
Introduction
-
Down Syndrome (Trisomy 21) is a genetic disorder caused by having an extra copy of chromosome 21.
-
Normally, every person has 46 chromosomes (23 pairs). In Down’s Syndrome, there are 47 chromosomes because chromosome 21 is triplicated.
-
It leads to mental retardation (intellectual disability), growth delay, distinct facial features, and various health problems.
-
It was first described by Dr. John Langdon Down in 1866, and the extra chromosome 21 was discovered by Dr. Jérôme Lejeune in 1959.
-
It is the most common chromosomal abnormality seen in newborns.
Genetic Basis (Cause)
Down’s Syndrome occurs because of extra genetic material from chromosome 21.
There are three main genetic types:
| Type | Genetic Mechanism | Frequency (%) | Key Points |
|---|---|---|---|
| Trisomy 21 (Nondisjunction) | Failure of chromosome 21 to separate during egg/sperm formation (meiosis) | 95% | Most common type; not inherited |
| Translocation | Extra part of chromosome 21 attaches to another chromosome (commonly 14 or 22) | 3–4% | May be inherited from parent |
| Mosaicism | Some cells have normal 46 chromosomes; others have 47 | 1–2% | Symptoms are milder |
🔹 Nondisjunction
-
Happens when chromosome 21 fails to separate properly during egg/sperm formation.
-
This gives an extra copy of 21 in the baby.
-
Increases with maternal age, especially >35 years.
🔹 Translocation
-
The total chromosome number remains 46, but extra material from chromosome 21 is attached to another chromosome.
-
One parent may carry a balanced translocation, increasing recurrence risk.
🔹 Mosaicism
-
Caused by an error in cell division after fertilization.
