
Proteinuria 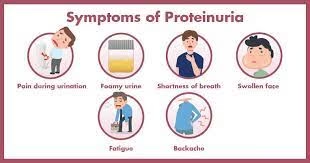
Introduction
Proteinuria is the abnormal presence of protein in the urine, often exceeding 150 mg/day in adults. It can be transient, orthostatic (position-dependent), or persistent. Persistent proteinuria usually indicates kidney damage or systemic disease. It is classified based on severity:
- Normal: <150 mg/day
- Microalbuminuria: 30–300 mg/day (an early sign of kidney dysfunction)
- Macroalbuminuria: >300 mg/day
- Nephrotic-range proteinuria: >3.5 g/day
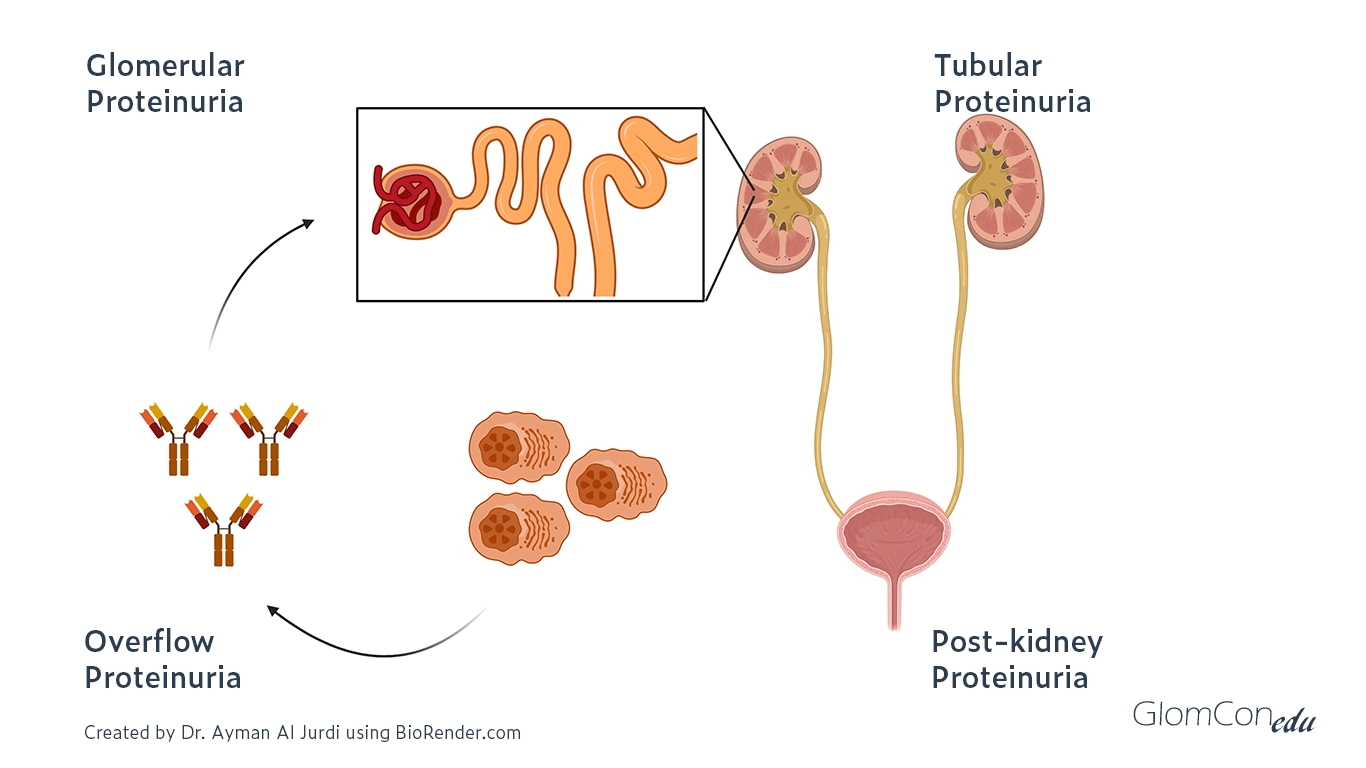
Pathophysiology
Proteinuria results from disruption in the kidneys’ normal filtration or reabsorption processes. Key mechanisms include:
