
Common bacteriology Laboratory Contaminants
- In bacteriology labs, it is crucial to differentiate between true pathogens and common contaminants.
- Contaminants are microorganisms that are not the cause of disease but can be introduced into specimens unintentionally.
- Below are more detailed descriptions of common bacterial contaminants:
Skin Flora Contaminants
These bacteria are part of the normal human skin flora and are often introduced during specimen collection, particularly blood cultures or skin swabs.
-
- Staphylococcus epidermidis:
- Characteristics: Coagulase-negative, gram-positive cocci in clusters.
- Clinical Significance: While it is typically non-pathogenic, S. epidermidis can cause infections in immunocompromised patients or those with indwelling devices.
- Laboratory Diagnosis: Catalase positive, coagulase negative, grows on blood agar.
- Cutibacterium acnes (formerly Propionibacterium acnes):
- Characteristics: Gram-positive, anaerobic, or facultative anaerobic, pleomorphic rods.
- Clinical Significance: It is usually non-pathogenic but can be associated with acne, prosthetic device infections, or post-surgical wound infections.
- Laboratory Diagnosis: Catalase positive, non-motile, and produces small, white colonies on blood agar.
- Corynebacterium species:
- Characteristics: Gram-positive, non-spore-forming rods.
- Clinical Significance: Often part of normal flora, but some species like Corynebacterium diphtheriae can be pathogenic.
- Laboratory Diagnosis: Grows on selective media like Tinsdale agar for identification.
- Staphylococcus epidermidis:
Environmental Contaminants
These bacteria are frequently found in the environment, especially in soil, water, and surfaces.
-
- Bacillus species:
- Characteristics: Gram-positive, spore-forming rods.
- Clinical Significance: Bacillus cereus can cause food poisoning or wound infections, but other species like Bacillus subtilis are usually contaminants.
- Laboratory Diagnosis: Large, round, white or off-white colonies, beta-hemolytic on blood agar.
- Pseudomonas species:
- Characteristics: Gram-negative, oxidase-positive, non-fermentative rods.
- Clinical Significance: Pseudomonas aeruginosa is a pathogenic species, but non-pathogenic species (e.g., Pseudomonas putida) may occasionally contaminate cultures.
- Laboratory Diagnosis: Greenish pigment production (pyocyanin), fruity odor, oxidase positive.
- Acinetobacter species:
- Characteristics: Gram-negative coccobacilli, non-fermentative.
- Clinical Significance: Acinetobacter baumannii is pathogenic, especially in hospital settings, but other species like Acinetobacter lwoffii may be contaminants.
- Laboratory Diagnosis: Growth on MacConkey agar, non-lactose fermenter, and oxidase negative.
- Bacillus species:
Water-Associated Contaminants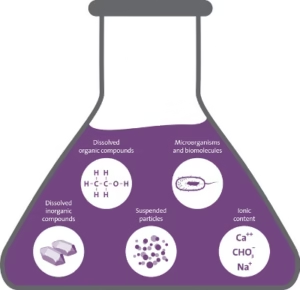
Some bacteria thrive in water and may contaminate laboratory cultures if water or equipment is disinfected.
-
- Mycobacterium gordonae:
- Characteristics: Acid-fast, slow-growing, non-pathogenic mycobacterium.
- Clinical Significance: Often found in tap water, it is non-pathogenic but can be mistaken for Mycobacterium tuberculosis.
- Laboratory Diagnosis: Slow-growing, acid-fast on Ziehl-Neelsen staining, non-chromogenic.
- Stenotrophomonas maltophilia:
- Characteristics: Gram-negative, oxidase-negative, non-fermentative rod.
- Clinical Significance: Can cause opportunistic infections, especially in immunocompromised patients, but often a contaminant in laboratory cultures.
- Laboratory Diagnosis: Lavender-green colonies on MacConkey agar, oxidase negative.
