
Introduction
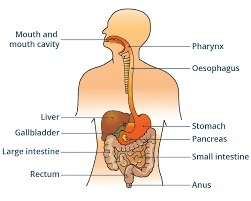
- The digestive system consists of the oral cavity and a hollow tubular gastrointestinal tract (GIT) plus digestive glands associated
with it. - The main function of the digestive system is to digest the ingested food and absorb the nutrients.
Oral Cavity
General Features
-
The oral cavity is the first part of the digestive system.
-
Food is broken into small pieces by teeth.
-
Saliva moistens and lubricates food.
-
Saliva is secreted by three pairs of major and minor salivary glands.
-
Amylase in saliva initiates carbohydrate digestion.
-
Saliva has bactericidal action.
-
The oral cavity has two parts: the vestibule and the oral cavity proper.
-
Vestibule: a slit-like space between the lips/cheeks externally and the gums/teeth internally.
-
Oral cavity proper: a large space bounded by dental arches (front/side) and palate (above), containing the tongue from the floor.
-
Lined by moist oral mucosa, continuous with dry skin at lip junction.
Structure of Oral Mucosa
-
Oral mucosa is made of stratified squamous epithelium and underlying connective tissue (lamina propria).
-
No muscularis mucosa is present.
-
Deeper part of lamina propria with blood vessels, adipose, and glands is called submucosa.
-
Submucosa contains minor salivary glands:
-
Labial (lip)
-
Buccal (cheek)
-
Palatine (palate)
-
Lingual (tongue)
-
-
Sebaceous glands may be present, seen as pale yellow Fordyce’s spots.
-
The presence of sebaceous glands is due to retained skin ectoderm during oral ectoderm invagination.
-
Oral mucosa varies structurally in different regions.
-
Types of oral mucosa (based on function):
-
Masticatory mucosa
-
Lining mucosa
-
Specialized mucosa
-
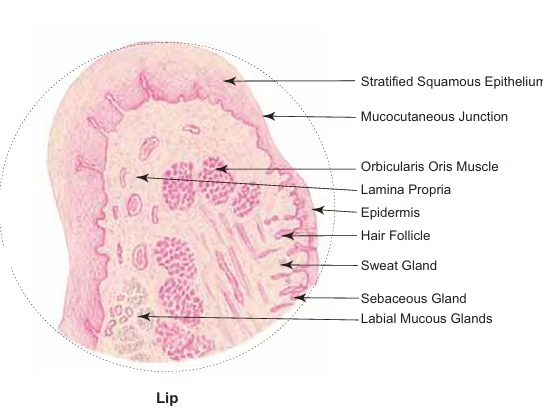
Lips
-
Lips are fleshy mucocutaneous flaps forming boundaries of the oral fissure.
-
Externally covered by dry hairy skin, internally by wet mucous membrane.
-
Middle part contains orbicularis oris (skeletal muscle, circularly arranged).
-
Oral orifice is a mucocutaneous junction where skin continues with mucous membrane.
-
Transition from keratinized skin epithelium to nonkeratinized labial mucosa = vermillion border (red line).
-
Labial epithelium is thick with deep vascular papillae of lamina propria.
-
Submucosa contains large labial glands (mainly mucous).
Gingiva
-
Gingiva (gum) = masticatory oral mucosa around the neck of the tooth.
-
Paler in color than alveolar mucosa.
-
Two parts:
-
Free gingiva – cuff around tooth neck.
-
Attached gingiva – firmly attached to alveolar bone.
-
-
Gingival sulcus/crevice = potential space between free gingiva and enamel.
-
Depth: 0.5–3.0 mm (average 1.8 mm).
-
Floor usually attached to enamel; with age may shift to CEJ or cementum.
-
-
Oral surface: lined by thick stratified squamous oral gingival epithelium.
-
At free margin (gingival crest), it continues with sulcular epithelium.
-
Sulcular epithelium = thin, lacks epithelial ridges, smooth interface with lamina propria.
Teeth
-
Teeth help in the mastication (chewing) of food.
-
Anchored in the sockets of the alveolar processes of the maxilla and mandible.
-
Alveolar processes are covered by the gingiva (gums), firmly attached to the periosteum.
-
Two sets of teeth in humans:
-
Deciduous (milk) teeth – 10 in each jaw, later replaced.
