Introduction
-
Haemophilia is a hereditary bleeding disorder caused by deficiency of specific coagulation factors.
-
It results in prolonged or spontaneous bleeding due to defective blood clot formation.
-
The disorder primarily affects the intrinsic pathway of the coagulation cascade.
-
Haemophilia is most commonly inherited as an X-linked recessive condition.
-
Males are predominantly affected, while females usually act as carriers.
-
The two major forms are Haemophilia A (Factor VIII deficiency) and Haemophilia B (Factor IX deficiency).
-
Bleeding typically occurs into joints, muscles, and soft tissues, rather than superficial skin.
-
Hemarthrosis (joint bleeding) is the hallmark clinical feature.
-
Laboratory findings characteristically show prolonged aPTT with normal PT and platelet count.
-
With advances in factor replacement therapy and gene therapy, haemophilia is now a manageable chronic disorder.
Types of Haemophilia
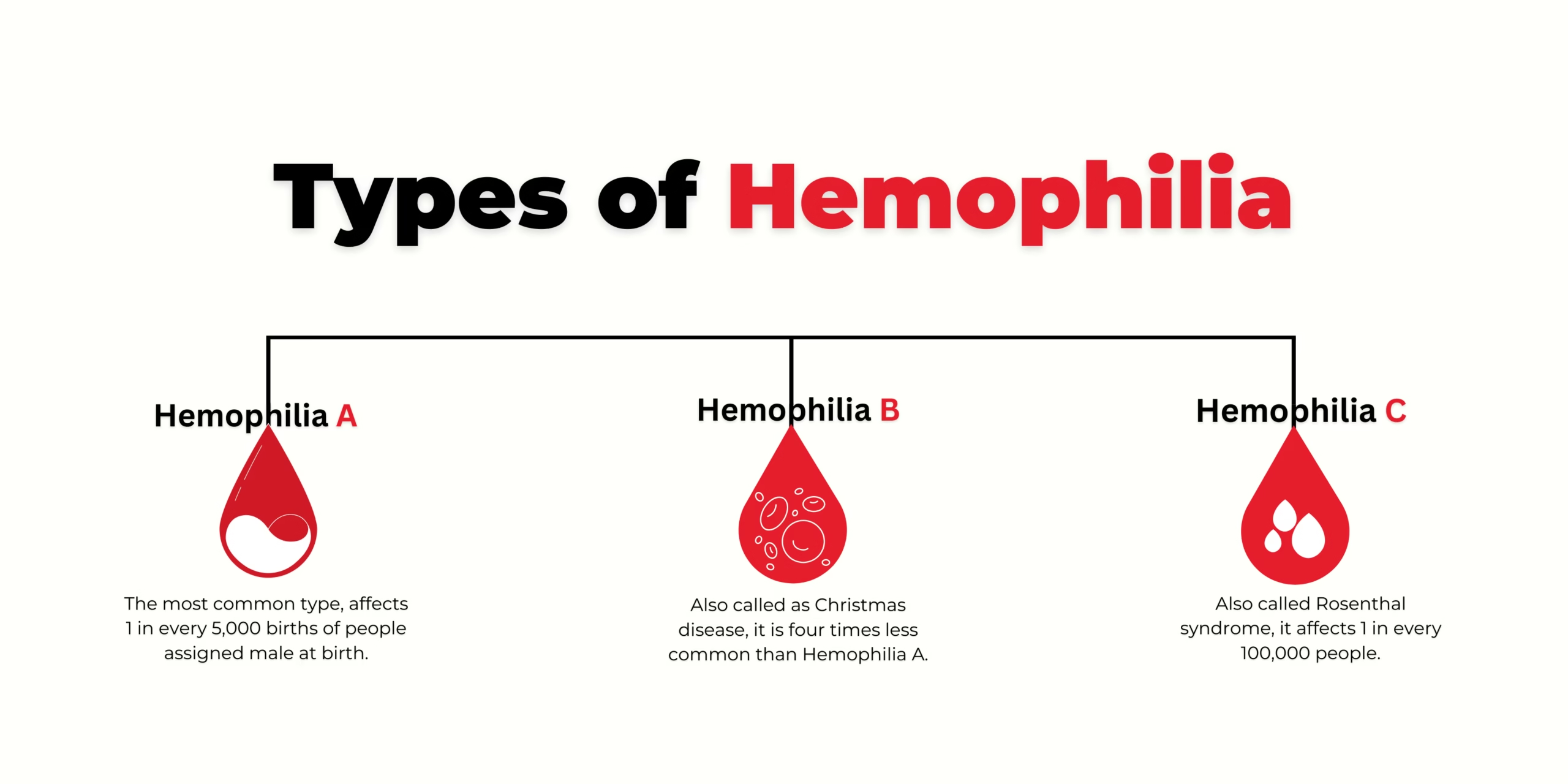 Haemophilia is classified based on the specific coagulation factor deficiency. The major types are described below:
Haemophilia is classified based on the specific coagulation factor deficiency. The major types are described below:
1. Haemophilia A
-
Also called Classic Haemophilia
-
Caused by Factor VIII deficiency
-
Accounts for 80–85% of cases
-
Inheritance: X-linked recessive
-
Common features:
-
Severe hemarthrosis
-
Muscle hematomas
-
Prolonged bleeding after surgery
-
-
Laboratory findings:
-
↑ aPTT
-
Normal PT and bleeding time
-
2. Haemophilia B
-
Also known as Christmas Disease
-
Caused by Factor IX deficiency
-
Accounts for 15–20% of cases
-
Inheritance: X-linked recessive
-
Clinical presentation is indistinguishable from Haemophilia A
-