-
Some cells are normal, others have trisomy 21 — so symptoms are less severe.
Epidemiology
| Parameter | Details |
|---|---|
| Incidence | 1 in every 700 live births |
| Gender ratio | Equal in males and females |
| Maternal age risk | ↑ Higher after 35 years |
| Inheritance | Mostly non-inherited (sporadic) |
Clinical Features
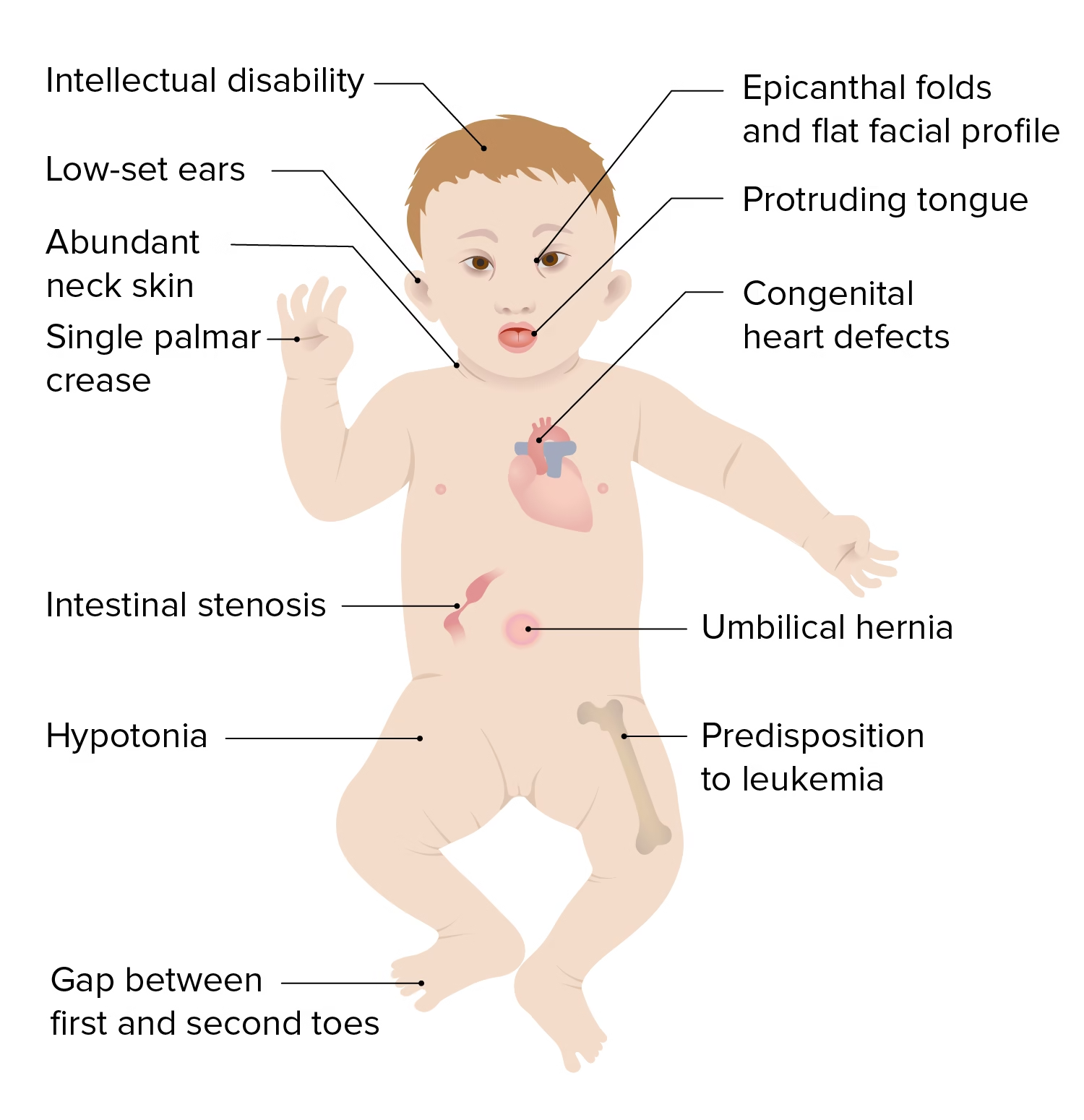
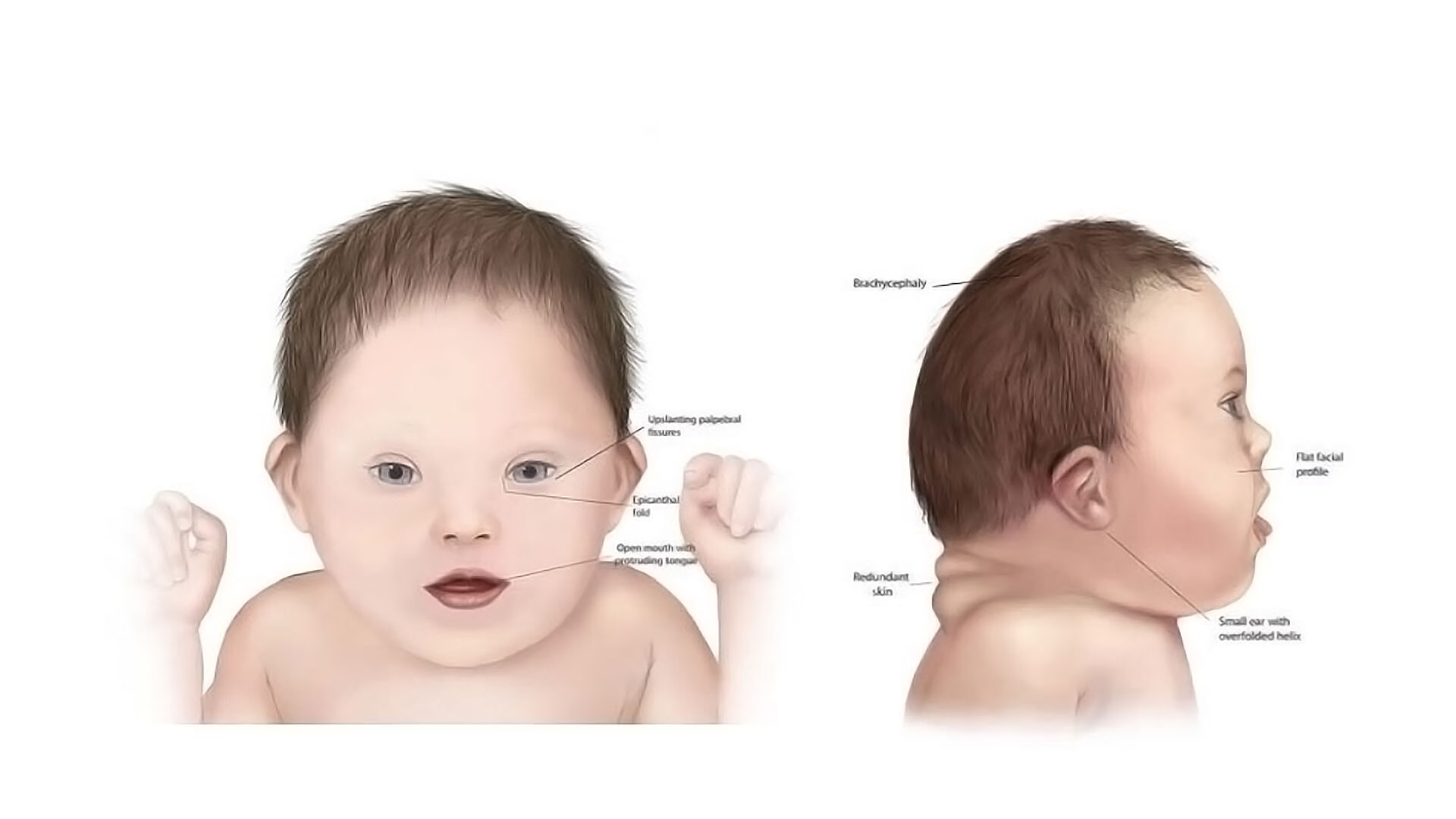
A. Physical Features
| System | Features |
|---|---|
| Face and Head | Flat facial profile, small nose, upward slanting eyes, epicanthic folds, small mouth with protruding tongue, small ears |
| Hands and Feet | Single palmar crease (“Simian crease”), short broad hands, wide gap between big and second toe |
| Neck | Short neck with loose skin folds |
| Body | Short stature, overweight tendency, soft muscle tone (hypotonia) in infancy |
| Hair/Skin | Dry skin, fine straight hair |
| Other | Delayed closure of fontanelles, small chin, broad flat skull |
B. Mental and Developmental Features
-
Mild to moderate intellectual disability (IQ 25–70)
-
Delayed milestones (late sitting, walking, talking)
-
Speech delay and learning difficulties
-
Friendly, cheerful, affectionate behavior
-
Good visual learning and social understanding
C. Medical Problems Common in Down’s Syndrome
| System | Common Problems |
|---|---|
| Heart | Congenital heart defects (Atrioventricular septal defect, ASD, VSD) – seen in 40–50% |
| Gastrointestinal | Duodenal atresia, Hirschsprung’s disease, constipation |
| Endocrine | Hypothyroidism (common) |
| Blood | Increased risk of leukemia (especially acute lymphoblastic leukemia) |