-
Permanent teeth – 16 in each jaw.
-
-
Both sets have similar histological structure.
Histological structure of a tooth
Parts of a typical tooth:
-
Crown – visible part above the gum.
-
Root – concealed part, anchored to socket by periodontal ligament; tip has apical foramen.
-
Neck – constricted junction between crown and root near gum line.
-
Pulp cavity & root canal – interior, filled with dentinal pulp.
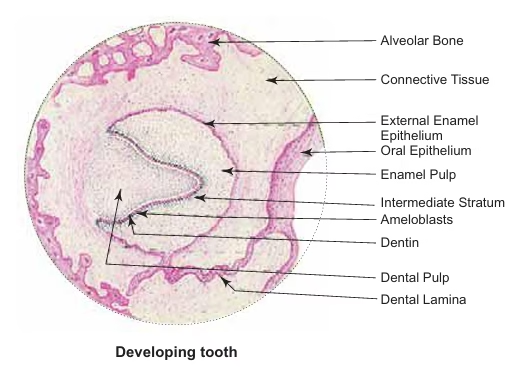
Tooth tissues:
-
Hard tissues – dentine, enamel, cementum.
-
Soft tissues – dentinal pulp, periodontal ligament.
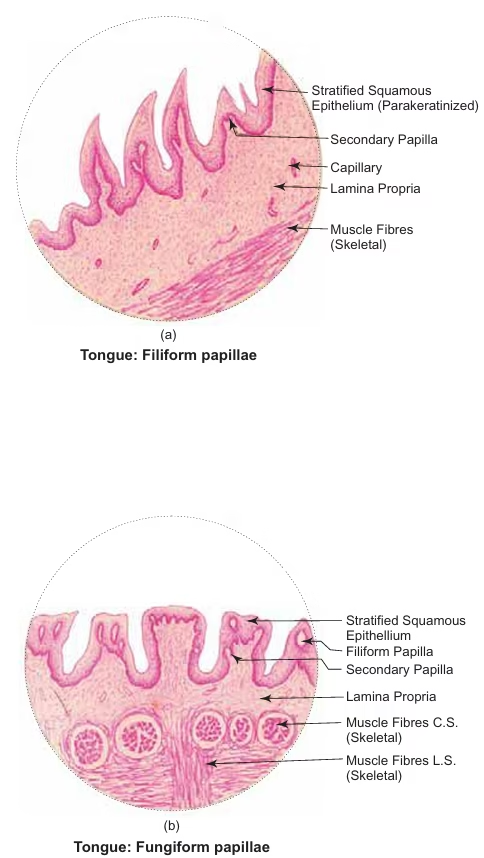
Tongue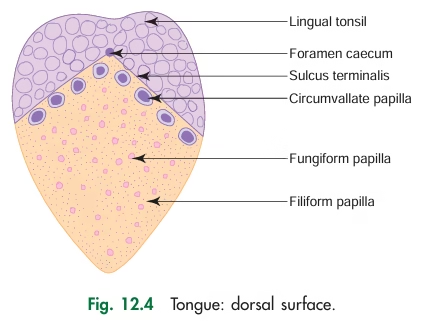
-
Tongue = muscular organ made of intrinsic & extrinsic skeletal muscles, covered by mucous membrane.
-
Mucous membrane: stratified squamous epithelium (keratinized at filiform tips) + lamina propria.
-
Lingual glands:
-
Anterior lingual glands – mixed (seromucous), at tip.
-
von Ebner’s glands – serous, near vallate & foliate papillae.
-
Posterior lingual glands – mucous, near lingual tonsil (ducts open into crypts).
-
-
Dorsal surface: rough (papillae & tonsils).
-
Ventral surface: smooth & slippery.
-
Dorsal surface divided by sulcus terminalis (V-shaped):
-
Anterior 2/3 = oral part (with papillae).
-
Posterior 1/3 = pharyngeal part (with lingual tonsils).
-
-
Lingual papillae (4 types):
-
Filiform
-
Fungiform
-
Circumvallate
-
Foliate (rudimentary in humans)
-
Taste Buds
-
Present in epithelium of fungiform, circumvallate & foliate papillae; also in epiglottis, soft palate, and oropharynx.
-
Appear as oval, pale-staining bodies in stratified squamous epithelium, extending from the basement membrane to the surface.