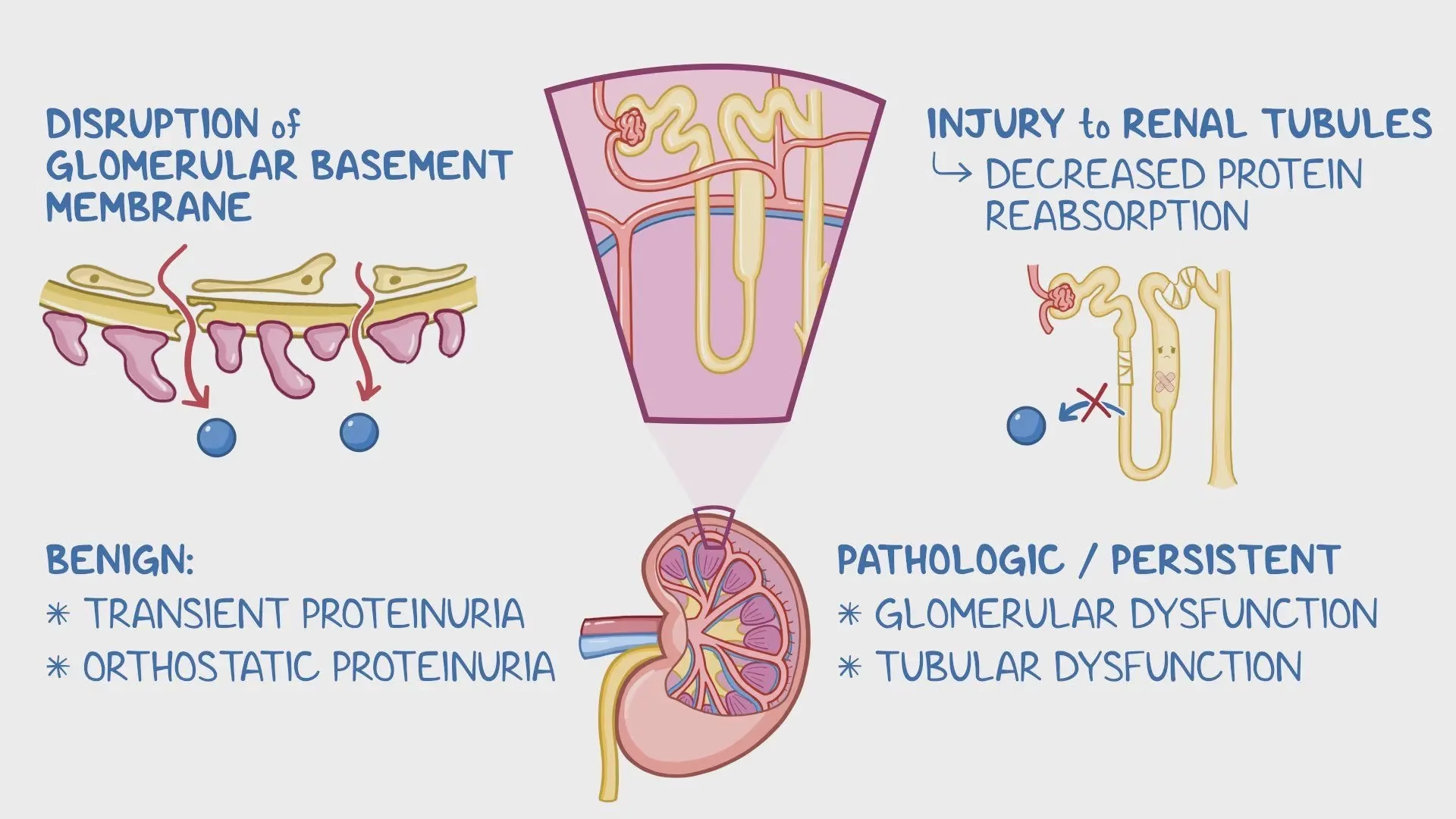
- Glomerular Proteinuria:
The glomerular filtration barrier (endothelium, basement membrane, or podocytes) is damaged. Causes increased permeability to large proteins, especially albumin. Common in glomerulonephritis or diabetic nephropathy.
- Tubular Proteinuria:
Dysfunction of the proximal tubules reduces protein reabsorption. Associated with tubulointerstitial nephritis, pyelonephritis, or toxic injury (e.g., drugs, heavy metals).
- Proteinuria:
Excess production of low molecular weight proteins (e.g., immunoglobulin light chains). Seen in multiple myeloma or hemolysis.
