Introduction
- Hemolytic Disease of the Newborn (HDN) is a condition that arises when there is incompatibility between the blood of the mother and the fetus, leading to the destruction (hemolysis) of the newborn’s red blood cells.
- This condition is most often associated with Rh incompatibility but can also occur due to ABO incompatibility or other minor blood group incompatibilities.
- This hemolysis causes a buildup of bilirubin in the newborn’s bloodstream, leading to jaundice and, in severe cases, more significant health complications such as anemia, organ damage, or even death if untreated.
Signs and Symptoms
The severity and specific symptoms of HDN can vary based on the degree of hemolysis and the timing of the diagnosis and treatment. Common symptoms include:
-
Jaundice: One of the hallmark signs of HDN. The newborn’s skin and eyes turn yellow due to elevated bilirubin levels, a byproduct of red blood cell breakdown. Jaundice can develop within the first 24-48 hours after birth.
-
Anemia: Due to the destruction of red blood cells, the newborn may experience paleness, weakness, and fatigue. Severe anemia can cause lethargy, poor feeding, and difficulty breathing.
-
Hepatosplenomegaly: The liver and spleen may become enlarged as the body attempts to compensate for the red blood cell destruction. In extreme cases, this can cause abdominal swelling and discomfort.
-
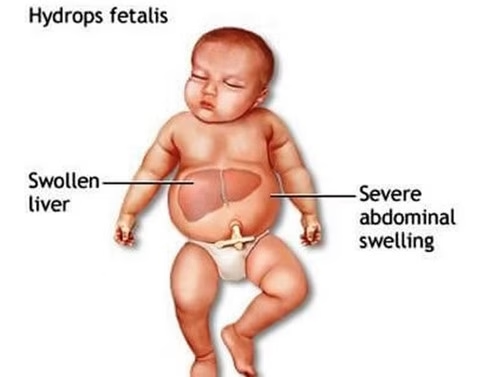
Edema (Hydrops fetalis): A severe form of HDN, hydrops fetalis is characterized by widespread swelling due to the accumulation of fluid in various parts of the body, including the abdomen, face, arms, legs, and around the lungs. This can be fatal if untreated.
-
Respiratory Distress: Severe anemia may cause respiratory distress as the baby struggles to get enough oxygen. The child may appear to be breathing fast and may require respiratory support.
-
Feeding difficulties: Babies with HDN may have poor feeding habits because of their general weakness or because they feel uncomfortable due to jaundice or anemia.
-
Abnormal Heart Rate: A rapid or irregular heartbeat can occur, often due to severe anemia, which decreases the amount of oxygen in the bloodstream.
Complications
The complications of HDN can vary in severity and may lead to permanent damage if not addressed immediately. Some potential complications include:
-
Kernicterus: A form of brain damage caused by excessive bilirubin, leading to long-term neurological deficits such as cerebral palsy, deafness, vision problems, and cognitive impairment. This occurs when bilirubin levels become dangerously high and cross the blood-brain barrier.
-
Severe Anemia: If untreated, HDN can cause very low red blood cell levels, leading to severe anemia, which might require blood transfusions.
-
Hydrops Fetalis: This is the most severe form of HDN. It results in widespread edema and organ failure in the fetus. If not treated in time, it can result in stillbirth or neonatal death.
-
Organ Failure: Due to the overproduction of red blood cells to compensate for hemolysis, the liver, spleen, and heart may become enlarged. If these organs cannot manage the excess workload, they can fail, leading to further complications.
-
Premature Birth: Severe HDN may lead to premature labor due to complications like hydrops fetalis, severe anemia, or intrauterine distress.
Pathophysiology
HDN occurs due to blood type incompatibilities between the mother and her baby. The immune system of the mother recognizes certain fetal red blood cells as foreign and mounts an immune response against them. This immune response leads to the destruction of red blood cells in the fetus or newborn. Two primary mechanisms cause this condition: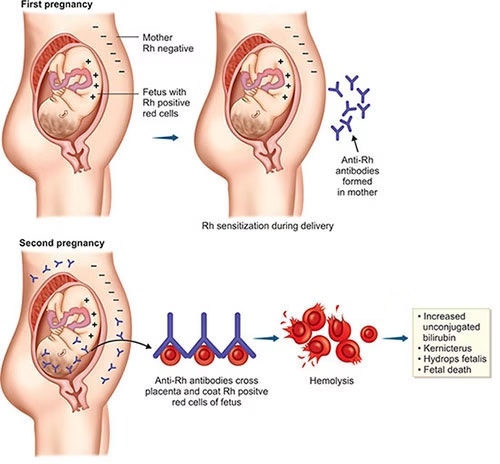
-
Rh Incompatibility:
-
Rh-negative mother, Rh-positive baby: The most common cause of HDN occurs when the mother is Rh-negative (lacks Rh antigen on her red blood cells), and the baby is Rh-positive (inherits the Rh antigen from the father).