Diagnosed by Factor IX assay
3. Haemophilia C
-
Caused by Factor XI deficiency
-
Very rare
-
Inheritance: Autosomal recessive
-
Affects both males and females
-
Usually presents with:
-
Mild bleeding
-
Post-operative bleeding
-
-
Less common hemarthrosis
4. Acquired Haemophilia
-
Caused by autoantibodies against clotting factors (commonly Factor VIII)
-
Seen in:
-
Elderly individuals
-
Postpartum women
-
Autoimmune disorders
-
-
Not inherited
-
Presents with:
-
Sudden severe bleeding
-
No family history
-
Table
| Type | Deficient Factor | Inheritance | Frequency | Severity |
|---|---|---|---|---|
| Haemophilia A | Factor VIII | X-linked | Most common | Mild–Severe |
| Haemophilia B | Factor IX | X-linked | Common | Mild–Severe |
| Haemophilia C | Factor XI | Autosomal | Rare | Mild |
| Acquired | Factor VIII (inhibitors) | Non-genetic | Rare | Severe |
Genetic Basis
Haemophilia is primarily a genetic disorder of blood coagulation caused by mutations affecting genes responsible for clotting factor synthesis.
1. Mode of Inheritance
-
Haemophilia A and B follow an X-linked recessive inheritance
-
Predominantly affects males
-
Females are usually asymptomatic carriers
2. Gene Involvement
| Type | Gene Affected | Chromosomal Location |
|---|---|---|
| Haemophilia A | F8 gene | X chromosome (Xq28) |
| Haemophilia B | F9 gene | X chromosome (Xq27) |
-
These genes encode Factor VIII and Factor IX, respectively
-
Mutations lead to partial or complete absence of functional clotting factors
3. Types of Genetic Mutations
-
Point mutations
-
Insertions or deletions
-
Inversions (common in severe Haemophilia A)
-
Nonsense mutations leading to truncated proteins
Severity of haemophilia correlates with the type and extent of mutation.