- Post-renal Proteinuria:
Protein leakage into urine due to urinary tract inflammation, infection, or malignancy.
Clinical Features
- General Symptoms:
-
- Foamy urine: Excess protein alters surface tension.
- Edema: Common in nephrotic syndrome due to hypoalbuminemia.
- Fatigue: From reduced kidney function.
- Disease-Specific Features:
-
- Diabetic nephropathy: Proteinuria, hypertension, and retinopathy.
- Nephrotic syndrome: Severe proteinuria (>3.5 g/day), hypoalbuminemia, hyperlipidemia, and edema.
- Lupus nephritis: Proteinuria with systemic symptoms (e.g., joint pain, rash).
- Multiple myeloma: Proteinuria with bone pain, anemia, and hypercalcemia.
Biochemical Manifestations
- Urine Findings:
-
- Dipstick test: Detects albumin (semi-quantitative).
- 24-hour urine collection: Quantifies total protein excretion.
- Spot urine protein-to-creatinine ratio (UPCR): Correlates with 24-hour excretion.
- Urine microscopy: Identifies casts or dysmorphic red blood cells (indicative of glomerular damage).
- Serum Findings:
-
- Hypoalbuminemia: Protein loss in urine.
- Hyperlipidemia: Seen in nephrotic syndrome due to compensatory liver synthesis.
- Elevated creatinine/BUN: Indicates impaired renal function.
- Specific markers: Monoclonal proteins in multiple myeloma (via serum protein electrophoresis).
Diagnosis
- Initial Evaluation:
-
- History and physical examination to identify possible causes (e.g., diabetes, infections).
- Urinalysis (dipstick test) for initial protein detection.
- Quantification of Proteinuria:
-
- 24-hour urine protein collection: Gold standard for quantifying protein.
- Spot urine UPCR: An easier alternative to estimate daily protein excretion.
- Additional Tests:
-
- Urine protein electrophoresis (UPEP): Detects monoclonal or abnormal proteins.
- Serum studies: Creatinine, albumin, lipids, and markers of systemic disease.
- Renal imaging: Ultrasound to assess kidney size and structure.
- Renal biopsy: Indicated in unexplained, severe, or persistent proteinuria, especially if associated with hematuria, declining kidney function, or systemic symptoms.
Treatment
- General Management:
-
- Lifestyle:
- Sodium restriction to reduce edema.
- Protein intake moderation to prevent renal stress (not universally recommended).
- Blood pressure control: Target <130/80 mmHg, often with ACE inhibitors or ARBs.
- Lifestyle:
- Medications:
-
- ACE inhibitors/ARBs: Reduce intraglomerular pressure and protein leakage.
- Statins: Manage hyperlipidemia in nephrotic syndrome.
- Diuretics: Control edema.
- Immunosuppressive agents:
- Used in autoimmune conditions like lupus nephritis or minimal change disease.
- Examples: Corticosteroids, cyclophosphamide, or mycophenolate mofetil.
- Anticoagulation: For patients with nephrotic syndrome and thrombosis risk.
- Disease-Specific Treatments:
-
- Diabetic nephropathy: Optimize glycemic control with SGLT2 inhibitors or GLP-1 receptor agonists.
- Lupus nephritis: Immunosuppressive therapy (e.g., corticosteroids, hydroxychloroquine).
- Multiple myeloma: Chemotherapy or autologous stem cell transplantation.
- Supportive Care:
-
- Manage complications like infection, anemia, or malnutrition.
- Monitor kidney function regularly to detect chronic kidney disease (CKD) progression.
- Introduction
Hypoproteinemia
Pathophysiology
- Decreased Protein Synthesis:
-
- Seen in liver diseases (e.g., cirrhosis) where albumin production is impaired.
- Increased Protein Loss:
-
- Protein loss through the kidneys (nephrotic syndrome) or gastrointestinal tract (protein-losing enteropathy).
- Inadequate Protein Intake:
-
- Malnutrition or malabsorption syndromes (e.g., celiac disease).
- Dilutional Causes:
-
- Overhydration or fluid overload.
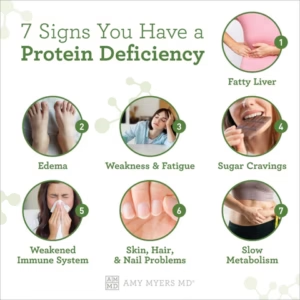
Clinical Features
-
- Generalized Edema: Due to reduced oncotic pressure (common with hypoalbuminemia).
