Introduction
-
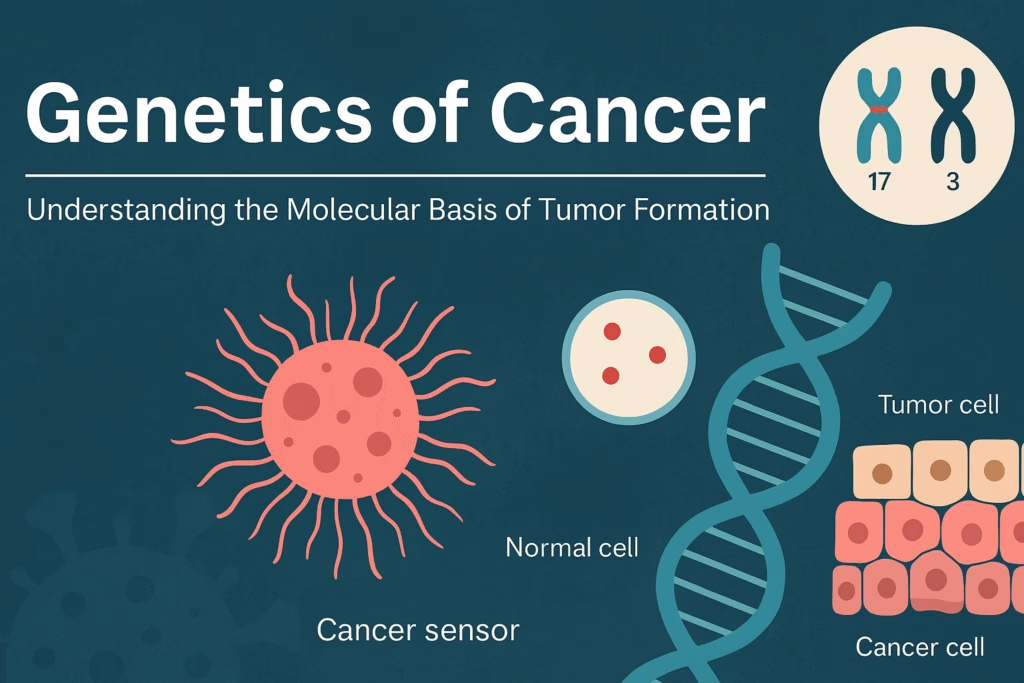
Cancer is a genetic disease caused by mutations in genes that control normal cell growth, division, and death.
-
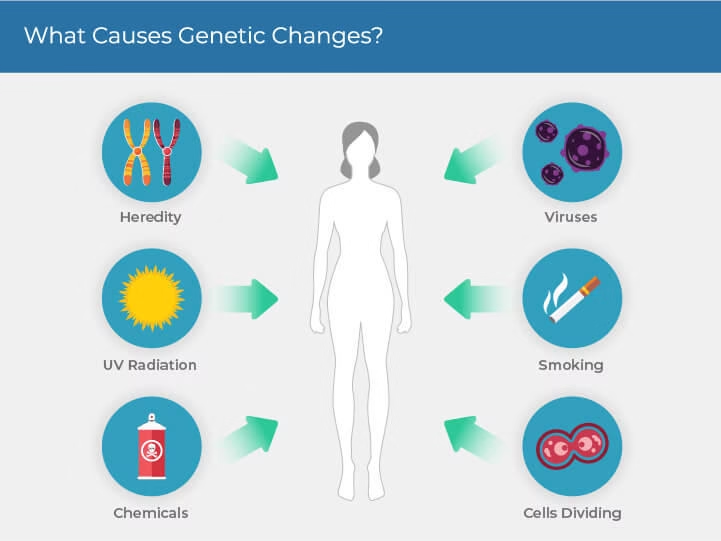
These mutations can be inherited (germline) or acquired (somatic) due to environmental factors like chemicals, radiation, or viruses.
-
Four main gene groups are involved in cancer development — proto-oncogenes, tumor suppressor genes, DNA repair genes, and apoptosis-regulating genes.
-
Accumulation of multiple genetic alterations leads to uncontrolled cell proliferation, loss of apoptosis, and formation of malignant tumors.
-
Understanding the genetic basis of cancer is crucial for early diagnosis, genetic screening, and targeted therapy in modern oncology.