-
Made of elongated spindle-shaped cells arranged perpendicular to the epithelium.
-
Apical ends converge at the taste pore; microvilli (taste hairs) project through it.
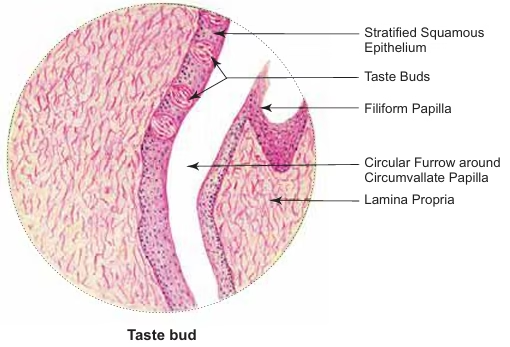
Cell types in taste buds:
-
Taste (gustatory) cells – Type II
-
Lightly stained, elongated, with apical microvilli.
-
Associated with unmyelinated nerve fibers.
-
-
Sustentacular (supporting) cells – Type I
-
Darkly stained, elongated, with apical microvilli.
-
Also linked with unmyelinated nerve fibers.
-
Support taste cells & secrete dense amorphous material.
-
-
Basal (stem) cells
-
Small, pyramidal, near the basement membrane.
-
Do not reach the taste pore.
-
Give rise to taste & supporting cells.
-
Gastrointestinal Tract
Oesophagus
General Features:
-
Oesophagus = long (25 cm) muscular tube from pharynx to stomach.
-
Conducts chewed food (bolus) and liquids to stomach.
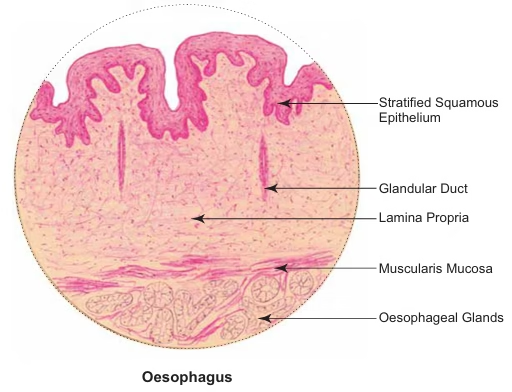
Oesophagus Structure:
-
Mucosa
-
Epithelium: stratified squamous nonkeratinized.
-
Lamina propria: contains oesophageal cardiac glands (lower part).
-
Muscularis mucosa: single longitudinal smooth muscle layer (no circular layer).
-
-
Submucosa
-
Contains mucous oesophageal glands.
-
-
Muscularis externa (inner circular, outer longitudinal)
-
Upper 1/3: skeletal muscle only.
-
Middle 1/3: both skeletal & smooth muscle.
-
Lower 1/3: smooth muscle only.
-
-
Adventitia
-
Typical connective tissue coat, as in the general GIT.
-
Stomach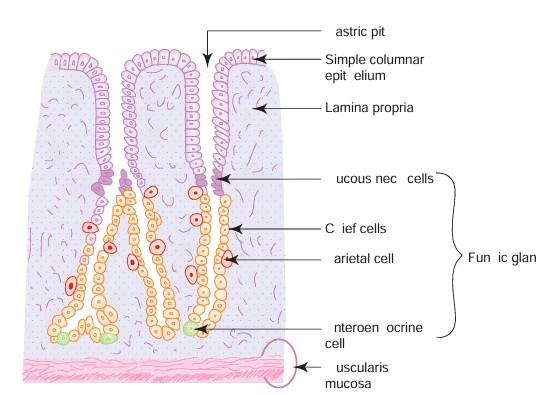
General Features
-
Muscular bag receiving food from oesophagus.
-
Converts food into chyme; absorbs water, salts, alcohol, drugs.
-
Longitudinal folds called rugae, disappear when stomach expands.
-
Invaginations in mucosa = gastric pits (foveolae gastricae); all glands open at pit base.
-
Anatomical parts: cardia, fundus, body, pylorus (histologically: cardia, fundus/body, pylorus).
Stomach Structure
-
Mucosa
-
Epithelium: simple tall columnar, secretes mucus, renewed every 3 days.
-
Lamina propria: contains gastric glands (cardiac, fundic, pyloric).
