
Introduction
-
Escherichia coli (E. coli) is a Gram-negative, rod-shaped bacterium belonging to the family Enterobacteriaceae.
-
It is a normal commensal organism found in the intestinal tract of humans and warm-blooded animals.
-
Most strains of E. coli are harmless and play an important role in vitamin K production and gut health.
-
Some strains are pathogenic and can cause intestinal and extra-intestinal infections.
-
E. coli is a facultative anaerobe, capable of growing in the presence or absence of oxygen.
-
It is non-spore forming and usually motile due to peritrichous flagella.
-
Pathogenic strains are responsible for diseases such as diarrhea, urinary tract infections (UTI), septicemia, and neonatal meningitis.
-
E. coli is widely used as a model organism in microbiology, genetics, and biotechnology.
-
In medical laboratories, E. coli is an important indicator organism for fecal contamination of water and food.
General Character
- Genus: Escherichia
- Species: Escherichia coli (E. coli)
- Family: Enterobacteriaceae
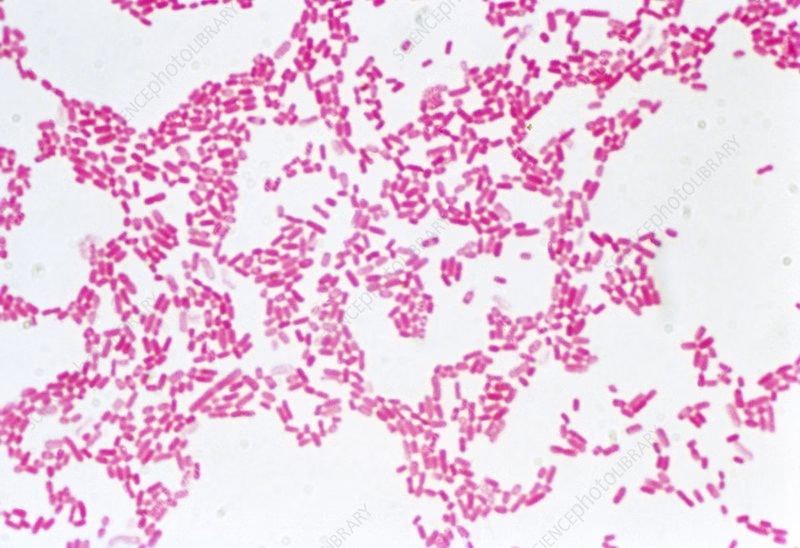
- Gram Staining: E. coli is a Gram-negative bacterium, appearing pink due to its thin peptidoglycan layer and outer membrane.
- Shape and Arrangement:
- Shape: E. coli are rod-shaped (bacilli).
- Arrangement: Typically found as single cells, but can also occur in pairs or chains.
- Oxygen Requirements: E. coli is a facultative anaerobe, capable of growing in aerobic and anaerobic conditions.
Morphology
- Cell Wall Structure:
- It comprises a thin layer of peptidoglycan, surrounded by an outer membrane containing lipopolysaccharides (LPS), contributing to its pathogenicity and immune evasion.
- Flagella:
- Many strains possess flagella, which provide motility, allowing E. coli to move toward favourable environments (chemotaxis).
- Capsule: Some strains have a polysaccharide capsule that helps protect against phagocytosis.
Cultural Characteristics
- Growth Media
- MacConkey Agar: Selective and differential medium that inhibits Gram-positive bacteria; E. coli ferments lactose, producing pink colonies.
- Blood Agar: Supports growth and allows observation of hemolytic activity.
- XLD Agar (Xylose Lysine Deoxycholate): Useful for distinguishing E. coli from other enteric pathogens.
- Colony Appearance
- On MacConkey agar, E. coli typically produces pink colonies due to the fermentation of lactose.
- Temperature and pH Range
- The optimal growth temperature is around 37°C, with a pH range of 6.0 to 7.5 being favourable.
Biochemical Reactions
- Catalase Test: E. coli is catalase-positive, producing bubbles when added hydrogen peroxide.
- Oxidase Test: E. coli is oxidase-negative, distinguishing it from other Gram-negative bacteria.
- Lactose Fermentation: E. coli ferments lactose, producing acid and gas, which can be detected on lactose-containing media.
- Indole Production: Most E. coli strains are indole-positive, indicating the ability to convert tryptophan into indole.
- Methyl Red Test: Positive, indicating mixed acid fermentation.
