Introduction
- Gonorrhea is a common sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae.
- It has significant health implications due to its potential to cause severe complications if left untreated, including infertility and increased susceptibility to HIV.
- The infection can affect various mucosal sites, including the urogenital tract, rectum, and oropharynx.
Causative Agent
Neisseria gonorrhoeae
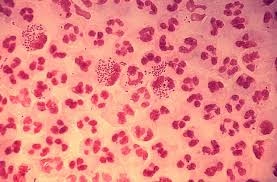
- Characteristics: This Gram-negative diplococcus is facultatively anaerobic and oxidase-positive. It is sensitive to environmental conditions, making it challenging to culture outside the human body.
- Transmission: Primarily through sexual contact, including vaginal, anal, and oral sex. It can also be transmitted from mother to child during childbirth, leading to neonatal conjunctivitis.
Clinical Presentation
Urogenital Infections
- Men: Typically present with acute urethritis characterized by:
- Dysuria: Painful urination.
- Purulent Discharge: Thick, yellow-green discharge from the penis, often referred to as “gonococcal urethritis.”
- Symptoms can appear within 2 to 7 days after exposure, but some may remain asymptomatic.
- Women: Often asymptomatic or present with:
- Cervicitis: Inflammation of the cervix, leading to increased vaginal discharge, dysuria, and intermenstrual bleeding.
- Pelvic Pain: If the infection progresses to PID, symptoms may include severe abdominal pain, fever, and nausea.
Extragenital Infections
- Pharyngeal Gonorrhea:
- Often asymptomatic, it may cause sore throat or pharyngeal discomfort.
- Increased prevalence in individuals engaging in oral sex.
- Rectal Gonorrhea:
- Symptoms may include rectal pain, discharge, and bleeding. Many cases are asymptomatic, complicating diagnosis.
Complications
- Women: Untreated gonorrhea can lead to PID, which may cause chronic pelvic pain, infertility, or ectopic pregnancy.
- Men: Complications may include epididymitis or prostatitis.
- Disseminated Gonococcal Infection (DGI): Rare but serious, characterized by arthritis, tenosynovitis, and, in severe cases, sepsis.
Sample Collection
The choice of the specimen depends on the site of the suspected infection:
- Urethral Swabs:
- For men, a swab from the urethra is collected, ideally, after the first morning urine, to maximize yield.
- Cervical Swabs:
- For women, a swab is taken from the endocervical canal during a pelvic examination.
- Throat Swabs:
- For suspected pharyngeal infections, a swab from the oropharynx is collected, making sure to avoid the tongue and tonsils to prevent contamination.
- Rectal Swabs:
- For suspected rectal infections, a swab is taken from the rectal mucosa, ideally inserted 2-3 cm into the rectum.
- Urine Samples:
- First-catch urine samples can be used for NAATs, particularly in men and women.
Handling and Transport
- Swabs should be collected using sterile techniques and appropriate swab types (e.g., calcium alginate or Dacron swabs, as cotton swabs can inhibit bacterial growth).
- Specimens should be transported to the laboratory promptly to ensure the viability of the organisms.
Laboratory Techniques
Culture Methods
While culture is not the first-line diagnostic method due to the rise of NAATs, it remains important for antibiotic susceptibility testing and cases of treatment failure.
- Culture Medium:
- Thayer-Martin Agar: A selective medium containing antibiotics to suppress normal flora and support the growth of N. gonorrhoeae.
- Incubation:
- Specimens are incubated in a humidified CO₂-enriched environment at 35-37°C for 24 to 48 hours.
- Identification:
- Presumptive identification based on colony morphology (small, grayish colonies).
- Gram Staining: Gram-negative diplococcus is often seen, confirming the presence of N. gonorrhoeae.
- Oxidase Test: Positive for N. gonorrhoeae, aiding differentiation from other organisms.
Nucleic Acid Amplification Tests (NAATs)
NAATs are the preferred method for diagnosing gonorrhea due to their high sensitivity and specificity.
- Types of NAATs:
- Polymerase Chain Reaction (PCR): Amplifies specific DNA sequences of N. gonorrhoeae.
- Transcription-Mediated Amplification (TMA): Similar to PCR, but amplifies RNA.
- Sample Types: NAATs can be performed on various specimens (urethral, cervical, rectal, pharyngeal, and urine).
- Advantages:
- Highly sensitive, particularly in asymptomatic individuals.
- Allows for the detection of co-infections (e.g., with Chlamydia trachomatis).
- Limitations:
- Higher cost than culture methods.
- It cannot distinguish between live and dead organisms, which may complicate interpretation.
Rapid Tests
Rapid tests for gonorrhea, including immunochromatographic tests, are available but are less commonly used due to variable sensitivity.
- Function: Detect gonococcal antigens directly from clinical specimens.
- Advantages: Quick results; useful in resource-limited settings.
- Limitations: Often less sensitive than NAATs; positive results should be confirmed with a more sensitive test.
Interpretation of Results
- Culture Results
- Positive Culture: Confirms active infection with N. gonorrhoeae. Identification can be verified through further biochemical testing and antibiotic susceptibility profiling.
- Negative Culture: This does not rule out gonorrhea, especially if the specimen was collected during the incubation period or if the patient has already received antibiotics.
- NAAT Results
- Positive NAAT: Indicates the presence of N. gonorrhoeae. In symptomatic individuals, this is diagnostic. In asymptomatic individuals, clinical correlation may be necessary.
- Negative NAAT: Suggests the absence of gonorrhea but may not rule it out entirely, especially if the sample was improperly collected or if testing occurred shortly after exposure.
- Rapid Test Results
- Positive Result: Suggests the presence of N. gonorrhoeae but should be confirmed with NAATs or culture for accuracy.
- Negative Result: Should be interpreted with caution; may necessitate further testing if clinical suspicion remains high.
Clinical Implications
Treatment
The treatment of gonorrhea has evolved due to rising antibiotic resistance. Current guidelines recommend:
- Ceftriaxone: 500 mg IM as a single dose for uncomplicated gonorrhea.
- Azithromycin: 1 g orally as a single dose (previously used but now less common due to resistance).
Follow-Up
- Patients should be re-evaluated 1-2 weeks after treatment to ensure the resolution of symptoms.
- Retesting is recommended after three months, especially for those at high risk of reinfection.
Public Health Considerations
- Gonorrhea is a notifiable disease, necessitating reporting to public health authorities.
- Public health strategies focus on:
- Education: Promoting awareness of safe sexual practices.
- Screening Programs: Regular testing for at-risk populations.
- Partner Notification and Treatment: Ensuring sexual partners are informed and treated to prevent reinfection.
Challenges in Diagnosis
- Asymptomatic Cases: A significant portion of gonorrhea cases are asymptomatic, complicating early detection.
- Antibiotic Resistance: Increasing resistance to first-line treatments necessitates ongoing surveillance and adjustments to treatment protocols.
Advances in Gonorrhea Diagnostics
Emerging Technologies
- Point-of-Care Testing: Development of rapid tests that can be used in clinical settings, allowing for immediate diagnosis and treatment.
- Multiplex Testing: Tests that can simultaneously detect multiple STIs, including gonorrhea and chlamydia, from a single sample.
Genomic Studies
- Whole Genome Sequencing: This technique helps to understand the epidemiology of N. gonorrhoeae, including patterns of antibiotic resistance and transmission dynamics.
Vaccination Efforts
- Although there is currently no vaccine for gonorrhea, research is ongoing to identify potential vaccine candidates to prevent infection.