What Is Cancer?
-
Cancer is a condition where cells lose control over growth and division, leading to the formation of a tumor (neoplasm).
-
Normally, cell division is regulated by a balance between growth-promoting genes and growth-suppressing genes.
-
When this balance is disturbed due to genetic mutations, cells begin to divide uncontrollably.
Genetic Basis of Cancer
Cancer develops through genetic mutations that can be:
-
Inherited (Germline mutations):
-
Present in the egg or sperm.
-
Found in every cell of the body.
-
Responsible for hereditary cancers (e.g., BRCA1 mutation in breast cancer).
-
-
Acquired (Somatic mutations):
-
Occur during a person’s lifetime due to environmental exposures (radiation, chemicals, viruses) or replication errors.
-
Affect only specific tissues or organs.
-
Account for more than 90% of cancers.
-
Types of Cancer-Related Genes
Cancer arises due to abnormalities in four major classes of genes:
1. Proto-oncogenes
-
These are normal genes that promote cell growth and division.
-
When mutated, they become oncogenes, leading to uncontrolled cell proliferation.
-
Mutation type: Gain-of-function (dominant mutation).
-
Examples:
-
RAS → Colon, lung, pancreatic cancers
-
MYC → Burkitt’s lymphoma
-
HER2/neu → Breast carcinoma
-
ABL → Chronic myeloid leukemia (CML)
-
2. Tumor Suppressor Genes
-
These genes act as brakes that inhibit abnormal cell growth.
-
When inactivated or deleted, cells lose control over the cell cycle.
-
Mutation type: Loss-of-function (recessive mutation).
-
Key Examples:
-
TP53 → “Guardian of the genome”; mutated in >50% of cancers
-
RB1 → Retinoblastoma, osteosarcoma
-
APC → Familial adenomatous polyposis (colon cancer)
-
BRCA1 and BRCA2 → Breast and ovarian cancers
-
3. DNA Repair Genes
-
These genes maintain genomic integrity by correcting DNA damage.
-
When defective, DNA mutations accumulate, increasing cancer risk.
-
Examples:
-
MLH1, MSH2 → Hereditary nonpolyposis colon cancer (Lynch syndrome)
-
XPA, XPC → Xeroderma pigmentosum (sensitivity to UV light)
-
4. Apoptosis-Regulating Genes
-
Control programmed cell death (apoptosis).
-
Mutation can prevent damaged cells from dying.
-
Examples:
-
BCL-2 → Overexpression prevents apoptosis in follicular lymphoma
-
BAX, BAD → Pro-apoptotic genes; loss promotes survival of mutant cells
-

Mechanisms Leading to Genetic Mutations in Cancer
-
Point Mutations:
Alter a single base pair in DNA (e.g., RAS gene mutation). -
Chromosomal Translocations:
Exchange of DNA between chromosomes; produces oncogenic fusion proteins.-
Example: t(9;22) → BCR-ABL fusion in Chronic Myeloid Leukemia (Philadelphia chromosome)
-
-
Gene Amplification:
Multiple copies of oncogenes cause excessive protein production.-
Example: HER2/neu amplification in breast cancer.
-
-
Deletions or Loss of Heterozygosity:
Loss of tumor suppressor gene regions (e.g., RB1 in retinoblastoma). -
Epigenetic Changes:
-
DNA methylation and histone modification alter gene expression without changing DNA sequence.
-
Hypermethylation → Silencing of tumor suppressor genes.
-
Hypomethylation → Activation of oncogenes.
-
Hallmarks of Cancer
According to Hanahan and Weinberg, cancer cells acquire the following genetic hallmarks:
-
Sustained proliferative signalling
-
Evasion of growth suppressors
-
Resistance to cell death (apoptosis)
-
Limitless replicative potential
-
Induction of angiogenesis
-
Activation of invasion and metastasis
-
Genome instability and mutation
-
Deregulated cellular energetics (Warburg effect)
Examples of Specific Genetic Cancers
| Cancer Type | Gene Involved | Mutation Effect |
|---|---|---|
| Retinoblastoma | RB1 | Loss of tumor suppressor control |
| Breast cancer | BRCA1, BRCA2 | Defective DNA repair |
| CML | BCR-ABL fusion | Constitutive tyrosine kinase activity |
| Burkitt’s lymphoma | MYC | Overexpression due to translocation |
| Colon cancer | APC, p53, KRAS | Stepwise accumulation of mutations |
| Melanoma | CDKN2A | Defective cell cycle regulation |
Environmental and Viral Causes of Genetic Damage
-
Chemical Carcinogens:
-
Benzene, aflatoxins, tobacco smoke cause DNA adducts and mutations.