- Voges-Proskauer Test: Negative, indicating the absence of acetoin production.
Pathogenicity
- Virulence Factors
- Adhesins: Enable adherence to the intestinal epithelium, facilitating colonization.
- Toxins:
- Shiga Toxin (produced by E. coli O157): Can cause severe gastrointestinal disease and hemolytic uremic syndrome (HUS).
- Enterotoxins (e.g., heat-labile and heat-stable toxins) can cause diarrhoea, especially in enterotoxigenic E. coli (ETEC).
- Capsule and Biofilm Formation: Help protect against host immune responses.
- Clinical Infections
- Gastroenteritis: Caused by pathogenic strains such as enterotoxigenic E. coli (ETEC), enteropathogenic E. coli (EPEC), and enterohemorrhagic E. coli (EHEC).
- Urinary Tract Infections (UTIs): Uropathogenic E. coli (UPEC) is a leading cause of UTIs.
- Sepsis: This can occur in immunocompromised patients.
- Meningitis: Particularly in neonates, caused by certain serotypes.
Laboratory Diagnosis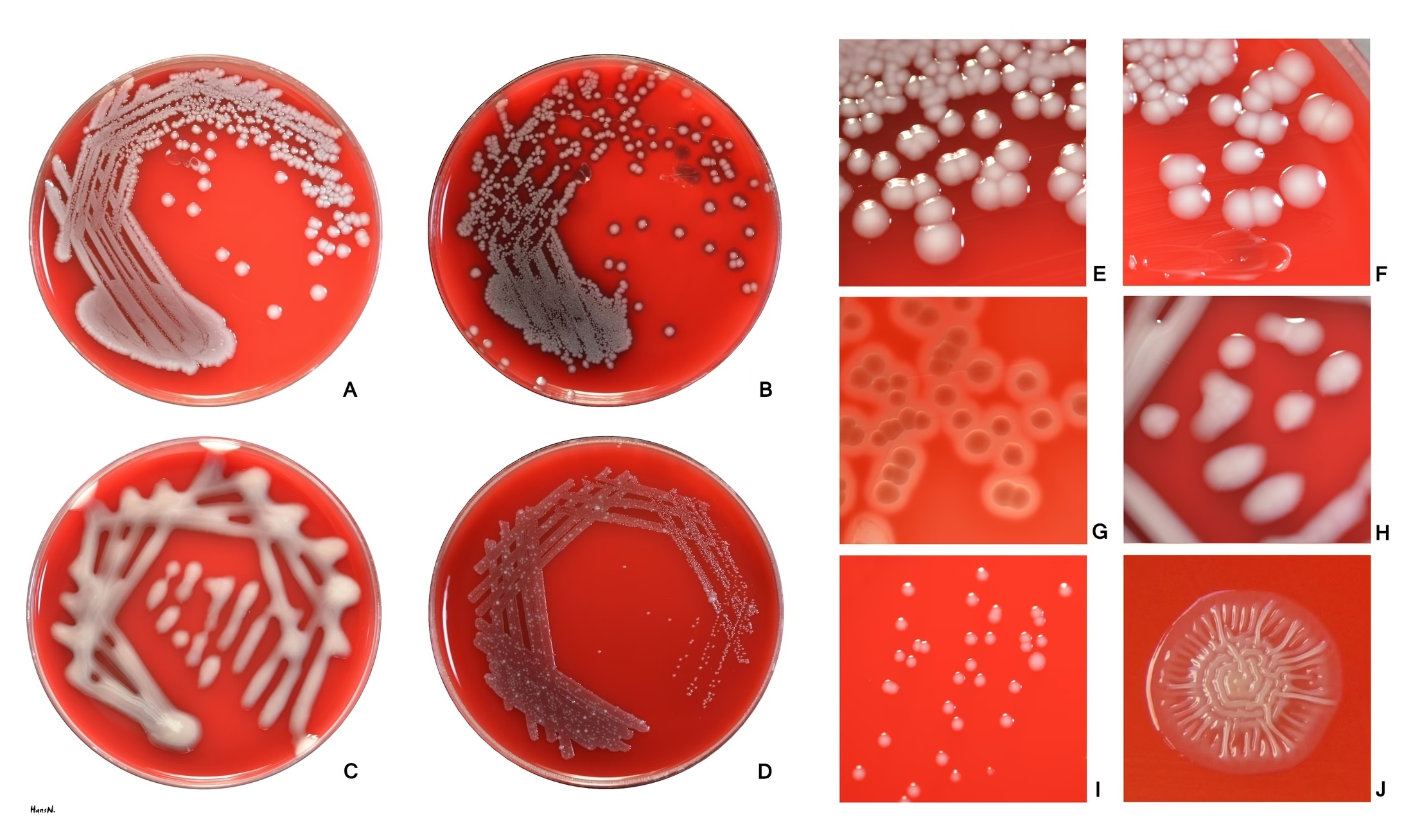
- Specimen Collection: Commonly involves stool samples for gastroenteritis or urine samples for UTIs.