| Nervous system | Early Alzheimer’s-like dementia |
| Vision/Hearing | Strabismus, cataract, hearing loss |
| Immunity | Prone to infections |
| Musculoskeletal | Joint laxity, short limbs |
Pathophysiology
| Cause | Effect |
|---|---|
| Extra chromosome 21 | Overexpression of many genes |
| Gene imbalance | Affects brain, heart, and growth |
| Overproduction of certain proteins | Leads to developmental and immune problems |
| Example genes: SOD1, APP, DYRK1A | Cause oxidative stress, Alzheimer-like changes, and delayed brain development |
Laboratory and Diagnostic Tests
1. Prenatal Screening Tests
Used to detect high-risk pregnancies before birth.
| Test Name | Timing | Components | Interpretation |
|---|---|---|---|
| First Trimester Screening | 11–13 weeks | Ultrasound (nuchal translucency) + PAPP-A + β-hCG | ↑ hCG, ↓ PAPP-A suggest risk |
| Second Trimester Quadruple Test | 15–20 weeks | AFP, hCG, Estriol, Inhibin-A | ↓ AFP, ↓ Estriol, ↑ hCG, ↑ Inhibin-A = risk |
| Non-Invasive Prenatal Testing (NIPT) | Any time after 10 weeks | Cell-free fetal DNA in maternal blood | Highly accurate |
2. Confirmatory Diagnostic Tests
| Test | Description | Timing |
|---|---|---|
| Chorionic Villus Sampling (CVS) | Tests placental cells for karyotype | 10–12 weeks |
| Amniocentesis | Tests amniotic fluid for chromosomal study | 15–18 weeks |
| Karyotyping | Confirms extra chromosome 21 | Any stage |
| FISH / Microarray | Rapid detection of specific chromosome changes | Used for confirmation |
3. Postnatal Diagnosis
-
Based on physical features + confirmed by karyotype (47, XX+21 or 47, XY+21).
