
Introduction
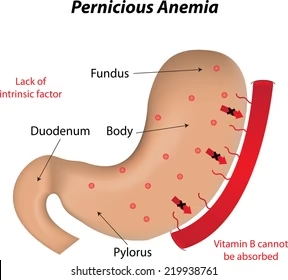
- Pernicious anaemia is a chronic, autoimmune condition resulting in vitamin B12 deficiency.
- This deficiency occurs because of the inability to absorb vitamin B12 from the gastrointestinal tract, primarily due to a lack of intrinsic factor.
- Intrinsic factor (IF) is a glycoprotein produced by the gastric parietal cells and is essential for the absorption of vitamin B12 in the terminal ileum of the small intestine.
- The lack of B12 leads to megaloblastic anaemia, a condition characterized by large, immature, and dysfunctional red blood cells.

Etiology
The underlying causes of pernicious anaemia are diverse, and the primary ones include:
-
Autoimmune Destruction of Parietal Cells:
-
The most common cause of pernicious anaemia is an autoimmune response targeting the parietal cells of the stomach. This autoimmune reaction reduces the ability of the parietal cells to produce intrinsic factor (IF), leading to vitamin B12 malabsorption.
-
The antibodies against intrinsic factor (IF) are specific and interfere with vitamin B12 binding to IF, blocking its absorption in the ileum.
-
-
Atrophic Gastritis:
-
Chronic inflammation of the stomach lining, often associated with autoimmune destruction of gastric mucosa, leads to atrophy of the gastric mucosa and reduced secretion of IF. As a result, vitamin B12 absorption is impaired.
-
-
Genetic Predisposition:
-
There is a genetic component, with a higher incidence in individuals with a family history of pernicious anaemia. Certain genetic mutations may increase susceptibility, particularly those related to immune function.
-
-
Associated Autoimmune Diseases:
-
Pernicious anaemia is commonly associated with other autoimmune disorders such as:
-
Type 1 diabetes
-
Autoimmune thyroid disease (Hashimoto’s thyroiditis)
-
Addison’s disease (adrenal insufficiency)
-
Graves’ disease
-
Celiac disease
-
-
These conditions may occur in conjunction due to the shared autoimmune pathways.
-
-
Surgical Causes:
-
Gastrectomy (removal of part or all of the stomach) or ileal resection (removal of part of the ileum) can lead to vitamin B12 deficiency since the stomach and terminal ileum are critical for absorption.
-
-
Malabsorption Syndromes:
-
Conditions like Crohn’s disease, celiac disease, or short bowel syndrome affect the intestinal absorption of B12 due to damage to the ileum or other parts of the gastrointestinal tract.
-
-
Dietary Deficiency (Rare):
-
Vitamin B12 is found mainly in animal products (meat, eggs, dairy), and strict vegans or those with malabsorption issues might develop deficiency if the intake is inadequate or absorption is impaired.
-
Epidemiology
-
Pernicious anaemia is more common in older adults, with a higher prevalence in those over the age of 60.
-
The condition is more frequently observed in Caucasians, particularly those of Northern European descent.
-
Women are affected more often than men, with a 2:1 ratio.
-
The prevalence in the general population is estimated to be about 0.1%, but it increases with age, reaching 2% in individuals over 60 years.
-
Genetic predisposition plays a role, and individuals with a family history of pernicious anaemia are at greater risk.
-
Pernicious anaemia is associated with a variety of other autoimmune disorders, including autoimmune thyroid disease, type 1 diabetes, and Addison’s disease.
-
It is also more common in people with a history of gastric surgery (e.g., gastrectomy or ileal resection).
Pathophysiology
-
Intrinsic Factor (IF) and Vitamin B12 Absorption:
-
Intrinsic factor (IF) is essential for vitamin B12 absorption in the ileum of the small intestine.
-
IF binds to vitamin B12 in the stomach, and this complex travels to the terminal ileum, where it is absorbed via a specific receptor-mediated mechanism.
-
In pernicious anaemia, the autoimmune destruction of gastric parietal cells reduces the secretion of intrinsic factor, leading to impaired absorption of vitamin B12.
-
-
Impaired Erythropoiesis:
-
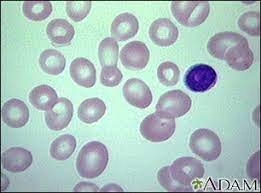
Vitamin B12 is required for the maturation of red blood cells. B12 deficiency leads to megaloblastic changes in the bone marrow, meaning the red blood cells produced are large, immature, and dysfunctional.
-
These large red blood cells are known as megaloblasts, which do not function properly and have a reduced ability to transport oxygen.
-
The body also compensates for the impaired erythropoiesis by releasing immature red blood cells into the peripheral blood.