4. Carrier State in Females
-
Females have two X chromosomes
-
One normal gene compensates for the defective one
-
Some carriers may show:
-
Mild bleeding
-
Reduced factor levels (due to lyonization / X-chromosome inactivation)
-
5. Inheritance Pattern
-
Carrier mother × normal father →
-
50% sons affected
-
50% daughters carriers
-
-
Affected father × normal mother →
-
All daughters carriers
-
Sons unaffected
-
6. De Novo Mutations
-
~30% of cases occur due to new (sporadic) mutations
-
No previous family history
-
Important in genetic counseling
7. Genetic Basis of Haemophilia C
-
Caused by Factor XI gene mutations
-
Autosomal recessive inheritance
-
Affects both males and females
-
More common in certain ethnic populations
8. Clinical Significance
-
Helps in:
-
Prenatal diagnosis
-
Carrier detection
-
Genetic counseling
-
Personalized therapy and prognosis
-
Pathophysiology
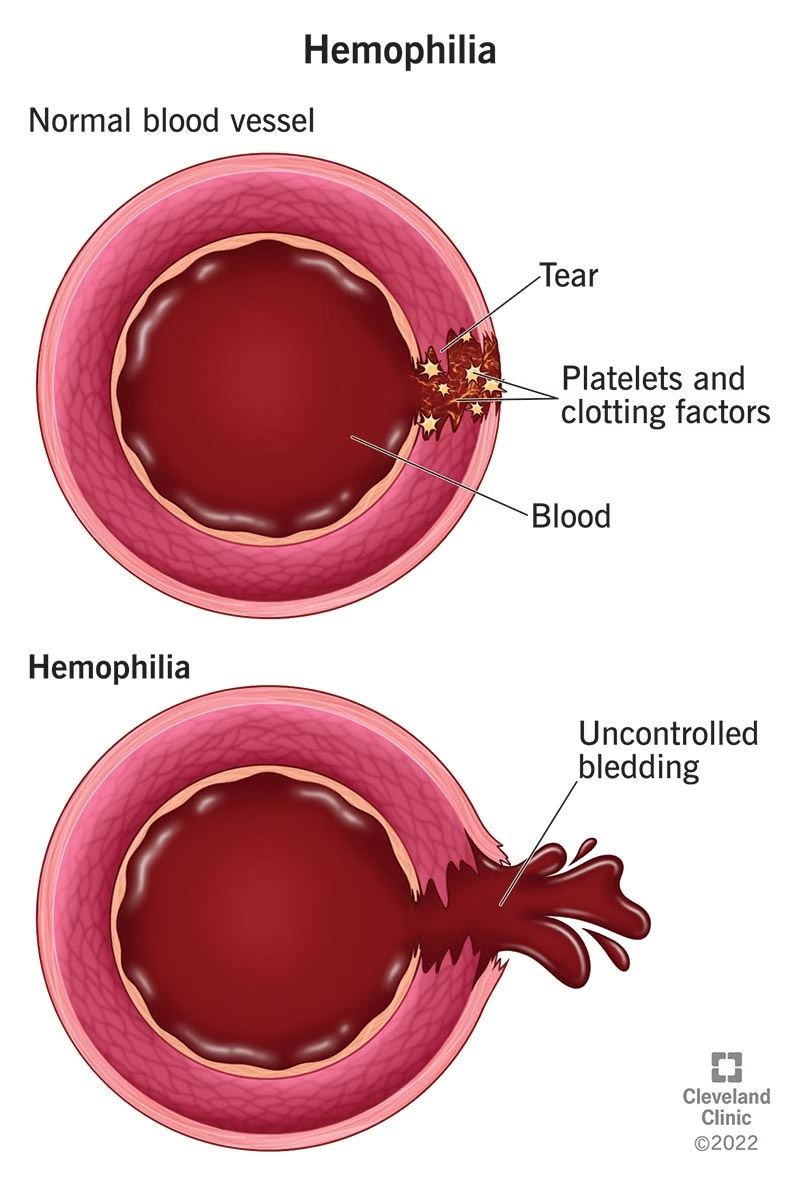
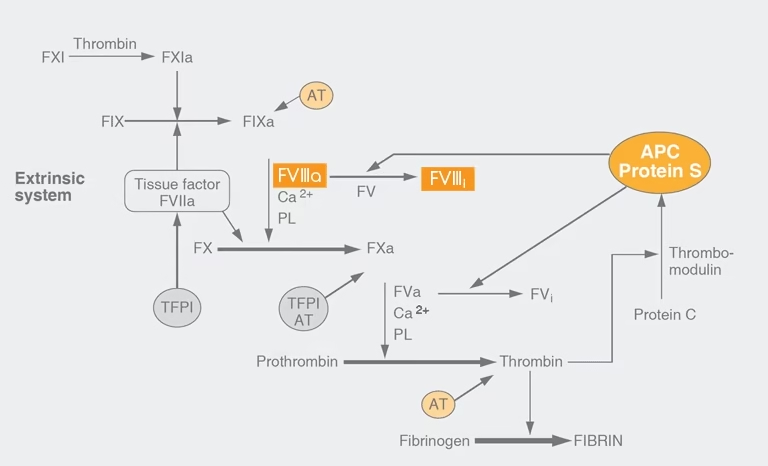 Haemophilia is a coagulation disorder resulting from a defect in the intrinsic pathway of the coagulation cascade, leading to impaired fibrin clot formation and persistent bleeding.