-
Newborns are screened for heart, thyroid, hearing, and vision defects.
Management and Treatment
There is no permanent cure, but early management and lifelong care can greatly improve quality of life.
A. Medical Management
| Problem | Management |
|---|---|
| Heart defects | Early surgery and cardiology follow-up |
| Hypothyroidism | Thyroid hormone replacement |
| Infections | Regular vaccination, antibiotics as needed |
| Leukemia risk | Routine blood monitoring |
| Vision/Hearing | Corrective lenses, hearing aids |
| GI problems | Surgical correction if required |
B. Developmental Support
-
Early intervention programs: Speech, physical, and occupational therapy from infancy.
-
Special education: Tailored learning plans and visual aids.
-
Social skill training: Improves independence and self-confidence.
-
Behavioral therapy: For discipline and emotional control.
C. Family and Genetic Counselling
| Aspect | Details |
|---|---|
| Parental education | Explainsthe nature of disorder and realistic expectations |
| Genetic counseling | Especially for translocation cases |
| Recurrence risk | About 1% for nondisjunction; up to 10–15% for translocation carriers |
| Emotional support | Support groups and special care organizations help parents cope |
Prognosis
| Parameter | Outcome |
|---|---|
| Life expectancy | Improved — around 55–60 years with medical care |
| Quality of life | Good with therapy and social inclusion |
| Complications | Heart defects, thyroid issues, infections, early aging |
| Survival improvement factors | Early detection, surgery, parental care, education |
Prevention
-
Genetic counseling before pregnancy, especially if mother >35 years.
-
Prenatal screening and testing during pregnancy.
-
Avoiding late maternal age pregnancy.
-
Use of assisted reproductive technology (PGD) for high-risk couples.
-
Folic acid supplementation and general maternal care improve outcomes.
MCQs
-
Down’s Syndrome is also known as:
A. Trisomy 18
B. Trisomy 21
C. Trisomy 13
D. Monosomy X -
Down’s Syndrome is caused by:
A. Mutation in a single gene
B. Deletion of a chromosome
C. Extra copy of chromosome 21
D. Lack of chromosome 21 -
The total number of chromosomes in a person with Down’s Syndrome is:
A. 45
B. 46
C. 47
D. 48 -
The genetic defect in Down’s Syndrome is due to:
A. Nondisjunction
B. Crossing over
C. Gene transposition
D. Deletion -
Down’s Syndrome is a type of:
A. Sex-linked disorder
B. Chromosomal disorder
C. Autosomal dominant disease
D. Metabolic disorder -
The risk of Down’s Syndrome increases with:
A. Paternal age
B. Maternal age
C. Childhood infections
D. Vitamin deficiency -
Which chromosomal abnormality is seen in Down’s Syndrome?
A. Monosomy
B. Trisomy
C. Tetrasomy
D. Translocation only -
The most common type of Down’s Syndrome is:
A. Mosaic type
B. Translocation type
C. Nondisjunction type
D. Structural type -
The most common cause of Down’s Syndrome is:
A. Nondisjunction of chromosome 21
B. Deletion of chromosome 21
C. Insertion of chromosome 21
D. Fusion of X and Y chromosomes -
The syndrome was first described by:
A. Watson and Crick
B. John Langdon Down
C. Gregor Mendel
D. Jerome Lejeune -
The chromosomal cause of Down’s Syndrome was discovered by:
A. Lejeune
B. Watson
C. Morgan
D. Muller -
Characteristic facial feature of Down’s Syndrome is:
A. Elongated face
B. Flat facial profile
C. Large forehead
D. Pointed chin -
Which of the following is a common hand feature in Down’s Syndrome?
A. Double palmar crease
B. Single transverse palmar crease (Simian crease)
C. Extra fingers
D. Curved nails -
Which of the following physical findings is common in Down’s Syndrome?
A. Long neck
B. Short neck with skin folds
C. Large jaw
D. Long fingers -
The muscle tone in Down’s Syndrome infants is usually:
A. Normal
B. Increased
C. Decreased
D. Variable -
Which congenital heart disease is most common in Down’s Syndrome?
A. Patent ductus arteriosus
B. Tetralogy of Fallot
C. Atrioventricular septal defect
D. Coarctation of aorta -
Which type of leukemia is common in Down’s Syndrome?