-
-
Radiation:
-
UV radiation → thymine dimers
-
Ionizing radiation → double-strand DNA breaks
-
-
Oncogenic Viruses:
-
HPV: Cervical cancer (E6, E7 oncogenes inactivate p53, RB)
-
EBV: Burkitt’s lymphoma, nasopharyngeal carcinoma
-
HBV/HCV: Hepatocellular carcinoma
-
HTLV-1: Adult T-cell leukemia
-
Genetic Testing and Molecular Diagnosis
Genetic analysis has revolutionised cancer detection and management.
Modern techniques include:
-
PCR (Polymerase Chain Reaction)
-
FISH (Fluorescence in situ hybridization)
-
DNA sequencing
-
Next-generation sequencing (NGS)
-
Gene expression profiling
These tools help:
-
Detect inherited mutations (e.g., BRCA1/2 testing).
-
Identify therapeutic targets (e.g., HER2 status).
-
Predict treatment response and prognosis.
Targeted and Genetic Therapies
Modern cancer treatment now includes genetic and molecular-based approaches:
-
Imatinib (Gleevec): Inhibits BCR-ABL in CML
-
Trastuzumab (Herceptin): Targets HER2 receptor in breast cancer
-
PARP inhibitors: Exploit DNA repair defects in BRCA-mutated cancers
-
Checkpoint inhibitors: Block PD-1/PD-L1 to enhance immune response
-
CAR-T cell therapy: Uses genetically modified T-cells to attack tumor cells
MCQs
-
Cancer is primarily considered a disease of:
A. Blood circulation
B. Genetic mutations
C. Immune deficiency
D. Hormonal imbalance -
Which of the following best describes the genetic nature of cancer?
A. Metabolic disorder
B. Infectious disease
C. Genetic disease of somatic cells
D. Autoimmune disorder -
Mutations in which genes promote uncontrolled cell growth?
A. Tumor suppressor genes
B. Proto-oncogenes
C. DNA repair genes
D. Housekeeping genes -
When a proto-oncogene is mutated, it becomes a/an:
A. Enzyme
B. Oncogene
C. Tumor suppressor
D. Hormone -
The p53 gene is classified as a:
A. Proto-oncogene
B. Tumor suppressor gene
C. DNA repair gene
D. Oncogene -
The “Guardian of the Genome” refers to which gene?
A. RB1
B. BRCA1
C. TP53
D. MYC -
Mutation in the RB1 gene leads to which type of cancer?
A. Lung cancer
B. Retinoblastoma
C. Breast cancer
D. Leukemia -
BRCA1 and BRCA2 genes are associated with:
A. Brain cancer
B. Breast and ovarian cancers
C. Lung cancer
D. Skin cancer -
The BCR-ABL fusion gene is produced by:
A. Gene duplication
B. Point mutation
C. Chromosomal translocation
D. Gene deletion -
The Philadelphia chromosome is found in:
A. Chronic myeloid leukemia (CML)
B. Retinoblastoma
C. Colon cancer
D. Melanoma -
The HER2/neu gene is associated with which cancer?
A. Breast cancer
B. Cervical cancer
C. Thyroid cancer
D. Brain tumor -
The MYC gene is an example of a/an:
A. Oncogene
B. Tumor suppressor gene
C. DNA repair gene
D. Enzyme gene -
Tumor suppressor genes are inactivated by:
A. Point mutations
B. Gene deletions
C. Promoter methylation
D. All of the above -
Which of the following genes controls apoptosis?
A. BCL-2
B. BRCA1
C. RB1
D. KRAS -
Overexpression of BCL-2 leads to:
A. Increased apoptosis
B. Decreased apoptosis
C. Increased DNA repair
D. Enhanced immune response -
Which of the following is a DNA repair gene?
A. MLH1
B. KRAS
C. TP53
D. HER2 -
Defects in mismatch repair genes lead to which condition?
