
Introduction
-
Neisseria is a genus of Gram-negative, aerobic diplococci that are exclusively human pathogens.
-
Most species are commensals of the upper respiratory tract, but some are highly pathogenic.
-
The two most important pathogenic species are:
-
Neisseria gonorrhoeae – causes gonorrhoea
-
Neisseria meningitidis – causes bacterial meningitis and meningococcemia
-
-
Pathogenicity is due to pili, outer membrane proteins, IgA protease, and endotoxin (LOS).
-
N. meningitidis possesses a polysaccharide capsule, a major virulence factor.
-
Infections can range from localized mucosal disease to life-threatening systemic infections.
-
Antimicrobial resistance, especially in N. gonorrhoeae, is a growing global concern.
-
Early laboratory diagnosis, appropriate antibiotic therapy, vaccination (for meningococcal disease), and public health measures are essential for prevention and control.
General Character
Genus: Neisseria
Family
-
Neisseriaceae
Key Pathogenic Species
-
Neisseria gonorrhoeae – causes gonorrhoea
-
Neisseria meningitidis – causes bacterial meningitis and meningococcemia
Morphological Characteristics
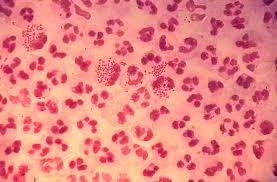
Gram Staining
-
Gram-negative bacteria
-
Appear pink on Gram stain
-
Due to:
-
Thin peptidoglycan layer
-
Presence of an outer membrane
-
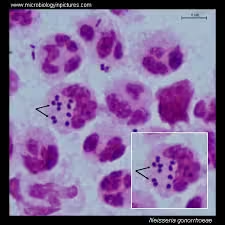
Shape and Arrangement
-
Shape: Diplococci (kidney- or coffee-bean shaped)
-
Arrangement:
-
Typically found in pairs (diplococci)
-
Occasionally seen in short chains
-
-
In clinical specimens, often found intracellularly within neutrophils (especially N. gonorrhoeae)
Oxygen Requirements
-
Strictly aerobic
-
Require enriched media and special growth conditions for optimal growth
-
Grow best at:
-
35–37°C
-
5–10% CO₂ atmosphere
-
Morphology
-
Gram reaction:
-
Gram-negative bacteria
-
Appear pink on Gram staining due to thin peptidoglycan layer and outer membrane
-
-
Shape:
-
Diplococci
-
Characteristic kidney-shaped / coffee-bean–shaped cocci
-
-
Arrangement:
-
Usually found in pairs (diplococci) with adjacent sides flattened
-
May be seen in short chains
-
Frequently observed intracellularly within polymorphonuclear leukocytes (PMNs), especially N. gonorrhoeae
-
-
Size:
-
Approximately 0.6–1.0 µm in diameter
-
-
Motility:
-
Non-motile
-
-
Spore formation:
-
Non-spore forming
-
-
Capsule:
-
Present in Neisseria meningitidis (important virulence factor)
-
Absent in Neisseria gonorrhoeae
-
-
Cell wall structure:
-
Thin peptidoglycan layer
-
Outer membrane containing lipooligosaccharide (LOS)
-
Cultural Characteristics
- Growth nature:
- Fastidious organisms
- Require enriched media for growth
- Culture media:
- Chocolate agar – supports growth of all pathogenic Neisseria
- Thayer–Martin medium (selective medium)
- Contains antibiotics (Vancomycin, Colistin, Nystatin, Trimethoprim)
- Inhibits contaminating flora and allows selective growth of Neisseria
- Atmospheric requirements:
- Aerobic
- Require 5–10% CO₂ (capnophilic) for optimal growth
- Temperature:
- Optimal growth at 35–37°C
- Colony characteristics:
- Small, round, smooth, moist, translucent colonies
- Colonies are non-pigmented and non-hemolytic
- N. gonorrhoeae colonies are delicate and may autolyse rapidly
- Growth characteristics of key species:
- Neisseria gonorrhoeae:
- More fragile, sensitive to drying and temperature changes
- Neisseria meningitidis:
- More robust, grows better on routine enriched media