A. Chronic lymphocytic leukemia
B. Acute lymphoblastic leukemia
C. Chronic myeloid leukemia
D. Hairy cell leukemia -
Down’s Syndrome children commonly have:
A. Hyperthyroidism
B. Hypothyroidism
C. Diabetes
D. Addison’s disease -
Which of the following GI problems may occur in Down’s Syndrome?
A. Duodenal atresia
B. Peptic ulcer
C. Crohn’s disease
D. Gastritis -
Down’s Syndrome individuals are at higher risk of developing:
A. Alzheimer-like dementia
B. Parkinson’s disease
C. Huntington’s disease
D. Multiple sclerosis -
The genetic abnormality in Down’s Syndrome can be confirmed by:
A. Blood sugar test
B. Karyotyping
C. MRI scan
D. ECG -
The karyotype of a Down’s Syndrome female is:
A. 45, XX
B. 46, XX
C. 47, XX, +21
D. 47, XY, +21 -
The karyotype of a Down’s Syndrome male is:
A. 45, XY
B. 47, XY, +21
C. 46, XY
D. 48, XY -
Prenatal screening for Down’s Syndrome can be done by:
A. Urine test
B. First-trimester ultrasound and biochemical tests
C. X-ray
D. Physical exam -
Which prenatal test confirms Down’s Syndrome?
A. Amniocentesis
B. Blood test
C. Ultrasound only
D. ECG -
In Down’s Syndrome screening, which serum marker is increased?
A. AFP
B. Estriol
C. hCG
D. PAPP-A -
Which serum marker is decreased in Down’s Syndrome?
A. hCG
B. Inhibin A
C. Estriol
D. LDH -
Non-Invasive Prenatal Testing (NIPT) detects:
A. Maternal hormones
B. Fetal DNA in maternal blood
C. Placental enzymes
D. Amniotic proteins -
Which of the following is NOT a typical feature of Down’s Syndrome?
A. Upward slanting eyes
B. Short stature
C. Tall and thin body
D. Flat face -
The IQ level of most Down’s Syndrome individuals is:
A. Normal
B. Mild to moderate mental retardation
C. Severe retardation
D. Superior intelligence -
Mosaic type Down’s Syndrome means:
A. All cells have extra chromosome 21
B. Only some cells have extra chromosome 21
C. No extra chromosome present
D. All chromosomes are duplicated -
In translocation Down’s Syndrome, the extra chromosome 21 is attached to:
A. Chromosome 22
B. Chromosome 13 or 14
C. Chromosome 18
D. Chromosome 1 -
Life expectancy in modern times for Down’s Syndrome individuals is around:
A. 10 years
B. 20 years
C. 50–60 years
D. 80–90 years -
Early intervention for Down’s Syndrome includes:
A. Surgery only
B. Speech, physical, and occupational therapy
C. Blood transfusion
D. Hormone replacement -
Which of the following preventive measures helps reduce the risk of Down’s Syndrome?
A. Regular exercise
B. Avoiding smoking
C. Genetic counseling and prenatal testing
D. Protein-rich diet
Answer Key
-
B — Trisomy 21
-
C — Extra copy of chromosome 21
-
C — 47
-
A — Nondisjunction
-
B — Chromosomal disorder
-
B — Maternal age
-
B — Trisomy
-
C — Nondisjunction type
-
A — Nondisjunction of chromosome 21
-
B — John Langdon Down
-
A — Lejeune
-
B — Flat facial profile
-
B — Single transverse palmar crease (Simian crease)
-
B — Short neck with skin folds
-
C — Decreased
-
C — Atrioventricular septal defect
-
B — Acute lymphoblastic leukemia
-
B — Hypothyroidism
-
A — Duodenal atresia
-
A — Alzheimer-like dementia
-
B — Karyotyping
-
C — 47, XX, +21
-
B — 47, XY, +21
-
B — First-trimester ultrasound and biochemical tests
-
A — Amniocentesis
-
C — hCG
-
C — Estriol
-
B — Fetal DNA in maternal blood
-
C — Tall and thin body
-
B — Mild to moderate mental retardation
-
B — Only some cells have extra chromosome 21
-
B — Chromosome 13 or 14
-
C — 50–60 years
-
B — Speech, physical, and occupational therapy
-
C — Genetic counseling and prenatal testing