-
Muscularis mucosa: two smooth muscle layers; fibers extend between glands.
-
-
Submucosa – as in general GIT.
-
Muscularis externa – three layers of smooth muscle: inner oblique, middle circular, outer longitudinal.
-
Serosa – as in general GIT.
Salient Features by Region
1. Cardia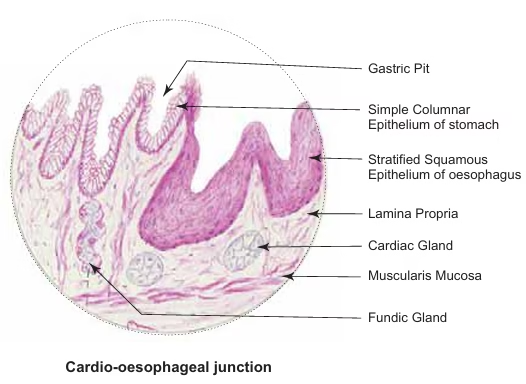
-
Transition from oesophageal stratified squamous → gastric columnar epithelium.
-
Cardiac glands (mucous) in lamina propria.
-
Shallow gastric pits.
2. Fundus & Body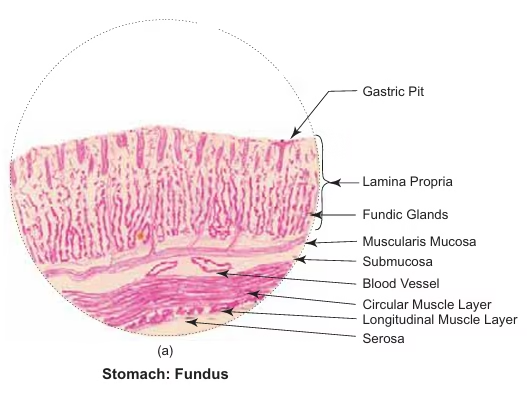
-
Shallow gastric pits = 1/4 of mucosa thickness.
-
Fundic glands: simple branched tubular; lamina propria.
-
Mucous neck cells – low columnar, acid mucus, neck region.
-
Parietal (oxyntic) cells – large pyramidal, acidophilic, secrete HCl & intrinsic factor.
-
Chief (zymogenic) cells – small cuboidal, basophilic, secrete pepsinogen, lipase, amylase.
-
Enteroendocrine cells – basal, unicellular, secrete amines & enteroglucagon (APUD series).
-
3. Pylorus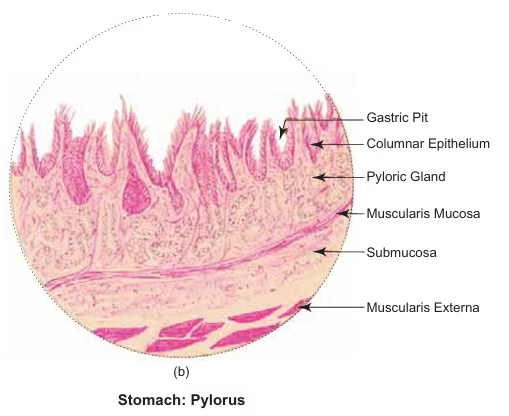
-
Deep gastric pits = 1/2 mucosa thickness.
-
Pyloric glands (mucous) in the lamina propria.
-
The middle circular muscle thickens → pyloric sphincter.
Small intestine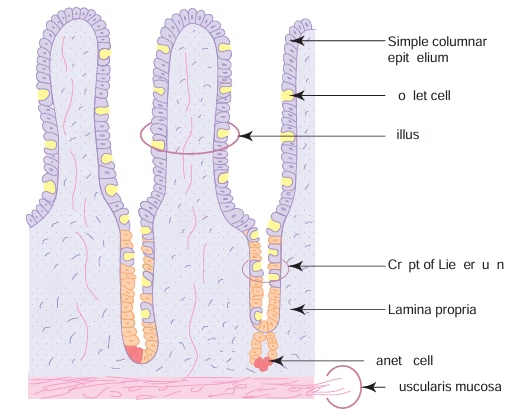
General Features
-
Length ≈ 6 m; divided into duodenum, jejunum, ileum.
-
Principal site for digestion completion and absorption; secretes hormones via enteroendocrine cells.