- Neisseria gonorrhoeae:
- Survival:
- Poor survival outside the human host
- Sensitive to heat, drying, and disinfectants
Biochemical Reactions
Biochemical Reactions of Genus Neisseria
-
Oxidase test:
-
Positive
-
Presence of cytochrome oxidase enzyme
-
Produces purple color within 10 seconds
-
-
Catalase test:
-
Positive
-
Breaks hydrogen peroxide into water and oxygen
-
-
Carbohydrate utilization (Sugar fermentation test):
-
Acid production without gas
-
Important for species identification
-
| Species | Glucose | Maltose | Sucrose | Lactose |
|---|---|---|---|---|
| Neisseria gonorrhoeae | + | – | – | – |
| Neisseria meningitidis | + | + | – | – |
| Non-pathogenic Neisseria | Variable | Variable | Variable | Variable |
-
Nitrate reduction:
-
Negative
-
-
Indole test:
-
Negative
-
-
Urease test:
-
Negative
-
-
Polysaccharide utilization:
-
N. meningitidis utilizes maltose, helping in differentiation
-
-
Autolysis:
-
Some strains (especially N. gonorrhoeae) show autolysis on prolonged incubation
-
Pathogenicity
Virulence Factors
-
Pili (fimbriae):
-
Mediate attachment to mucosal epithelial cells
-
Show antigenic variation, helping in immune evasion
-
Essential for colonization
-
-
Outer membrane proteins (OMP):
-
Aid in adhesion and invasion
-
Prevent complement-mediated killing
-
-
Lipooligosaccharide (LOS):
-
Acts as endotoxin
-
Causes intense inflammatory response
-
Responsible for tissue damage and septic shock
-
-
IgA protease:
-
Cleaves secretory IgA
-
Facilitates survival on mucosal surfaces
-
Pathogenicity of Neisseria gonorrhoeae
-
Mode of transmission:
-
Sexual contact
-
Perinatal transmission (during childbirth)
-
-
Pathogenesis:
-
Adheres to mucosal epithelium of:
-
Urethra (male)
-
Cervix (female)
-
Rectum, pharynx, conjunctiva
-
-
Penetrates epithelial cells → induces acute suppurative inflammation
-
Survives intracellularly in neutrophils
-
-
Clinical manifestations:
-
Urethritis with purulent discharge
-
Cervicitis (often asymptomatic in females)
-
Pelvic inflammatory disease (PID)
-
Infertility and ectopic pregnancy
-
Neonatal conjunctivitis (ophthalmia neonatorum)
-
Disseminated gonococcal infection (arthritis, dermatitis, endocarditis)
-
Pathogenicity of Neisseria meningitidis
-
Mode of transmission:
-
Respiratory droplets
-
-
Capsule:
-
Major virulence factor
-
Anti-phagocytic
-
Helps survival in bloodstream
-
-
Pathogenesis:
-
Colonizes nasopharynx
-
Enters bloodstream → bacteremia
-
Crosses blood–brain barrier → meningitis
-
-
Clinical manifestations:
-
Acute bacterial meningitis
-
Meningococcemia
-
Petechial or purpuric rash
-
Septic shock
-
Waterhouse–Friderichsen syndrome (adrenal hemorrhage)
-
Laboratory Diagnosis
1. Specimen Collection
Neisseria gonorrhoeae
-
Urethral swab (male)
-
Endocervical swab (female)
-
Rectal and pharyngeal swabs
-
Conjunctival swab (neonates)
-
First-catch urine (for NAAT)
Neisseria meningitidis
-
Cerebrospinal fluid (CSF)
-
Blood (during septicemia)
-
Nasopharyngeal swab (carrier detection)
2. Direct Microscopy
-
Gram staining:
-
Gram-negative, kidney-shaped intracellular diplococci
-
Highly diagnostic in symptomatic males with gonorrhea
-
Lower sensitivity in females and asymptomatic cases
-
3. Culture
-
Media used:
-
Chocolate agar
-
Thayer–Martin selective medium
-
-
Incubation conditions:
-
35–37°C
-
5–10% CO₂ atmosphere
-
-
Colony morphology:
-
Small, smooth, moist, translucent colonies
-