Haemophilia is a coagulation disorder resulting from a defect in the intrinsic pathway of the coagulation cascade, leading to impaired fibrin clot formation and persistent bleeding.
1. Normal Coagulation
-
Hemostasis occurs in three stages:
-
Vascular constriction
-
Platelet plug formation
-
Coagulation cascade → fibrin clot
-
-
The intrinsic pathway involves Factors VIII, IX, XI, and XII
-
Factor VIII acts as a cofactor for Factor IXa in activating Factor X
2. Primary Defect in Haemophilia
| Type | Defective Factor | Pathophysiological Effect |
|---|---|---|
| Haemophilia A | Factor VIII | Failure of intrinsic pathway |
| Haemophilia B | Factor IX | Inadequate Factor X activation |
-
Reduced or absent factor activity leads to:
-
Poor conversion of prothrombin → thrombin
-
Reduced fibrinogen → fibrin
-
Weak, unstable clot formation
-
3. Effect on Hemostasis
-
Platelet plug forms normally
-
Fibrin stabilization is defective
-
Clot breaks down easily → recurrent bleeding
4. Site-Specific Bleeding
-
Joints (hemarthrosis):
-
Repeated bleeding → synovial inflammation
-
Cartilage destruction → haemophilic arthropathy
-
-
Muscles:
-
Hematoma formation
-
Compartment syndrome in severe cases
-
-
Soft tissues & CNS:
-
Life-threatening hemorrhage
-
5. Severity Correlation
-
Severity depends on residual clotting factor level
-
<1% activity → spontaneous bleeding
-
1–5% → bleeding after minor trauma
-
5% → bleeding after surgery/major trauma
6. Development of Inhibitors
-
Some patients develop alloantibodies against infused clotting factors
-
Neutralize therapeutic factor VIII or IX
-
Causes treatment resistance and severe bleeding
7. Acquired Haemophilia
-
Autoantibodies against Factor VIII
-
Sudden onset bleeding
-
No family history
Clinical Features
1. General Bleeding Manifestations
-
Prolonged bleeding after:
-
Minor cuts
-
Tooth extraction
-
Surgery or trauma
-
-
Excessive bleeding after injections or vaccinations
-
Delayed bleeding (bleeding may restart hours after injury)
2. Hemarthrosis
-
Most commonly affected joints:
-
Knee
-
Ankle
-
Elbow
-
-
Clinical signs:
-
Pain and swelling
-
Warmth and restricted movement
-
-
Recurrent episodes lead to:
-
Synovial inflammation
-
Cartilage destruction
-
Haemophilic arthropathy
-
3. Muscle Bleeding
-
Deep muscle hematomas (thigh, calf, iliopsoas)
-
Painful swelling and stiffness
-
Can cause:
-
Nerve compression
-
Compartment syndrome
-
Functional disability
-
4. Skin and Mucosal Bleeding
-
Easy bruising (ecchymosis)
-
Subcutaneous hematomas
-
Gum bleeding
-
Epistaxis (nosebleeds)
5. Internal and Life-Threatening Bleeding
-
Intracranial hemorrhage (most serious complication)
-
Gastrointestinal bleeding
-
Retroperitoneal hemorrhage
-
Hematuria (blood in urine)
6. Bleeding in Children
-
Excessive bleeding after circumcision
-
Large bruises during crawling or walking
-
Joint swelling in toddlers
-
Delayed diagnosis in mild cases
7. Severity-Based Clinical Presentation
| Severity | Factor Level | Clinical Features |
|---|---|---|
| Severe | < 1% | Spontaneous bleeding, frequent hemarthrosis |
| Moderate | 1–5% | Bleeding after minor trauma |
| Mild | > 5% | Bleeding after surgery or major trauma |
Laboratory Diagnosis
1. Screening Coagulation Tests
These tests help suspect haemophilia:
| Test | Finding in Haemophilia | Explanation |
|---|---|---|
| Bleeding Time | Normal | Platelet function intact |
| Platelet Count | Normal | No platelet deficiency |
| Prothrombin Time (PT) | Normal | Extrinsic pathway normal |
| Activated Partial Thromboplastin Time (aPTT) | Prolonged | Intrinsic pathway defect |