- Microscopic Examination:
- Gram staining reveals Gram-negative bacilli.
- Culture Techniques:
- Inoculation on selective media like MacConkey or XLD agar, followed by incubation.
- Biochemical Testing:
- Confirmatory tests for lactose fermentation, indole production, and other biochemical reactions to identify E. coli.
- Molecular Methods: PCR and other nucleic acid amplification techniques can identify specific pathogenic strains, especially in outbreaks.
Antibiotic Resistance
- Emergence of Resistance: E. coli has shown increasing resistance to multiple antibiotics, including penicillins and fluoroquinolones.
- Multidrug-Resistant Strains: Especially concerning hospital-acquired infections and among strains producing extended-spectrum beta-lactamases (ESBLs) or carbapenemases.
- Treatment Options: The selection of antibiotics based on susceptibility testing is crucial due to varying resistance patterns.
Prevention
- Hygiene Practices: Proper handwashing and food safety measures (cooking food thoroughly, avoiding cross-contamination) are vital to prevent E. coli infections.
- Vaccination: Currently, no vaccines exist for E. coli; however, research is ongoing, particularly for pathogenic strains such as EHEC.
- Surveillance: Monitoring food sources and outbreaks can help manage risks associated with E. coli infections.
MCQs
Section A: General Characteristics
1. Escherichia coli belongs to which family?
A. Vibrionaceae
B. Enterobacteriaceae
C. Pseudomonadaceae
D. Neisseriaceae
2. E. coli is best described as:
A. Gram-positive cocci
B. Gram-negative bacilli
C. Acid-fast bacilli
D. Gram-variable bacilli
3. The natural habitat of E. coli is:
A. Soil
B. Water
C. Human intestine
D. Skin
4. E. coli is a:
A. Obligate aerobe
B. Obligate anaerobe
C. Facultative anaerobe
D. Microaerophile
5. Which structure is responsible for motility in E. coli?
A. Pili
B. Capsule
C. Flagella
D. Fimbriae
Section B: Morphology & Staining
6. E. coli shows which arrangement microscopically?
A. Chains
B. Clusters
C. Single rods
D. Palisades
7. E. coli is:
A. Spore forming
B. Non-spore forming
C. Acid fast
D. Encapsulated always
8. The Gram reaction of E. coli is due to:
A. Thick peptidoglycan
B. Absence of cell wall
C. Thin peptidoglycan with outer membrane
D. Teichoic acid
9. Capsule in E. coli is:
A. Always present
B. Never present
C. Present in some strains
D. Only in laboratory strains
10. The flagellar arrangement in E. coli is:
A. Monotrichous
B. Lophotrichous
C. Amphitrichous
D. Peritrichous
Section C: Culture Characteristics
11. E. coli grows best at:
A. 25°C
B. 30°C
C. 37°C
D. 45°C
12. On MacConkey agar, E. coli produces:
A. Colorless colonies
B. Pale colonies
C. Pink colonies
D. Black colonies
13. Lactose fermentation by E. coli indicates:
A. Gas production only
B. Acid production
C. Protein digestion
D. Spore formation
14. On EMB agar, E. coli shows:
A. No growth
B. Blue colonies
C. Green metallic sheen
D. Yellow colonies
15. E. coli is an indicator of:
A. Air pollution
B. Water hardness
C. Fecal contamination
D. Chemical toxicity
Section D: Biochemical Reactions
16. Indole test of E. coli is:
A. Negative
B. Weak positive
C. Positive
D. Variable
17. Methyl red test of E. coli is:
A. Negative
B. Positive
C. Variable
D. Delayed
18. Voges–Proskauer test of E. coli is:
A. Positive
B. Weak positive
C. Negative
D. Variable