N. gonorrhoeae colonies are delicate and may autolyse
-
4. Biochemical Identification
-
Oxidase test: Positive
-
Catalase test: Positive
-
Carbohydrate fermentation tests:
-
N. gonorrhoeae → Glucose only
-
N. meningitidis → Glucose + Maltose
-
5. Rapid and Molecular Methods
-
NAAT (Nucleic Acid Amplification Tests):
-
Gold standard for diagnosis of gonorrhea
-
High sensitivity and specificity
-
Useful for urine and non-invasive samples
-
-
PCR:
-
Rapid identification of meningococcal infection
-
6. Antigen Detection
-
Latex agglutination test:
-
Detects capsular antigen in CSF
-
Useful in partially treated meningitis cases
-
7. Serological Tests
-
Limited diagnostic role
-
Mainly used for epidemiological studies
8. Antibiotic Susceptibility Testing
-
Essential due to rising resistance in N. gonorrhoeae
-
Methods:
-
Disk diffusion
-
MIC determination
-
Antibiotic Resistance
1. Neisseria gonorrhoeae – Antibiotic Resistance
Drugs with Documented Resistance
-
Penicillin
-
Due to β-lactamase (penicillinase) production
-
-
Tetracyclines
-
Fluoroquinolones (e.g., ciprofloxacin)
-
Macrolides (azithromycin – increasing resistance)
-
Reduced susceptibility to third-generation cephalosporins
Mechanisms of Resistance
-
β-lactamase production
-
Plasmid-mediated (penicillin resistance)
-
-
Altered penicillin-binding proteins (PBPs)
-
Efflux pump overexpression
-
Decreases intracellular antibiotic concentration
-
-
Porin mutations
-
Reduced drug entry
-
-
Target site modification
-
Especially for fluoroquinolones and macrolides
-
Current Recommended Therapy
-
Ceftriaxone (drug of choice)
-
Often used in dual therapy to delay resistance
-
Continuous surveillance is essential
2. Neisseria meningitidis – Antibiotic Resistance
-
Generally less resistant than N. gonorrhoeae
-
Reduced susceptibility reported for:
-
Penicillin
-
Ampicillin
-
-
Resistance mechanisms:
-
Altered PBPs
-
-
Most strains remain sensitive to:
-
Ceftriaxone
-
Chloramphenicol (alternative in some settings)
-
3. Public Health Importance
-
Rapid emergence of multidrug-resistant gonococci
-
Limited treatment options available
-
Emphasis on:
-
Antibiotic stewardship
-
Surveillance programs
-
Early diagnosis and complete treatment
-
Safe sexual practices
-
Prevention
1. Vaccination
Neisseria meningitidis
-
Highly effective vaccines available
-
Types of vaccines:
-
Polysaccharide vaccines
-
Conjugate vaccines (preferred)
-
Recombinant protein vaccines (for serogroup B)
-
-
Targeted against common serogroups: A, C, Y, W, B
-
Recommended for:
-
Children and adolescents
-
Travelers to endemic areas
-
Military personnel
-
Immunocompromised individuals
-
Neisseria gonorrhoeae
-
No licensed vaccine available
-
Antigenic variation and lack of protective immunity hinder vaccine development
2. Chemoprophylaxis
Meningococcal Disease
-
Given to close contacts of confirmed cases
-
Drugs used:
-
Rifampicin
-
Ciprofloxacin
-
Ceftriaxone
-
-
Prevents secondary cases by eradicating nasopharyngeal carriage
3. Safe Sexual Practices (Gonorrhea Prevention)
-
Consistent and correct condom use
-
Limiting number of sexual partners
-
Regular screening of high-risk individuals
-
Early diagnosis and complete treatment of patients and partners
4. Infection Control Measures
-
Early case detection and isolation
-
Prompt antibiotic treatment
-
Contact tracing
-
Reporting to public health authorities
5. Health Education and Awareness
-
Public education on:
-
Sexually transmitted infections
-
Symptoms and complications
-
Importance of early treatment
-
-
School and community-based programs
6. Surveillance and Public Health Programs
-
Monitoring antimicrobial resistance patterns
-
Outbreak investigation and control
-
Strengthening laboratory diagnostic capacity
MCQs
1. Neisseria are best described as:
A. Gram-positive cocci
B. Gram-negative bacilli
C. Gram-negative diplococci
D. Gram-positive diplococci
✅ Answer: C
2. Characteristic shape of Neisseria is:
A. Lanceolate
B. Kidney bean-shaped
C. Spherical clusters
D. Filamentous
✅ Answer: B
3. Family of Neisseria is:
A. Enterobacteriaceae
B. Micrococcaceae
C. Neisseriaceae
D. Streptococcaceae
✅ Answer: C
4. Which Neisseria species causes gonorrhoea?
A. N. lactamica
B. N. sicca
C. N. meningitidis
D. N. gonorrhoeae
✅ Answer: D
5. Which Neisseria species causes meningococcemia?
A. N. gonorrhoeae
B. N. meningitidis
C. N. flavescens
D. N. subflava
✅ Answer: B
6. Gram stain of Neisseria shows:
A. Gram-positive cocci in chains
B. Gram-negative bacilli
C. Gram-negative intracellular diplococci
D. Acid-fast bacilli
✅ Answer: C
7. Neisseria are:
A. Anaerobic
B. Facultative anaerobic
C. Strictly aerobic
D. Microaerophilic
✅ Answer: C
8. Optimal temperature for Neisseria growth is:
A. 25°C
B. 30°C
C. 35–37°C
D. 42°C
✅ Answer: C
9. Neisseria requires which atmosphere for optimal growth?
A. Anaerobic
B. High oxygen
C. 5–10% CO₂
D. Nitrogen-rich
✅ Answer: C
10. Selective medium for Neisseria is:
A. MacConkey agar
B. Blood agar
C. Thayer–Martin agar
D. Lowenstein–Jensen
✅ Answer: C
11. Chocolate agar supports growth of:
A. Only N. gonorrhoeae
B. Only N. meningitidis
C. All pathogenic Neisseria
D. Only commensal Neisseria
✅ Answer: C
12. Oxidase test in Neisseria is:
A. Negative
B. Variable
C. Positive
D. Weakly positive
✅ Answer: C
13. Catalase test in Neisseria is:
A. Negative
B. Positive
C. Variable
D. Not applicable
✅ Answer: B
14. N. gonorrhoeae ferments:
A. Glucose only
B. Maltose only
C. Glucose and maltose
D. No sugars
✅ Answer: A
15. N. meningitidis ferments:
A. Glucose only
B. Maltose only
C. Glucose and maltose
D. Lactose
✅ Answer: C
16. Capsule is present in:
A. N. gonorrhoeae
B. N. meningitidis
C. Both
D. Neither
✅ Answer: B
17. Major virulence factor of N. meningitidis is:
A. Pili
B. IgA protease
C. Capsule
D. LOS
✅ Answer: C
18. Endotoxin of Neisseria is:
A. Lipopolysaccharide
B. Lipoteichoic acid
C. Lipooligosaccharide
D. Exotoxin
✅ Answer: C
19. IgA protease helps Neisseria in:
A. Capsule formation
B. Immune evasion
C. Sporulation
D. Motility
✅ Answer: B
20. Gonorrhoea is transmitted mainly by:
A. Food
B. Water
C. Sexual contact
D. Insects
✅ Answer: C
21. Meningococcal infection spreads by:
A. Sexual contact
B. Respiratory droplets
C. Fecal–oral route
D. Blood transfusion
✅ Answer: B
22. Neonatal conjunctivitis is caused by:
A. N. meningitidis
B. N. gonorrhoeae
C. Chlamydia only
D. Streptococcus
✅ Answer: B
23. Waterhouse–Friderichsen syndrome is seen in:
A. Gonorrhoea
B. Typhoid
C. Meningococcemia
D. Tuberculosis
✅ Answer: C