- Muscle wasting: Caused by protein depletion.
- Fatigue and weakness.
- Infections: Due to immune dysfunction (low immunoglobulins).
- Delayed wound healing.
Biochemical Manifestations
-
- Serum total protein: <6 g/dL.
- Serum albumin: Often <3.5 g/dL.
- Urinary protein: Elevated in protein-losing conditions (e.g., nephrotic syndrome).
- Electrophoresis findings: May show low albumin or specific globulin patterns based on the underlying cause.
Diagnosis
- Blood tests:
-
- Serum total protein and albumin levels.
- Serum protein electrophoresis (to assess globulin patterns).
- Urine tests: Detect protein loss (e.g., 24-hour urine protein).
- Liver function tests: Assess protein synthesis capacity.
- Imaging/Endoscopy: To evaluate malabsorption or protein-losing enteropathies.
Treatment
- Treat the underlying cause:
- Malnutrition: Improve dietary intake.
- Liver disease: Manage underlying liver dysfunction.
- Nephrotic syndrome: Use diuretics, ACE inhibitors, or immunosuppressants.
- Protein supplementation: In severe protein depletion.
- Diuretics: For edema, used cautiously.
Hyperproteinemia
Pathophysiology
- Relative Causes:
-
- Dehydration or hemoconcentration due to fluid loss (e.g., diarrhea, vomiting).
- Excessive Protein Production:
-
- Increased synthesis of immunoglobulins (e.g., multiple myeloma, Waldenström macroglobulinemia).
- Chronic inflammation or infections (e.g., tuberculosis, rheumatoid arthritis).
- Monoclonal Gammopathies:
-
- Conditions like monoclonal gammopathy of undetermined significance (MGUS).
Clinical Features
- Asymptomatic: Often detected on routine blood work.
- Symptoms of the underlying disease:
- Bone pain or fractures in multiple myeloma.
- Fatigue and weight loss in chronic inflammatory states.
- Hyperviscosity syndrome: Rare but may occur in Waldenström macroglobulinemia, causing blurred vision, dizziness, and headaches.
Biochemical Manifestations
- Serum total protein: >8.3 g/dL.
- Electrophoresis: Detects monoclonal protein bands (M-proteins).
- Serum albumin: Often normal unless dehydration is present.
- Elevated immunoglobulins: Seen in conditions like multiple myeloma.
Diagnosis
- Blood tests:
-
- Serum total protein and albumin levels.
- Serum protein electrophoresis and immunofixation for monoclonal proteins.
- Bone marrow biopsy: If multiple myeloma or other plasma cell disorders are suspected.
- Imaging: To detect lytic bone lesions in multiple myeloma.
Treatment
- Rehydrate: Correct dehydration if relative hyperproteinemia is present.
- Treat underlying conditions:
- Multiple myeloma: Chemotherapy, autologous stem cell transplant, or targeted therapy.
- Chronic inflammation: Manage the primary disease (e.g., infections or autoimmune conditions).
- Plasmapheresis: For hyperviscosity syndrome in severe cases.
Hypergammaglobulinemia
Introduction
- Hypergammaglobulinemia is an abnormal increase in gamma globulins (immunoglobulins) in the blood, primarily produced by plasma cells as part of the immune response.
- It can result from chronic immune stimulation, infections, autoimmune disorders, or monoclonal plasma cell proliferations such as multiple myeloma.
Pathophysiology
The mechanisms leading to hypergammaglobulinemia depend on whether the condition is polyclonal or monoclonal:
- Polyclonal Hypergammaglobulinemia
- Mechanism:
- Chronic immune activation stimulates multiple clones of plasma cells, leading to increased production of various immunoglobulins.
- Commonly seen in infections, autoimmune diseases, and chronic inflammatory states.
- Causes:
- Infectious diseases:
- Viral: HIV, hepatitis B/C, Epstein-Barr virus (EBV).
- Bacterial: Tuberculosis, syphilis, chronic abscesses.
- Parasitic: Schistosomiasis, malaria.
- Autoimmune diseases:
- Rheumatoid arthritis (RA).
- Systemic lupus erythematosus (SLE).
- Chronic liver diseases:
- Cirrhosis (especially due to alcohol or hepatitis).
- Other conditions: Sarcoidosis, primary immunodeficiencies.