-
Luminal surface area increased 400–600× by:
-
Plicae circulares (valves of Kerckring) – permanent folds of mucosa & submucosa; 2–3× increase.
-
Intestinal villi – finger-like mucosal projections with lamina propria, lacteal, capillaries; 10× increase.
-
Microvilli – on absorptive epithelium, striated border; 20× increase.
-
-
Nutrient absorption:
-
Proteins → amino acids → capillaries → portal vein → liver.
-
Carbohydrates → monosaccharides → capillaries → portal vein → liver.
-
Lipids → free fatty acids & monoglycerides → lacteal → thoracic duct → systemic circulation.
-
Monoglycerides → triglycerides → coated with protein/phospholipids → chylomicrons → lymphatics.
-
Structure
-
Mucosa
-
Epithelium: simple columnar absorptive with goblet cells; finger-like villi; glycocalyx protects & adsorbs enzymes.
-
Crypts of Lieberkuhn: tubular invaginations; lined by columnar & goblet cells; Paneth cells at base secrete lysozyme.
-
Epithelium renewed every 3–5 days.
-
Lamina propria: fibroblasts, mast cells, plasma cells, lymphocytes, lacteals, capillary loops, crypts.
-
Muscularis mucosa: as general GIT plan.
-
-
Submucosa
-
Duodenum: Brunner’s glands (branched, coiled, mucous; neutralize acid).
-
Ileum: Peyer’s patches (aggregated lymphoid follicles, M cells).
-
Jejunum: no glands or Peyer’s patches.
-
-
Muscularis externa: as general GIT plan.
-
Serosa: as general GIT plan.
Region-specific Features
-
Duodenum:
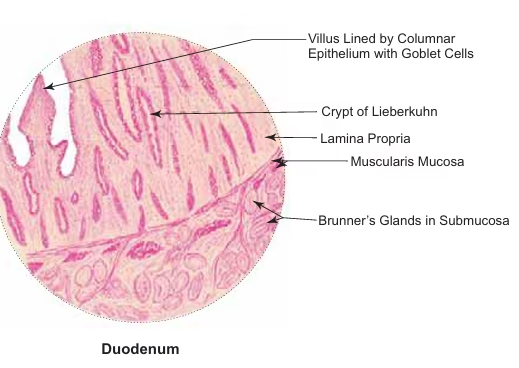
-
Leaf-like villi.
-
Muscularis mucosa disrupted.
-
Brunner’s glands in submucosa.
-
Enteroendocrine cells secrete urogastrone, secretin, cholecystokinin.
-
-
Jejunum:
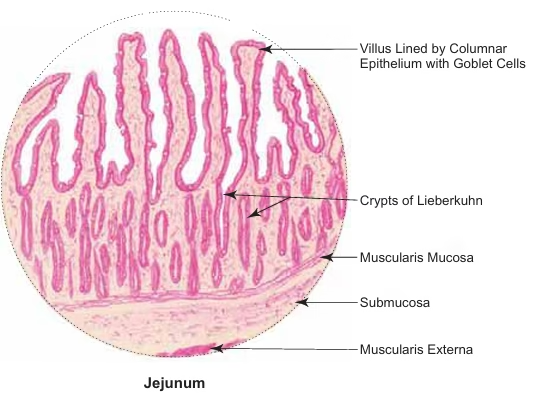
-
Finger-like villi.
-
Submucosa lacks glands & Peyer’s patches.
-
-
Ileum:
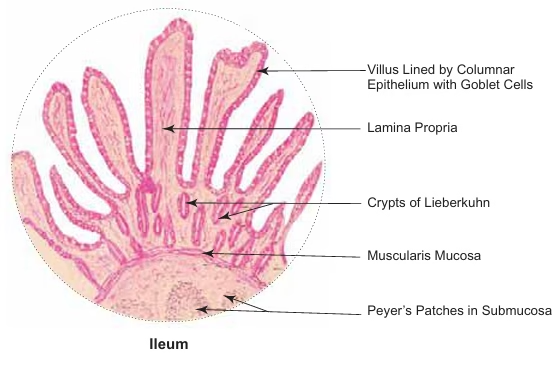
-
Thin, slender villi.
-
Submucosa contains Peyer’s patches.
-
M cells over lymphoid follicles are present.
