16. ORS works due to which transporter?
A. GLUT-2
B. SGLT-1
C. GLUT-4
D. Na⁺/glucose exchanger
17. Carbohydrate absorption occurs mostly in:
A. Duodenum
B. Jejunum
C. Ileum
D. Colon
18. Which of the following steps needs energy (ATP)?
A. SGLT-1 directly
B. Na⁺/K⁺ ATPase
C. GLUT-5
D. Sucrase
19. The major dietary polysaccharide is:
A. Cellulose
B. Pectin
C. Starch
D. Glycosaminoglycans
20. Cellulose is not digested in humans because:
A. Lack of β-1,4-glucosidase
B. Lack of α-amylase
C. Absence of lactase
D. Absence of trehalase
21. Maltose is split by maltase into:
A. Glucose + galactose
B. Glucose + glucose
C. Glucose + fructose
D. Galactose + galactose
22. Pancreatic amylase requires which ion for activity?
A. Na⁺
B. Mg²⁺
C. Ca²⁺
D. Cl⁻
23. Dietary fiber slows glucose absorption mainly by:
A. Inhibiting amylase
B. Increasing gastric emptying time
C. Activating SGLT-1
D. Reducing GLUT-2 expression
24. Glucose and galactose absorption is maximal due to:
A. SGLT-1 saturation
B. High-affinity transport
C. Facilitated diffusion
D. Passive channels
25. Transport of fructose across basolateral membrane uses:
A. SGLT-1
B. GLUT-2
C. GLUT-5
D. Na⁺-dependent transporter
26. A key step that increases pancreatic amylase secretion is:
A. Secretin release
B. Cholecystokinin release
C. Gastrin release
D. Somatostatin release
27. Glucose uptake into enterocytes leads to water absorption due to:
A. Osmosis following Na⁺
B. High intracellular glucose
C. GLUT-2 activation
D. Low luminal pH
28. The brush border enzyme complex for starch digestion is:
A. Sucrase-isomaltase
B. Maltase-glucoamylase
C. Lactase
D. Both A and B
29. Acarbose inhibits:
A. Salivary amylase
B. Pancreatic lipase
C. Brush border α-glucosidases
D. GLUT-2
30. Incomplete digestion of carbohydrates leads to:
A. Increased bile secretion
B. Osmotic diarrhea
C. Constipation
D. Hypernatremia
31. Which disaccharide has an α-1,2 linkage?
A. Lactose
B. Sucrose
C. Maltose
D. Trehalose
32. Rate-limiting factor in carbohydrate digestion is:
A. Amylase activity
B. Brush border enzyme activity
C. Gastric emptying
D. SGLT-1 expression
33. Monosaccharides enter portal circulation via:
A. Mesenteric lymphatics
B. Hepatic artery
C. Hepatic portal vein
D. Thoracic duct
34. Which transporter is insulin-independent?
A. GLUT-4
B. GLUT-2
C. SGLT-1
D. Both B and C
35. High sucrose intake increases activity of:
A. Lactase
B. Sucrase
C. Maltase
D. Pancreatic amylase
36. Which is not a brush-border enzyme?
A. Lactase
B. Sucrase
C. Pancreatic amylase
D. Maltase
37. Raffinose is digested by:
A. Human α-galactosidase
B. Pancreatic amylase
C. Brush border enzymes
D. Not digested in humans
38. Which is a clinical feature of lactase deficiency?
A. Hyperglycemia
B. Bloating and flatulence
C. Constipation
D. Hypothermia
39. The first step in carbohydrate digestion after the stomach is:
A. Pancreatic amylase action
B. Sucrase activity
C. Enterokinase secretion
D. HCl neutralization
40. Glucoamylase primarily releases:
A. Glucose
B. Maltose
C. Fructose
D. Galactose
41. Which transporter is upregulated after a high-carbohydrate meal?
A. GLUT-5
B. GLUT-2
C. SGLT-1
D. Na⁺/K⁺ ATPase
42. The transport of glucose across basolateral membrane is:
A. Primary active
B. Secondary active
C. Facilitated diffusion
D. Passive diffusion
43. Enzyme responsible for limit dextrin hydrolysis:
A. Amylase
B. Sucrase
C. Isomaltase
D. Galactosidase
44. Main cause of carbohydrate malabsorption in rotavirus infection:
A. Loss of brush border enzymes
B. Low pancreatic enzyme
C. Low salivary amylase
D. High gastric pH
45. Sucrase breaks sucrose into:
A. Glucose + glucose
B. Glucose + galactose
C. Glucose + fructose
D. Fructose + galactose
46. High-fiber diet affects glucose absorption by:
A. Reducing amylase secretion
B. Delaying gastric emptying
C. Inhibiting lactase
D. Destroying GLUT-2
47. After a large carbohydrate meal, which transporter is rapidly inserted into the apical membrane?
A. GLUT-5
B. GLUT-2
C. SGLT-1
D. GLUT-4
48. Resistance starch is digested in:
A. Mouth
B. Stomach
C. Colon
D. Ileum
49. The major stimulus for pancreatic amylase secretion is:
A. Secretin
B. CCK
C. Gastrin
D. Ghrelin
50. The only carbohydrate absorbed in the colon is:
A. Glucose
B. Fructose
C. Short-chain fatty acids
D. Galactose
Answers
-
C
-
B
-
C
-
C
-
B
-
B
-
C
-
B
-
B
-
D
-
B
-
D
-
C
-
B
-
A
-
B
-
B
-
B
-
C
-
A
-
B
-
C
-
B
-
B
-
B
-
B
-
A
-
D
-
C
-
B
-
B
-
B
-
C
-
D
-
B
-
C
-
D
-
B
-
A
-
A
-
B
-
C
-
C
-
A
-
C
-
B
-
B
-
C
-
B
-
C