- Mycobacterium gordonae:
Laboratory-Associated Contaminants
These contaminants are typically introduced through improper sterilization of materials or accidental handling.
-
- Enterobacteriaceae species (e.g., Escherichia coli, Klebsiella):
- Characteristics: Gram-negative, facultatively anaerobic, lactose-fermenting rods.
- Clinical Significance: Some species are pathogenic (e.g., E. coli), but non-pathogenic strains are often laboratory contaminants.
- Laboratory Diagnosis: Lactose fermentation on MacConkey agar, indole positive for E. coli.
- Enterobacteriaceae species (e.g., Escherichia coli, Klebsiella):
Common Fungal Contaminants in the Laboratory
Fungal contaminants can also be introduced into cultures from environmental sources, especially air, surfaces, or improper storage of specimens.
- Yeast Contaminants
-
- Candida species:
- Characteristics: Yeast-like fungi, gram-positive, non-filamentous.
- Clinical Significance: Candida albicans is a common human pathogen, but other species, like Candida glabrata, may contaminate certain cultures (e.g., in urine or sputum samples).
- Laboratory Diagnosis: Creamy white colonies on Sabouraud agar, germ tube test positive for C. albicans.
- Candida species:
- Mould Contaminants
-
- Aspergillus species:
- Characteristics: Filamentous fungi with septate hyphae and conidia.
- Clinical Significance: Aspergillus fumigatus is pathogenic, but other species, like Aspergillus niger, can be environmental contaminants.
- Laboratory Diagnosis: Dark green or black colonies, conidial heads on microscopic examination.
- Penicillium species:
- Characteristics: Filamentous fungi, typically blue-green colonies with a characteristic “brush” appearance of conidiophores.
- Clinical Significance: Non-pathogenic but can contaminate fungal cultures.
- Laboratory Diagnosis: Blue-green colonies, characteristic brush-like conidial heads.
- Cladosporium species:
- Characteristics: Filamentous fungi with dark, branching conidiophores.
- Clinical Significance: Usually a contaminant, though certain species can cause infections in immunocompromised individuals.
- Laboratory Diagnosis: Black or olive-brown colonies, microscopically showing chains of conidia.
- Alternaria species:
- Characteristics: Dark, septate hyphae with typical alternating conidia.
- Clinical Significance: Opportunistic pathogen, but often a contaminant in laboratory cultures.
- Laboratory Diagnosis: Dark, rough-textured colonies with a “feather-like” appearance.
- Aspergillus species:
Strategies to Minimize Contamination
To minimize contamination during microbiological work, the following practices are essential:
-
- Aseptic Techniques:
- Always use sterile equipment and media.
- Practice proper hand hygiene and wear gloves when handling samples.
- Proper Specimen Collection:
- Use appropriate swabs, containers, and collection devices.
- Avoid contamination from the skin or external sources by cleaning the collection site properly.
- Environmental Controls:
- Maintain a clean laboratory environment with proper ventilation.
- Regularly disinfect surfaces and equipment.
- Ensure that water used in cultures is sterile and free from contaminants.
- Quality Control:
- Regularly test for and monitor contamination in media and reagents.
- Employ periodic checks of air quality and environmental sterilization procedures.
- Aseptic Techniques:
Distinguishing Contaminants from True Pathogens
-
- Clinical History: Carefully assessing the patient’s clinical history can help differentiate between contaminants (e.g., from normal flora) and true pathogens.
- Culture Growth Patterns: Some contaminants (like Staphylococcus epidermidis) show growth in cultures from non-infected sites. At the same time, true pathogens typically have distinctive growth characteristics or are obtained from sites of infection.
- Biochemical Testing: Detailed biochemical testing and molecular identification (e.g., PCR) can confirm whether a suspected pathogen is a contaminant.
- Repeat Cultures: If the same microorganism is isolated from multiple specimens, it is more likely to be a true pathogen. Contaminants are typically isolated from a single specimen.