-
Large Intestine
General Features
-
Composed of caecum, appendix, colon, rectum, anal canal.
-
Short, leaf-like villi present in duodenum; large intestine lacks villi.
-
Harbours nonpathogenic bacteria producing:
-
Vitamin B12 – necessary for haemopoiesis.
-
Vitamin K – necessary for coagulation.
-
-
Functions: absorption of electrolytes & water, mucus secretion for fecal passage.
Structure
-
Follows general small intestine plan, with specific modifications in each region.
Region-specific Features
1. Vermiform Appendix 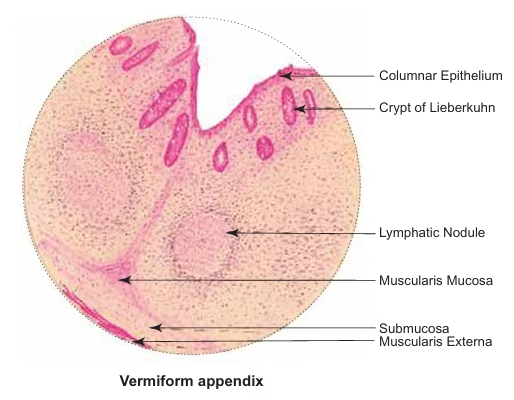
-
Small, angular lumen with thick wall.
-
No villi; few short crypts.
-
Ring of lymphoid follicles with germinal centers around lumen.
-
Muscularis mucosa disrupted.
2. Caecum & Colon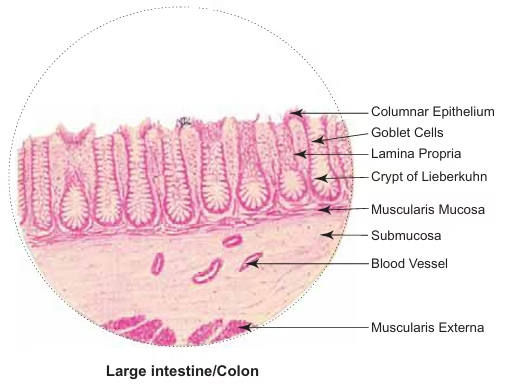
-
No villi.
-
Well-developed crypts lined with goblet cells; Paneth cells absent.
-
Outer longitudinal layer of muscularis externa forms 3 taenia coli.
-
Serosa shows fat-filled pockets (appendices epiploicae).
3. Rectum
-
Long crypts of Lieberkuhn.
-
Less lymphoid tissue in lamina propria.
-
Muscle coat lacks taenia coli.
-
Serosa replaced by adventitia in lower part.
4. Anal Canal
-
Epithelium changes:
-
Above anal valves – stratified cuboidal.
-
At anal valves – stratified squamous.
-
At anal orifice – epidermis (mucocutaneous junction).
-
-
No crypts of Lieberkuhn; muscularis mucosa absent.
-
Lamina propria becomes submucosa with rich vascular plexus.
-
Inner circular muscle → internal anal sphincter (smooth).
-
External skeletal muscle → external anal sphincter.
Liver
General Features
-
Second heaviest organ (~2% body weight), mainly in right hypochondrium, below diaphragm.
-
Blood supply: portal vein 70%, hepatic artery 30%.
-
Functions:
-
Exocrine: bile synthesis & secretion for fat emulsification; bilirubin excretion.
-
Endocrine: plasma proteins (albumin, prothrombin, fibrinogen) synthesis.
-
Glycogen storage, drug detoxification, fetal hematopoiesis.
-
Phagocytosis of cellular debris by Kupffer cells.
-
Structure
-
Enveloped by Glisson’s capsule (fibrous), sending trabeculae into parenchyma.
-
Trabeculae contain portal tract/space/canal: hepatic artery, portal vein, hepatic duct, lymphatics.
-
Liver lobule (classical): hexagonal; central vein at center; portal triads at corners.