- Monoclonal Hypergammaglobulinemia
- Mechanism:
- A single plasma cell clone proliferates abnormally, producing large amounts of a single type of immunoglobulin (monoclonal protein or M-protein).
- Seen in plasma cell dyscrasias.
- Causes:
- Multiple myeloma: Malignant proliferation of plasma cells producing an M-protein.
- Waldenström macroglobulinemia: Overproduction of monoclonal IgM.
- Monoclonal gammopathy of undetermined significance (MGUS): Asymptomatic monoclonal protein elevation.
- Chronic lymphocytic leukemia (CLL): Occasionally produces monoclonal proteins.
Clinical Features
- Polyclonal Hypergammaglobulinemia
- Symptoms depend on the underlying condition:
- Chronic infections:
- Fever, weight loss, night sweats, fatigue.
- Autoimmune diseases:
- Joint pain, rash, photosensitivity (SLE).
- Swelling and stiffness (RA).
- Liver diseases:
- Jaundice, ascites, spider angiomas.
- Granulomatous diseases (e.g., sarcoidosis):
- Dry cough, shortness of breath, lymphadenopathy.
- Chronic infections:
- Monoclonal Hypergammaglobulinemia
Often asymptomatic in early stages (e.g., MGUS).
-
- Symptoms of plasma cell dyscrasias:
- Bone pain or fractures (multiple myeloma).
- Recurrent infections due to immune suppression.
- Symptoms of hyperviscosity syndrome:
- Blurred vision, headaches, dizziness, nosebleeds.
- Anemia, fatigue, or kidney dysfunction.
- Symptoms of plasma cell dyscrasias:
Biochemical Manifestations
- Polyclonal Hypergammaglobulinemia
-
- Serum Protein Electrophoresis (SPEP): Broad elevation of the gamma-globulin region (diffuse pattern).
- Quantitative Immunoglobulin Testing: Increased IgG, IgA, or IgM levels, depending on the condition.
- Other findings:
- Elevated ESR and CRP (indicating inflammation).
- Low albumin in chronic inflammatory or liver conditions.
- Monoclonal Hypergammaglobulinemia
-
- Serum Protein Electrophoresis (SPEP): Sharp peak (M-spike) in the gamma region, indicating monoclonal protein production.
- Immunofixation Electrophoresis (IFE): Identifies the specific monoclonal immunoglobulin (e.g., IgG, IgA, or IgM).
- Additional tests:
- Beta-2 microglobulin: Elevated in multiple myeloma, indicating disease burden.
- Renal function tests: May show impaired kidney function in multiple myeloma.
Diagnosis
- Polyclonal Hypergammaglobulinemia
-
- Serum protein electrophoresis (SPEP): Diffuse gamma globulin elevation.
- Quantitative immunoglobulins: Shows increased IgG, IgA, or IgM levels.
- Tests to identify underlying conditions:
- Infection markers: HIV, hepatitis B/C, tuberculosis tests.
- Autoimmune markers: ANA, RF, anti-dsDNA, or anti-CCP
- Liver function tests and imaging for liver disease.
- Monoclonal Hypergammaglobulinemia
-
- SPEP: Detects an M-spike.
- Immunofixation electrophoresis (IFE): Identifies the specific monoclonal protein.
- Bone marrow biopsy: Confirms clonal plasma cell proliferation (>10% plasma cells in multiple myeloma).
- Imaging: X-rays, CT, or MRI for lytic lesions in multiple myeloma.
Treatment
- Polyclonal Hypergammaglobulinemia
- Infections:
- Depending on the causative pathogen, treat it with antibiotics, antivirals, or antiparasitic agents.
- Autoimmune diseases:
- Immunosuppressive therapy (e.g., corticosteroids, methotrexate, or biologics such as TNF inhibitors).
- Liver diseases:
- Address the underlying cause (e.g., antiviral therapy for hepatitis, alcohol cessation).
- Monoclonal Hypergammaglobulinemia
- Multiple Myeloma:
- Chemotherapy (e.g., bortezomib, lenalidomide, dexamethasone).
- Autologous stem cell transplantation in eligible patients.
- Bisphosphonates for bone disease.
- Waldenström Macroglobulinemia:
- Plasmapheresis for hyperviscosity symptoms.
- Targeted therapy (e.g., rituximab, BTK inhibitors).
- MGUS:
- Regular monitoring (no treatment required unless progression to myeloma or other conditions occurs).