feature: Isolated prolongation of aPTT
2. Mixing Study
-
Patient plasma mixed with normal plasma (1:1)
-
Correction of aPTT → Factor deficiency (Haemophilia A/B)
-
No correction → Presence of inhibitors (acquired haemophilia)
3. Specific Factor Assays
| Disorder | Test |
|---|---|
| Haemophilia A | ↓ Factor VIII level |
| Haemophilia B | ↓ Factor IX level |
| Haemophilia C | ↓ Factor XI level |
-
Determines type and severity
-
Factor activity expressed as percentage of normal
4. Severity Assessment
| Factor Level | Severity |
|---|---|
| < 1% | Severe |
| 1–5% | Moderate |
| > 5% | Mild |
5. Inhibitor Assay
-
Performed in patients:
-
Not responding to therapy
-
With recurrent bleeding despite replacement
-
-
Bethesda assay used to quantify inhibitors
6. Additional Investigations
-
Complete blood count:
-
May show anemia due to blood loss
-
-
Liver function tests:
-
To rule out liver disease
-
-
Von Willebrand factor assay:
-
To exclude von Willebrand disease
-
7. Genetic Testing
-
Identification of F8 or F9 gene mutations
-
Used for:
-
Carrier detection
-
Prenatal diagnosis
-
Family screening
-
8. Diagnostic Flow
-
Prolonged aPTT
-
Normal PT & bleeding time
-
Mixing study → correction
-
Factor assay → definitive diagnosis
MCQs
1. Haemophilia is best described as:
A. Platelet disorder
B. Vascular disorder
C. Coagulation factor deficiency
D. Autoimmune disorder
Answer: C
2. The most common type of haemophilia is:
A. Haemophilia B
B. Haemophilia C
C. Acquired haemophilia
D. Haemophilia A
Answer: D
3. Haemophilia A is due to deficiency of:
A. Factor VII
B. Factor VIII
C. Factor IX
D. Factor XI
Answer: B
4. Christmas disease refers to:
A. Haemophilia A
B. Haemophilia B
C. Haemophilia C
D. Von Willebrand disease
Answer: B
5. Haemophilia B is caused by deficiency of:
A. Factor VIII
B. Factor IX
C. Factor X
D. Factor XI
Answer: B
6. Mode of inheritance of Haemophilia A is:
A. Autosomal dominant
B. Autosomal recessive
C. X-linked recessive
D. X-linked dominant
Answer: C
7. Which sex is most commonly affected by haemophilia?
A. Females
B. Males
C. Both equally
D. Only newborns
Answer: B
8. Females with one defective haemophilia gene are usually:
A. Severely affected
B. Symptomatic
C. Carriers
D. Lethal
Answer: C
9. Haemophilia mainly affects which pathway of coagulation?
A. Extrinsic
B. Common
C. Intrinsic
D. Fibrinolytic
Answer: C
10. Hallmark clinical feature of haemophilia is:
A. Petechiae
B. Hemarthrosis
C. Purpura
D. Telangiectasia
Answer: B
11. Most commonly affected joint in haemophilia is:
A. Shoulder
B. Hip
C. Knee
D. Wrist
Answer: C
12. Bleeding time in haemophilia is usually:
A. Increased
B. Decreased
C. Normal
D. Variable
Answer: C
13. Platelet count in haemophilia is:
A. Decreased
B. Increased
C. Normal
D. Absent
Answer: C
14. Prothrombin time (PT) in haemophilia is:
A. Prolonged
B. Shortened
C. Normal
D. Absent
Answer: C
15. aPTT in haemophilia is:
A. Normal
B. Shortened
C. Prolonged
D. Variable
Answer: C
16. Test most sensitive for screening haemophilia is:
A. PT
B. Bleeding time
C. aPTT
D. Clot retraction
Answer: C
17. Confirmatory test for haemophilia A is:
A. PT
B. aPTT
C. Factor VIII assay
D. Platelet count
Answer: C
18. Severity of haemophilia depends on:
A. Age
B. Gender
C. Factor activity level
D. Platelet count
Answer: C
19. Severe haemophilia is defined as factor level:
A. <10%
B. <5%
C. <1%
D. <20%
Answer: C
20. Mixing study shows correction of aPTT indicates:
A. Inhibitor present
B. Platelet defect
C. Factor deficiency
D. Liver disease
Answer: C
21. Failure of aPTT correction in mixing study suggests:
A. Vitamin K deficiency
B. Liver disease