19. Citrate utilization test of E. coli is:
A. Positive
B. Negative
C. Variable
D. Weak
20. Which IMViC pattern is typical for E. coli?
A. ++–
B. –++
C. +-+-
D. ++++
Section E: Antigenic Structure
21. O antigen of E. coli is part of:
A. Capsule
B. Flagella
C. Lipopolysaccharide
D. Pili
22. H antigen is associated with:
A. Capsule
B. Flagella
C. Cell wall
D. Ribosomes
23. K antigen represents:
A. Flagellar antigen
B. Capsular antigen
C. Somatic antigen
D. Enzyme
24. Endotoxin of E. coli is:
A. Exotoxin
B. Protein toxin
C. Lipopolysaccharide
D. Enzyme
25. Endotoxin mainly causes:
A. Paralysis
B. Fever and shock
C. Muscle spasm
D. Diarrhea only
Section F: Pathogenic Types
26. Which strain causes traveler’s diarrhea?
A. EHEC
B. ETEC
C. EIEC
D. EAEC
27. Hemolytic uremic syndrome is associated with:
A. EPEC
B. ETEC
C. EHEC
D. EIEC
28. Enteropathogenic E. coli mainly affects:
A. Adults
B. Neonates and infants
C. Elderly only
D. Pregnant women
29. Enteroinvasive E. coli resembles infection caused by:
A. Vibrio cholerae
B. Salmonella
C. Shigella
D. Campylobacter
30. Which toxin causes watery diarrhea?
A. Shiga toxin
B. Heat-labile toxin
C. Endotoxin
D. Cytotoxin
Section G: Clinical Significance
31. Most common cause of UTI is:
A. Klebsiella
B. Proteus
C. E. coli
D. Pseudomonas
32. E. coli can cause all EXCEPT:
A. UTI
B. Neonatal meningitis
C. Typhoid
D. Septicemia
33. Extra-intestinal infections of E. coli include:
A. Diarrhea only
B. Pneumonia only
C. UTI and septicemia
D. Skin infection only
34. Neonatal meningitis strain is commonly associated with:
A. O antigen
B. H antigen
C. K1 antigen
D. F antigen
35. Source of infection is usually:
A. Airborne
B. Vector-borne
C. Endogenous flora
D. Sexual contact
Section H: Laboratory Diagnosis
36. Specimen for diagnosing E. coli diarrhea is:
A. Blood
B. Urine
C. Stool
D. CSF
37. Primary culture medium for E. coli is:
A. Blood agar
B. Lowenstein–Jensen
C. MacConkey agar
D. TCBS agar
38. Gas production by E. coli is seen in:
A. Glucose fermentation
B. Lactose fermentation
C. Both A and B
D. None
39. Which test differentiates E. coli from Klebsiella?
A. Catalase test
B. Indole test
C. Oxidase test
D. Urease test
40. E. coli oxidase test is:
A. Positive
B. Negative
C. Weak positive
D. Variable
Section I: Applied & Miscellaneous
41. E. coli is widely used in research because it:
A. Is pathogenic
B. Grows slowly
C. Is genetically well studied
D. Is acid fast
42. Indicator organism for water quality is:
A. Staphylococcus
B. E. coli
C. Clostridium
D. Bacillus
43. Which enzyme test is positive in E. coli?
A. Oxidase
B. Urease
C. Catalase
D. Coagulase
44. Antibiotic resistance in E. coli is commonly due to:
A. Spore formation
B. Capsule
C. Plasmids
D. Flagella
45. E. coli is sensitive to:
A. Penicillin always
B. All antibiotics
C. Antibiotics based on sensitivity testing
D. Antifungals
Section J: True Concept MCQs
46. E. coli is part of normal gut flora.
A. True
B. False
47. All E. coli strains are pathogenic.
A. True
B. False
48. E. coli ferments lactose rapidly.
A. True
B. False
49. E. coli produces exotoxin only.
A. True
B. False
50. Presence of E. coli in water indicates fecal pollution.
A. True
B. False
Answer Key
-
B
-
B
-
C
-
C
-
C
-
C
-
B
-
C
-
C
-
D
-
C
-
C
-
B
-
C
-
C
-
C
-
B
-
C
-
B
-
A
-
C
-
B
-
B
-
C
-
B
-
B
-
C
-
B
-
C
-
B
-
C
-
C
-
C
-
C
-
C
-
C
-
C
-
C
-
B
-
B
-
C
-
B
-
C
-
C
-
C
-
A
-
B
-
A
-
B
-
A