
Introduction
- Inheritance of Blood Group System is determined by the presence or absence of specific antigens on the surface of red blood cells (RBCs).
- These antigens are genetically inherited from our parents.
There are more than 30 blood group systems, but the most clinically important are:
-
-
ABO blood group system
-
Rhesus (Rh) factor system
-
These systems are important in blood transfusion, organ transplantation, and pregnancy.
ABO Blood Group System
Discovery
-
Discovered by Karl Landsteiner in 1901.
-
He found that mixing blood from different individuals sometimes caused clumping (agglutination), which led to the identification of A, B, AB, and O blood groups.
Genetic Basis
-
The ABO gene is located on chromosome number 9 (9q34).
-
This gene has three alleles: IA, IB, and i.
-
IA → produces A antigen on the red cell surface.
-
IB → produces B antigen on the red cell surface.
-
i → produces no antigen.
-
Dominance Relationship:
-
IA and IB are co-dominant, meaning both can be expressed together.
-
i is recessive, meaning it will be expressed only when both alleles are i (ii).
Molecular Basis of ABO System
-
The A and B antigens are complex sugar molecules (oligosaccharides) present on the surface of RBCs.
-
The H antigen acts as the base structure.
-
The A allele codes for an enzyme that adds N-acetylgalactosamine to the H antigen.
-
The B allele codes for an enzyme that adds galactose to the H antigen.
-
The O allele produces no enzyme, so the H antigen remains unchanged.
Thus:
| Blood Type | Antigen on RBC | Added Sugar Molecule |
|---|---|---|
| A | A antigen | N-acetylgalactosamine |
| B | B antigen | Galactose |
| AB | A and B antigens | Both sugars |
| O | No antigen | None |
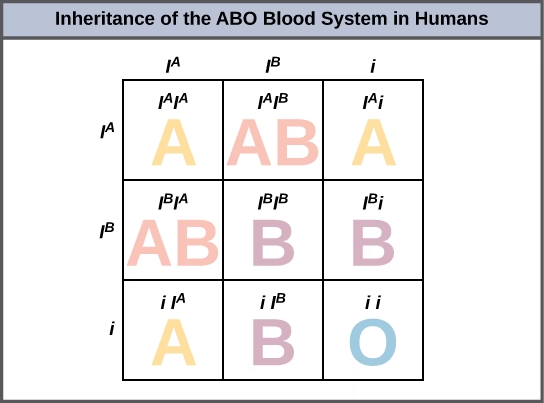
Genotypes and Phenotypes
| Blood Group | Genotype | Antigen on RBC | Antibody in Plasma |
|---|---|---|---|
| A | IAIA or IAi | A antigen | Anti-B |
| B | IBIB or IBi | B antigen | Anti-A |
| AB | IAIB | A and B antigens | None |
| O | ii | None | Anti-A and Anti-B |
Inheritance Pattern
Each individual inherits one allele from each parent.
Examples:
| Parents’ Blood Groups | Possible Blood Groups of Children |
|---|---|
| A × A | A or O |
| A × B | A, B, AB, or O |
| A × O | A or O |
| B × O | B or O |
| AB × O | A or B |
| AB × AB | A, B, or AB (no O) |
Possible Blood Types
There are four main blood types based on ABO grouping:
-
A type – has A antigen and anti-B antibodies
-
B type – has B antigen and anti-A antibodies
-
AB type – has both A and B antigens; no antibodies
-
O type – has no antigens; both anti-A and anti-B antibodies
Blood Type Compatibility
Blood Transfusion Principles
-
Antigen-antibody reaction is the key.
-
If mismatched blood is transfused, agglutination (clumping) and hemolysis occur, which can be fatal.
| Recipient’s Blood Type | Can Receive Blood From | Can Donate Blood To |
|---|---|---|
| A | A, O | A, AB |
| B | B, O | B, AB |
| AB | A, B, AB, O | AB (universal recipient) |
| O | O only | A, B, AB, O (universal donor) |
Explanation:
-
O blood group has no antigens → safe for all recipients.
-
AB blood group has no antibodies → can receive from all groups.
ABO Blood Group and Associated Health Risks
Research studies show some correlations between blood groups and diseases:
| Blood Group | Health Associations |
|---|---|
| A | Higher risk of stomach and pancreatic cancers, heart disease, and severe COVID-19 infection. |
| B | Slightly increased risk of diabetes and blood clotting disorders. |
| AB | Higher risk of cognitive impairment and thrombosis. |
| O | Lower risk of heart disease and cancer, but higher risk of peptic ulcer due to H. pylori. |
Note: These are associations, not direct causes.
Rhesus (Rh) Factor
-
The Rhesus (Rh) blood group system is one of the most important blood group systems after the ABO system.
-
It was discovered in 1940 by Karl Landsteiner and Alexander Wiener while studying Rhesus monkeys, hence the name Rhesus factor.
-
The Rh system is based on the presence or absence of a specific antigen known as the D antigen on the surface of red blood cells (RBCs).
Types of Rh Factor
-
Rh Positive (Rh⁺)
-
If D antigen is present on RBCs.