C. Presence of inhibitors
D. Mild haemophilia
Answer: C
22. Test used to detect inhibitors is:
A. ELISA
B. Coombs test
C. Bethesda assay
D. Western blot
Answer: C
23. Haemophilia C is caused by deficiency of:
A. Factor VIII
B. Factor IX
C. Factor XI
D. Factor XII
Answer: C
24. Haemophilia C inheritance pattern is:
A. X-linked recessive
B. Autosomal recessive
C. Autosomal dominant
D. Mitochondrial
Answer: B
25. Haemophilia C affects:
A. Only males
B. Only females
C. Both sexes
D. Only children
Answer: C
26. Most serious complication of haemophilia is:
A. Anemia
B. Hemarthrosis
C. Intracranial hemorrhage
D. Muscle bleeding
Answer: C
27. Repeated joint bleeding leads to:
A. Osteoporosis
B. Rheumatoid arthritis
C. Haemophilic arthropathy
D. Septic arthritis
Answer: C
28. Preferred treatment for haemophilia is:
A. Blood transfusion
B. Vitamin K
C. Factor replacement therapy
D. Steroids
Answer: C
29. Drug useful in mild Haemophilia A is:
A. Warfarin
B. Aspirin
C. Desmopressin
D. Heparin
Answer: C
30. Drug contraindicated in haemophilia is:
A. Paracetamol
B. Aspirin
C. Tranexamic acid
D. Factor VIII
Answer: B
31. Gene therapy in haemophilia aims to:
A. Destroy platelets
B. Suppress immunity
C. Correct defective gene
D. Increase vitamin K
Answer: C
32. Acquired haemophilia is caused by:
A. Genetic mutation
B. Platelet defect
C. Autoantibodies against factor VIII
D. Vitamin deficiency
Answer: C
33. Acquired haemophilia commonly occurs in:
A. Children
B. Neonates
C. Elderly
D. Teenagers
Answer: C
34. Hematuria in haemophilia indicates:
A. Platelet defect
B. Renal bleeding
C. Liver disease
D. Infection
Answer: B
35. Muscle hematomas may cause:
A. Hypercalcemia
B. Nerve compression
C. Hypotension only
D. Rash
Answer: B
36. Best method to prevent haemophilia complications is:
A. Surgery
B. Genetic counseling
C. Chemotherapy
D. Radiation
Answer: B
37. Prenatal diagnosis of haemophilia is done by:
A. CBC
B. Ultrasound
C. Genetic testing
D. PT test
Answer: C
38. Which factor is a cofactor for Factor IXa?
A. Factor V
B. Factor VIII
C. Factor XI
D. Factor XII
Answer: B
39. Delayed bleeding after trauma is characteristic of:
A. Platelet disorders
B. Vascular disorders
C. Haemophilia
D. DIC
Answer: C
40. In haemophilia, platelet plug formation is:
A. Absent
B. Defective
C. Normal
D. Increased
Answer: C
41. Main reason for prolonged bleeding in haemophilia is:
A. Platelet deficiency
B. Weak fibrin clot
C. Vasodilation
D. Infection
Answer: B
42. Which factor level correlates with severity?
A. Platelet count
B. PT value
C. Factor VIII/IX activity
D. Bleeding time
Answer: C
43. Most common presenting age for severe haemophilia is:
A. Old age
B. Adolescence
C. Infancy
D. Adulthood
Answer: C
44. Preferred physical activity in haemophilia patients is:
A. Boxing
B. Football
C. Swimming
D. Weight lifting
Answer: C
45. Major cause of joint deformity in haemophilia is:
A. Infection
B. Recurrent bleeding
C. Vitamin deficiency
D. Osteoporosis
Answer: B
46. Which lab test differentiates haemophilia from VWD?
A. PT
B. aPTT
C. Bleeding time
D. Platelet count
Answer: C
47. In haemophilia, fibrin formation is:
A. Excessive
B. Normal
C. Reduced
D. Accelerated
Answer: C
48. Gene affected in Haemophilia A is located on:
A. Chromosome 1
B. Chromosome 7
C. X chromosome
D. Y chromosome
Answer: C
49. Most common cause of death in untreated haemophilia is:
A. Anemia
B. Infection
C. Intracranial bleeding
D. Renal failure
Answer: C
50. Best long-term management strategy is:
A. Symptomatic treatment
B. Prophylactic factor replacement
C. Blood transfusion only
D. Surgery
Answer: B