A. Xeroderma pigmentosum
B. Lynch syndrome (HNPCC)
C. Leukemia
D. Melanoma -
The APC gene is associated with which cancer?
A. Colon cancer
B. Lung cancer
C. Pancreatic cancer
D. Prostate cancer -
The transformation of a normal cell into a cancer cell is known as:
A. Mutation
B. Oncogenesis
C. Apoptosis
D. Differentiation -
Gene amplification results in:
A. Reduced gene expression
B. Multiple copies of an oncogene
C. Deletion of a gene
D. Normal gene activity -
Which virus is associated with cervical cancer?
A. Epstein-Barr virus (EBV)
B. Hepatitis B virus (HBV)
C. Human papillomavirus (HPV)
D. Human T-cell leukemia virus (HTLV-1) -
The viral oncogenes E6 and E7 inactivate which cellular genes?
A. p53 and RB1
B. MYC and KRAS
C. APC and MLH1
D. BRCA1 and BRCA2 -
The main cause of cancer at the molecular level is:
A. Abnormal gene expression
B. Hormonal imbalance
C. Vitamin deficiency
D. Protein denaturation -
Loss of heterozygosity is commonly seen in:
A. Tumor suppressor genes
B. Oncogenes
C. DNA repair genes
D. Structural genes -
Which of the following is NOT a hallmark of cancer?
A. Uncontrolled proliferation
B. Evasion of apoptosis
C. Limited replicative potential
D. Metastasis -
The term “multi-step carcinogenesis” means:
A. One mutation causes cancer
B. Cancer develops after accumulation of multiple mutations
C. Cancer spreads rapidly
D. Genetic repair is enhanced -
The gene product of p53 acts as a:
A. Transcription factor
B. Kinase enzyme
C. Cell surface receptor
D. Growth factor -
RAS oncogene causes cancer by:
A. Activating cell proliferation pathways
B. Inhibiting apoptosis
C. Blocking DNA repair
D. Preventing cell adhesion -
Which chemical agent causes DNA adduct formation leading to mutations?
A. Benzene
B. Aflatoxin B1
C. Nicotine
D. Methanol -
UV radiation mainly causes which type of DNA damage?
A. Double-strand break
B. Thymine dimer formation
C. Cross-linking of proteins
D. Frameshift mutation -
Which virus is associated with Burkitt’s lymphoma?
A. EBV (Epstein–Barr virus)
B. HPV
C. HBV
D. HCV -
Which of the following tests can detect specific gene mutations in cancer?
A. ELISA
B. PCR
C. ESR
D. CBC -
Targeted therapy for HER2-positive breast cancer uses which drug?
A. Trastuzumab (Herceptin)
B. Imatinib (Gleevec)
C. Tamoxifen
D. Methotrexate -
The BCR-ABL fusion protein in CML acts as a:
A. Tyrosine kinase
B. DNA polymerase
C. Protease
D. Transcription factor -
The future of cancer treatment focuses mainly on:
A. Chemotherapy only
B. Gene therapy and personalized medicine
C. Herbal medicine
D. Radiation alone
Answer Key
-
B — Genetic mutations
-
C — Genetic disease of somatic cells
-
B — Proto-oncogenes
-
B — Oncogene
-
B — Tumor suppressor gene
-
C — TP53
-
B — Retinoblastoma
-
B — Breast and ovarian cancers
-
C — Chromosomal translocation
-
A — Chronic myeloid leukemia (CML)
-
A — Breast cancer
-
A — Oncogene
-
D — All of the above
-
A — BCL-2
-
B — Decreased apoptosis
-
A — MLH1
-
B — Lynch syndrome (HNPCC)
-
A — Colon cancer
-
B — Oncogenesis
-
B — Multiple copies of an oncogene
-
C — Human papillomavirus (HPV)
-
A — p53 and RB1
-
A — Abnormal gene expression
-
A — Tumor suppressor genes
-
C — Limited replicative potential
-
B — Cancer develops after accumulation of multiple mutations
-
A — Transcription factor
-
A — Activating cell proliferation pathways
-
B — Aflatoxin B1
-
B — Thymine dimer formation
-
A — EBV (Epstein–Barr virus)
-
B — PCR
-
A — Trastuzumab (Herceptin)
-
A — Tyrosine kinase
-
B — Gene therapy and personalized medicine