-
-
Neurological Manifestations:
-
Vitamin B12 is essential for myelin synthesis in the nervous system. B12 deficiency causes demyelination, particularly in the posterior columns and corticospinal tracts of the spinal cord, leading to neurological symptoms such as:
-
Paresthesia (tingling in hands and feet)
-
Weakness
-
Gait disturbances
-
Cognitive impairment or dementia if untreated.
-
-
-
Hypersegmented Neutrophils:
-
One of the hallmark features in the peripheral blood of patients with pernicious anaemia is the presence of hypersegmented neutrophils. These are neutrophils with more than five nuclear segments, a classic sign of megaloblastic anaemia.
-
Laboratory Investigations
-
Complete Blood Count (CBC):
-
Macrocytic anaemia: This is characterized by an elevated mean corpuscular volume (MCV), often >100 fL, indicating the presence of large, immature red blood cells.
-
Anisocytosis: Variation in red blood cell size.
-
Low haemoglobin: Resulting from ineffective erythropoiesis.
-
Hypersegmented neutrophils: A key feature of megaloblastic anaemia.
-
-
Serum Vitamin B12:
-
A low serum B12 level is diagnostic, but it should be confirmed with additional tests, as levels can be affected by other conditions (e.g., liver disease).
-
-
Serum Homocysteine and Methylmalonic Acid:
-
Elevated homocysteine and methylmalonic acid (MMA) are specific markers of vitamin B12 deficiency. Elevated MMA is a more specific indicator of B12 deficiency than homocysteine, and both are often measured in conjunction with B12 levels.
-
-
Intrinsic Factor Antibody Test:
-
Intrinsic factor antibodies are present in approximately 70% of individuals with pernicious anaemia. A positive result confirms the autoimmune nature of the disease but does not directly correlate with the severity of the condition.
-
-
Parietal Cell Antibody Test:
-
Antibodies against parietal cells are present in 90% of individuals with pernicious anaemia but are less specific than IF antibodies.
-
-
Schilling Test (Historical):
-
The Schilling test was historically used to diagnose vitamin B12 malabsorption. It involved oral and intramuscular administration of vitamin B12 and measuring its excretion in urine. If B12 was not absorbed, it would indicate a lack of intrinsic factor.
-
-
Bone Marrow Biopsy:
-
If necessary, a bone marrow biopsy can show megaloblastic changes, with large, immature red blood cells and a decreased number of mature red blood cells.
-
-
Gastric Biopsy:
-
A gastric biopsy can reveal atrophic gastritis or damage to parietal cells, confirming the presence of autoimmune gastritis in many cases of pernicious anaemia.
-
Treatment and Management
-
Vitamin B12 Replacement:
-
Parenteral B12 (hydroxocobalamin or cyanocobalamin):
-
Initial Treatment: High-dose B12 injections, typically 1,000 mcg daily or every other day for 1–2 weeks to correct deficiency.
-
Maintenance: Once levels are normalized, B12 is usually administered intramuscularly every 2–3 months for life.
-
-
Oral Vitamin B12: In some patients with mild deficiency, high-dose oral B12 supplements (e.g., 1,000–2,000 mcg daily) may be used, especially if intrinsic factor production is sufficient.
-
-
Folic Acid:
-
Folate supplementation is sometimes required, especially if there is a concurrent folate deficiency, but it should be used cautiously as it can mask the neurological symptoms of B12 deficiency.
-
-
Monitoring:
-
Regular monitoring of vitamin B12 levels and complete blood counts (CBC) to track the effectiveness of therapy.
-
Neurological symptoms may improve slowly or not at all, so patients should be monitored for long-term complications.
-
-
Treating Underlying Conditions:
-
Manage any associated autoimmune disorders that may be contributing to the condition (e.g., autoimmune thyroiditis or type 1 diabetes).
-
-
Patient Education:
-
Patients should be informed that treatment is lifelong, and regular follow-up is required to ensure that B12 levels remain normal and that symptoms are managed.
-
Management (Long-Term)
-
Lifelong Vitamin B12 Therapy:
-
Parenteral or oral B12 therapy is typically needed for life, as the underlying autoimmune disorder will persist.
-
-
Monitoring:
-
Regular follow-up to ensure that B12 levels are maintained and that there are no signs of deterioration.
-
Neurological assessment should be part of the long-term management plan, as neuropathy or dementia may not fully reverse.
-
-
Screening for Complications:
-
Increased gastric cancer risk due to chronic atrophic gastritis should be considered. Regular screening may be appropriate, especially in older patients.
-
Be vigilant for other autoimmune diseases that may require management alongside pernicious anaemia.
-
-
Dietary Management:
-
Encourage dietary intake of vitamin B12, particularly for vegans or those with gastrointestinal diseases that affect absorption.
-
Supplementation should be encouraged for those at risk of deficiency.
-