-
Example: Blood type A⁺, B⁺, AB⁺, or O⁺.
-
-
Rh Negative (Rh⁻)
-
If D antigen is absent on RBCs.
-
Example: Blood type A⁻, B⁻, AB⁻, or O⁻.
-
Approximately 85% of people are Rh positive, while 15% are Rh negative.
Genetic Basis
-
The Rh factor is controlled by a gene located on chromosome number 1.
-
The gene has two main alleles:
-
D (dominant) – produces the Rh (D) antigen.
-
d (recessive) – produces no antigen.
-
Genotypes and Phenotypes
| Genotype | Phenotype | Description |
|---|---|---|
| DD | Rh⁺ | Homozygous dominant |
| Dd | Rh⁺ | Heterozygous |
| dd | Rh⁻ | Homozygous recessive |
Inheritance:
Each person inherits one Rh gene from each parent.
Example:
-
If both parents are Rh⁺ (Dd), their child can be Rh⁺ or Rh⁻ depending on the combination of alleles.
Rhesus Factor and Blood Transfusion
Compatibility Rules:
| Recipient’s Rh Type | Can Receive Blood From | Cannot Receive Blood From |
|---|---|---|
| Rh⁺ | Rh⁺, Rh⁻ | — |
| Rh⁻ | Rh⁻ only | Rh⁺ (causes reaction) |
-
If an Rh⁻ person receives Rh⁺ blood, the immune system recognizes the D antigen as foreign and produces anti-D antibodies.
-
On second exposure, these antibodies attack and destroy the Rh⁺ red cells → causing hemolytic transfusion reaction.
Rhesus Factor and Pregnancy
Rh Incompatibility
-
Occurs when:
-
Mother → Rh⁻
-
Father → Rh⁺
-
Baby → Rh⁺ (inherits D antigen from the father)
-
During pregnancy or delivery, some fetal Rh⁺ blood may enter the mother’s bloodstream.
This causes the mother’s immune system to form anti-D antibodies (sensitization).
Effect on Future Pregnancies
-
In the first pregnancy, usually no problem occurs because antibodies form slowly.
-
In the next pregnancy with another Rh⁺ baby, the mother’s anti-D antibodies can cross the placenta and destroy the baby’s red blood cells.
This condition is called Hemolytic Disease of the Newborn (HDN) or Erythroblastosis Fetalis.
Symptoms of HDN
-
Severe anemia in the baby
-
Jaundice (yellow skin and eyes)
-
Enlarged liver and spleen
-
Swelling (edema)
-
In severe cases → stillbirth or death of the baby
Prevention
-
Anti-D Immunoglobulin (Rho(D) Injection)
-
Given to Rh⁻ mothers within 72 hours after delivery of an Rh⁺ baby.
-
Also given after miscarriage, abortion, or ectopic pregnancy.
-
It destroys any Rh⁺ fetal cells in the mother’s blood before her immune system can react.
-
-
Blood Typing During Pregnancy
-
Both parents’ blood groups are tested early in pregnancy to assess the risk.
-
-
Monitoring
-
Antibody screening and fetal health checks (ultrasound, amniotic fluid tests) are done regularly if incompatibility is suspected.
-
Clinical Importance of Rh Factor
-
Safe Blood Transfusion – prevents hemolytic reactions.
-
Safe Pregnancy – avoids HDN by giving anti-D injection.
-
Blood Donation and Organ Transplantation – ensures compatibility.
-
Forensic Medicine – helps in parentage testing and identity verification.
Genetic Basis
-
Controlled by RhD gene on chromosome 1.
-
Two main alleles:
-
D (dominant) → produces D antigen (Rh⁺)
-
d (recessive) → no antigen (Rh⁻)
-
-
Genotypes:
-
DD or Dd → Rh⁺
-
dd → Rh⁻
-
Rhesus Factor Compatibility
Blood Transfusion
| Recipient’s Rh Type | Can Receive From |
|---|---|
| Rh⁺ | Rh⁺, Rh⁻ |
| Rh⁻ | Only Rh⁻ |
If Rh⁻ person receives Rh⁺ blood → their immune system forms anti-D antibodies → causes hemolytic reaction on second exposure.
Rhesus Factor in Pregnancy (Hemolytic Disease of the Newborn)
-
Occurs when:
-
Mother = Rh⁻
-
Father = Rh⁺
-
Baby = Rh⁺
-
-
During childbirth, some Rh⁺ fetal blood may enter mother’s circulation.
-
Mother’s immune system forms anti-D antibodies.
-
In a second pregnancy with another Rh⁺ baby, these antibodies can cross the placenta and destroy fetal RBCs → causing Hemolytic Disease of the Newborn (HDN) or Erythroblastosis fetalis.
Symptoms in baby:
-
Jaundice
-
Anemia
-
Enlarged liver and spleen
-
In severe cases, stillbirth
Prevention:
-
Give anti-D immunoglobulin (Rho(D) injection) to Rh⁻ mothers within 72 hours after delivery of an Rh⁺ baby.
-
This prevents antibody formation.