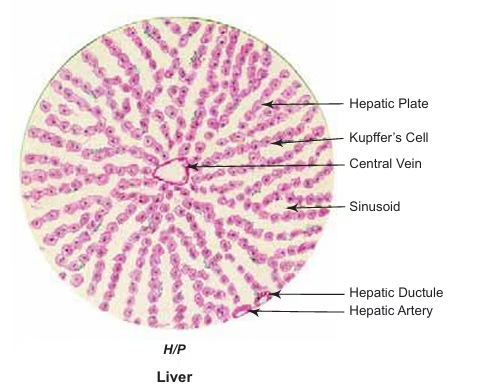
-
Hepatocytes:
-
Polyhedral, 1–2 nuclei (polyploidy common), eosinophilic cytoplasm, abundant organelles.
-
Arranged in plates radiating from central vein, 1-cell thick in adults, 2-cell thick in children <7 yrs.
-
Surfaces:
-
Sinusoidal surface → blood exchange via space of Disse.
-
Lateral surface → forms bile canaliculi between hepatocytes.
-
-
Bile canaliculi → canal of Hering → hepatic ductules → hepatic duct (bile flows from center → periphery).
-
-
Liver sinusoids:
-
Lined by fenestrated endothelial cells.
-
Kupffer cells: phagocytose worn-out RBCs.
-
-
Hepatic stellate (Ito) cells: store vitamin A; activated in pathology.
Pancreas
General Features
-
Pancreas: both exocrine digestive and endocrine gland.
-
Extends from duodenum (right) to spleen (left), retroperitoneally in posterior abdominal wall.
Structure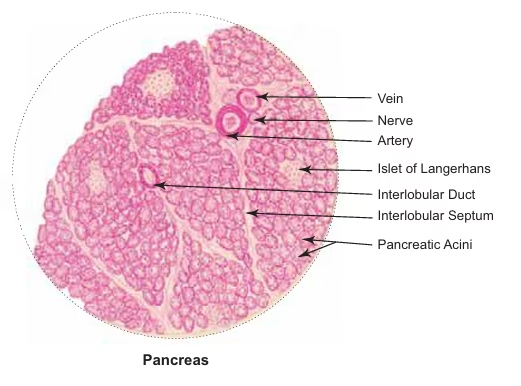
-
Made of serous acini arranged into lobules.
-
Lobules separated by interlobular septa carrying blood vessels, nerves, and ducts.
-
Serous acinus:
-
Pyramidal cells surrounding a small lumen.
-
Basal region: darkly stained; apical region: lightly stained with zymogen granules.
-
No myoepithelial cells.
-
Pancreatic stellate cells (myofibroblast-like) encircle acinus base in periacinar connective tissue.
-
-
Some acini contain centroacinar cells:
-
Pale-staining, cuboidal cells within lumen.
-
Represent intra-acinar part of intercalated duct (starts inside acinus).
-
Gall Bladder
General Features
-
A muscular sac on the visceral surface of the liver in the gall bladder fossa.
-
Functions:
-
Concentrates bile by absorbing water.
-
Stores bile (~50–100 ml capacity).
-
-
Regulation:
-
Fat in the small intestine → stimulates cholecystokinin (CCK) from duodenal enteroendocrine cells → gall bladder contracts → bile is released into the common bile duct.
-
-
Bile salts: emulsify lipids, aiding absorption.
Structure 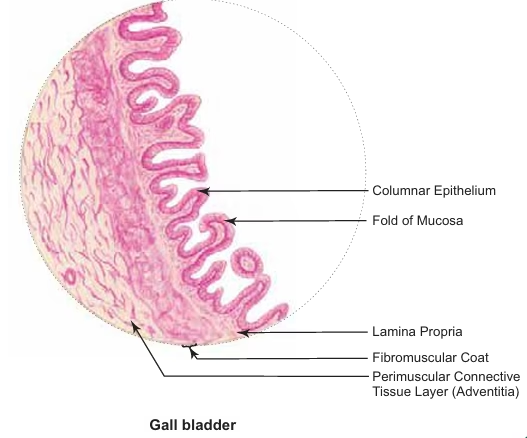
-
Mucosa
-
Simple columnar epithelium with microvilli (brush border) for water absorption.
-
Lamina propria rich in elastic fibers and blood vessels.
-
Folded when bladder is empty.
-
Muscularis mucosa & submucosa absent (fused with muscularis externa).
-
-
Fibromuscular Layer
-
Circular smooth muscle fibers interspersed with connective tissue.
-
-
Serosa/Adventitia
-
Serosa: fundus & lower body surface (covered by peritoneum).
-
Adventitia: upper surface attached to liver fossa.
-