-
During pregnancy or delivery, some of the baby’s Rh-positive blood cells may enter the mother’s bloodstream, triggering her immune system to produce anti-Rh antibodies.
-
These antibodies cross the placenta and attack the fetus’s red blood cells, causing hemolysis and leading to anemia and jaundice in the newborn.
-
The more severe the Rh incompatibility, the higher the chances of complications like hydrops fetalis or kernicterus.
-
-
ABO Incompatibility:
-
This occurs when the mother’s blood type is O, and the baby’s blood type is A, B, or AB. Type O blood naturally has antibodies (anti-A and anti-B) that can cross the placenta and attack the fetus’s red blood cells if they are of the A or B blood group.
-
This incompatibility is less severe than Rh incompatibility but still causes hemolysis and jaundice in the newborn. ABO incompatibility is much more common, affecting approximately 15-20% of pregnancies.
-
-
Other Blood Group Incompatibilities:
-
In addition to Rh and ABO, other minor blood group incompatibilities (such as Kell, Duffy, MNS antigens) can also lead to HDN but are much less common.
-
Serological Types
-
Rh Incompatibility:
-
Rh-negative mother with Rh-positive baby.
-
-
ABO Incompatibility:
-
Most common in mothers with blood type O and babies with type A, B, or AB blood.
-
-
Other Minor Blood Group Incompatibilities:
-
Involves other blood group antigens like Kell, Duffy, etc.
-
Diagnosis 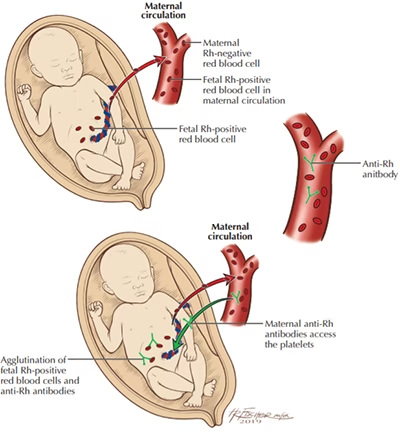
Diagnosis involves several methods, including:
-
Maternal Blood Tests:
-
Antibody screening to check for Rh antibodies.
-
Blood typing to determine the maternal and fetal blood types and check for incompatibility.
-
-
Newborn Blood Tests:
-
Bilirubin levels: To monitor jaundice and the risk of kernicterus.
-
Complete blood count (CBC): To assess anemia and red blood cell count.
-
Direct Coombs Test: To detect antibodies on the surface of red blood cells. A positive Coombs test indicates HDN.
-
-
Ultrasound:
-
To detect hydrops fetalis and the extent of organ involvement.
-
-
Amniocentesis:
-
In some cases, amniotic fluid bilirubin levels are measured to assess the severity of the condition before birth.
-
Prevention
-
Rh Immunoglobulin (RhIg):
-
RhoGAM or other Rh immunoglobulins are given to Rh-negative mothers at 28 weeks of pregnancy and after childbirth if the baby is Rh-positive. This prevents the mother’s immune system from producing anti-Rh antibodies.
-
-
Early Blood Type Screening:
-
Blood type testing at the start of pregnancy helps identify at-risk pregnancies early.
-
-
ABO Incompatibility:
-
There are no preventive measures for ABO incompatibility, but early detection and treatment can mitigate the effects of the condition.
-
After Birth Testing
After birth, babies at risk for HDN require several tests:
-
Bilirubin levels: To monitor for jaundice and prevent kernicterus.
-
Complete Blood Count (CBC): To check for anemia.
-
Direct Coombs test: To assess for antibodies on red blood cells.
Treatment
-
Phototherapy:
-
Blue light therapy is used to break down excess bilirubin and reduce jaundice.
-
-
Exchange Transfusion:
-
In severe cases, exchange transfusion may be necessary to remove antibodies and excess bilirubin from the baby’s blood and replace it with donor blood.
-
-
Blood Transfusion:
-
For severe anemia, a blood transfusion may be necessary to restore the baby’s red blood cells.
-
-
Supportive Care:
-
This includes feeding support, intravenous fluids, and sometimes oxygen therapy to support organ function.
-
Transfusion Reactions
Blood transfusion reactions can occur and include:
-
Fever
-
Chills
-
Rash
-
Back pain
-
Shortness of breath
These reactions are minimized by careful matching of the donor blood and close monitoring of the baby during the transfusion.
Epidemiology
-
Rh Incompatibility: The prevalence of Rh incompatibility varies by region, but with the widespread use of Rh immunoglobulin (RhIg), the incidence of severe Rh-related HDN has dramatically decreased.
-
ABO Incompatibility: ABO incompatibility is more common than Rh incompatibility and affects about 15-20% of pregnancies. It is usually less severe but still leads to jaundice and other complications in newborns.