Introduction
The Glucose Tolerance Test (GTT) is commonly used to detect impaired glucose tolerance (IGT), gestational diabetes, and diabetes mellitus. The test involves administering a fixed dose of glucose and measuring the blood glucose concentration at specific time intervals.
The oral glucose tolerance test (OGTT) is the most widely used method, but there are also intravenous glucose tolerance tests (IVGTT), depending on the clinical scenario.
Principle
The Glucose Tolerance Test works on the principle that the function of insulin and other regulatory mechanisms influences the body’s ability to metabolize glucose. In a normal individual, blood glucose levels rise after ingesting glucose but return to normal within a few hours due to insulin secretion. In people with impaired glucose tolerance or diabetes, the glucose levels remain elevated longer than normal due to inadequate insulin secretion or insulin resistance.
Requirements
- Sample:
- Blood samples are collected at baseline (fasting) and at specific time intervals (usually 1 hour, 2 hours, and sometimes 3 hours) after the glucose load.
- Some tests also use urine for glucose measurements, although blood glucose is more common.
- Reagents:
- Glucose solution (typically 75g of glucose in 250-300 mL water for an adult patient).
- Glucose oxidase reagent (for the blood glucose determination by colorimetric or enzymatic methods).
- Apparatus:
- Glucose meter or spectrophotometer for measuring blood glucose levels.
- Syringes or vacutainers for blood collection.
- Timer to monitor the intervals after glucose administration.
- Centrifuge (if sample separation is required).
- Water bath (optional, for incubation in some methods).
Procedure
- Preparation of the Patient
-
- The patient should fast for 8-12 hours before the test, with no food or drink intake (except water).
- Any medications that could interfere with the test (e.g., diuretics, steroids, etc.) should be temporarily stopped, if possible, under the supervision of a doctor.
- Fasting Blood Glucose Measurement
-
- A blood sample measures the baseline glucose level (fasting glucose).
- The fasting glucose level is important as it provides a baseline for comparison.
- Administration of Glucose
-
- The patient is given a 75g oral glucose solution (for adults), usually dissolved in 250-300 mL of water.
- For gestational diabetes, a 50g glucose solution may be used, and this test is done with a single 1-hour measurement (called a one-hour glucose challenge test).
- Post-Glucose Blood Sampling
-
- Blood samples are taken at regular intervals, typically 1 hour, 2 hours, and sometimes 3 hours after glucose ingestion.
- The patient should remain seated and avoid physical activity during testing to avoid influencing glucose levels.
- Measurement of Blood Glucose Levels
-
- Blood glucose levels are determined using a glucose oxidase method (colorimetric or enzymatic) or an automatic blood glucose analyzer.
- Interpretation of Results
-
- Blood glucose values at each time point are recorded and analyzed based on standard reference ranges (which can vary slightly depending on the lab or country).
- Blood glucose values at each time point are recorded and analyzed based on standard reference ranges (which can vary slightly depending on the lab or country).
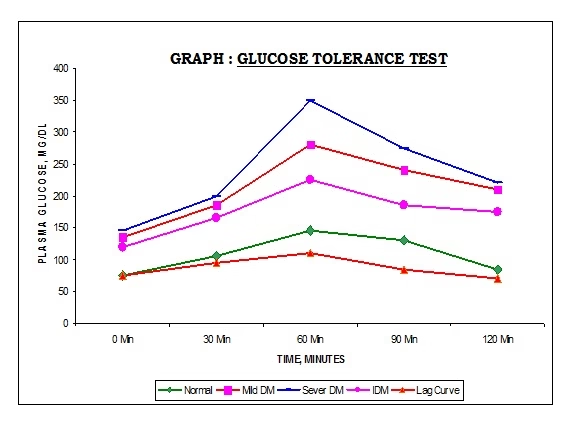
Interpretation of Results
The normal range for a 75g Oral Glucose Tolerance Test (OGTT) is as follows:
- Fasting blood glucose:
- Normal: 70–99 mg/dL (3.9–5.5 mmol/L)
- Impaired fasting glucose: 100–125 mg/dL (5.6–6.9 mmol/L)
- Diabetes: ≥ 126 mg/dL (≥ 7 mmol/L)
- 1-hour post-glucose:
- Normal: < 180 mg/dL (10.0 mmol/L)
- Impaired glucose tolerance: 180–199 mg/dL (10.0–11.0 mmol/L)
- Diabetes: ≥ 200 mg/dL (≥ 11.1 mmol/L)
- 2-hour post-glucose:
- Normal: < 140 mg/dL (7.8 mmol/L)
- Impaired glucose tolerance (IGT): 140–199 mg/dL (7.8–11.0 mmol/L)
- Diabetes: ≥ 200 mg/dL (≥ 11.1 mmol/L)
Diagnosis:
- Normal glucose tolerance: If glucose levels return to normal by 2 hours.
- Impaired glucose tolerance (IGT): If glucose levels are elevated above normal but do not meet the criteria for diabetes.
- Diabetes: If glucose levels meet the diagnostic criteria at any time during the test.
For gestational diabetes, the following criteria are commonly used (depending on local guidelines):
- Fasting glucose ≥ 92 mg/dL (5.1 mmol/L)
- 1-hour glucose ≥ 180 mg/dL (10.0 mmol/L)
- 2-hour glucose ≥ 153 mg/dL (8.5 mmol/L)
Clinical Significance
- Diagnosis of Diabetes Mellitus:
- The GTT is a key tool for diagnosing type 2 diabetes mellitus and differentiating between normal glucose metabolism, impaired glucose tolerance (IGT), and diabetes.
- Gestational Diabetes Screening:
- The test is crucial in the diagnosis of gestational diabetes. Pregnant women are often tested between 24-28 weeks of pregnancy.
- Monitoring of Glucose Metabolism:
- The GTT can be used to monitor patients with known insulin resistance or impaired fasting glucose to prevent progression to diabetes.
- Evaluation of Endocrine Disorders:
- The GTT can evaluate endocrine disorders involving glucose metabolism, including conditions like Cushing’s syndrome and acromegaly, which affect insulin secretion.
- Insulin Resistance and Metabolic Syndrome:
- The test is useful in assessing insulin resistance, a component of metabolic syndrome, and is often seen in conditions like obesity, hypertension, and dyslipidemia.
Limitations
- Patient Compliance: The test requires fasting and a specific glucose intake, affecting compliance.
- Time-consuming: The test takes several hours and requires multiple blood samples.
- Inaccurate Results in Certain Populations: Conditions like pregnancy, stress, or severe illness can influence test results and lead to false positives.
- Age and Medications: Certain medications, like oral contraceptives and diuretics or age-related changes in insulin sensitivity, can interfere with the results.