24. Best specimen for diagnosing gonorrhoea in males:
A. Blood
B. CSF
C. Urethral swab
D. Stool
✅ Answer: C
25. Best specimen for meningitis diagnosis:
A. Urine
B. Blood
C. CSF
D. Sputum
✅ Answer: C
26. Gold standard test for gonorrhoea diagnosis is:
A. Gram stain
B. Culture
C. NAAT
D. Serology
✅ Answer: C
27. Latex agglutination test detects:
A. Antibodies
B. Capsular antigen
C. Toxins
D. DNA
✅ Answer: B
28. Which Neisseria shows maximum antibiotic resistance?
A. N. meningitidis
B. N. gonorrhoeae
C. N. lactamica
D. N. sicca
✅ Answer: B
29. Penicillin resistance in gonococci is due to:
A. Capsule
B. Efflux pumps
C. β-lactamase
D. Spore formation
✅ Answer: C
30. Current drug of choice for gonorrhoea is:
A. Penicillin
B. Ciprofloxacin
C. Ceftriaxone
D. Azithromycin
✅ Answer: C
31. Chemoprophylaxis for meningococcal contacts includes:
A. Ampicillin
B. Rifampicin
C. Penicillin V
D. Doxycycline
✅ Answer: B
32. Vaccine is available for:
A. N. gonorrhoeae
B. N. meningitidis
C. Both
D. Neither
✅ Answer: B
33. Serogroup B vaccine is:
A. Polysaccharide
B. Toxoid
C. Recombinant protein
D. Live vaccine
✅ Answer: C
34. Neisseria are non-motile because they lack:
A. Cilia
B. Flagella
C. Pili
D. Capsule
✅ Answer: B
35. Which test differentiates N. gonorrhoeae from N. meningitidis?
A. Oxidase test
B. Catalase test
C. Sugar fermentation
D. Gram stain
✅ Answer: C
36. Intracellular diplococci are commonly seen in:
A. Blood
B. CSF
C. Neutrophils
D. Epithelial cells
✅ Answer: C
37. LOS causes:
A. Immunity
B. Inflammation and shock
C. Capsule synthesis
D. Motility
✅ Answer: B
38. Complement deficiency predisposes to:
A. Gonorrhoea
B. Meningococcal infection
C. Syphilis
D. Tuberculosis
✅ Answer: B
39. Autolysis is commonly seen in:
A. N. meningitidis
B. N. gonorrhoeae
C. N. lactamica
D. N. flavescens
✅ Answer: B
40. Best prevention of gonorrhoea is:
A. Vaccination
B. Antibiotics
C. Safe sexual practices
D. Isolation
✅ Answer: C
41. Best prevention of meningococcal disease is:
A. Antibiotics
B. Vaccination
C. Isolation
D. Nutrition
✅ Answer: B
42. Which Neisseria is a commensal?
A. N. gonorrhoeae
B. N. meningitidis
C. N. lactamica
D. All
✅ Answer: C
43. Which is NOT a virulence factor?
A. Pili
B. Capsule
C. LOS
D. Spore
✅ Answer: D
44. Gonococci survive poorly outside host due to:
A. Capsule
B. Spore formation
C. Fragile nature
D. Motility
✅ Answer: C
45. Culture failure is common in:
A. Treated patients
B. Untreated patients
C. New infections
D. Neonates
✅ Answer: A
46. NAAT is preferred because it is:
A. Cheap
B. Rapid and sensitive
C. Culture-based
D. Manual
✅ Answer: B
47. Gonorrhoea in females is often:
A. Severe
B. Fatal
C. Asymptomatic
D. Self-limiting
✅ Answer: C
48. Thayer–Martin medium contains antibiotics to:
A. Enhance Neisseria growth
B. Kill Neisseria
C. Inhibit normal flora
D. Increase pigment
✅ Answer: C
49. Which antibiotic resistance is plasmid-mediated?
A. Cephalosporin
B. Penicillin
C. Rifampicin
D. Chloramphenicol
✅ Answer: B
50. Neisseria are exclusively:
A. Environmental organisms
B. Animal pathogens
C. Human pathogens
D. Plant pathogens
✅ Answer: C