Introduction
- Prevention of viral diseases has long been a significant threat to global health, causing illnesses from mild colds to life-threatening infections.

- Preventing these diseases is crucial for reducing their spread and impact on individuals, communities, and healthcare systems.
- Viruses, due to their ability to mutate and adapt, can spread quickly and efficiently, making prevention strategies even more important.
- Prevention involves various methods, ranging from vaccination to hygiene practices, antiviral medications, vector control, and public health education.
- These strategies aim not only to stop the transmission of viruses but also to mitigate their effects and protect those who are most vulnerable.
- By understanding the modes of transmission and adopting effective preventive measures, we can reduce the burden of viral diseases and ultimately improve global health outcomes.
Vaccination
Vaccination is one of the most effective methods to prevent viral infections. Vaccines stimulate the body’s immune system to recognize and fight specific viruses, offering long-term immunity. Here’s a detailed elaboration on how vaccines work and their role in viral disease prevention: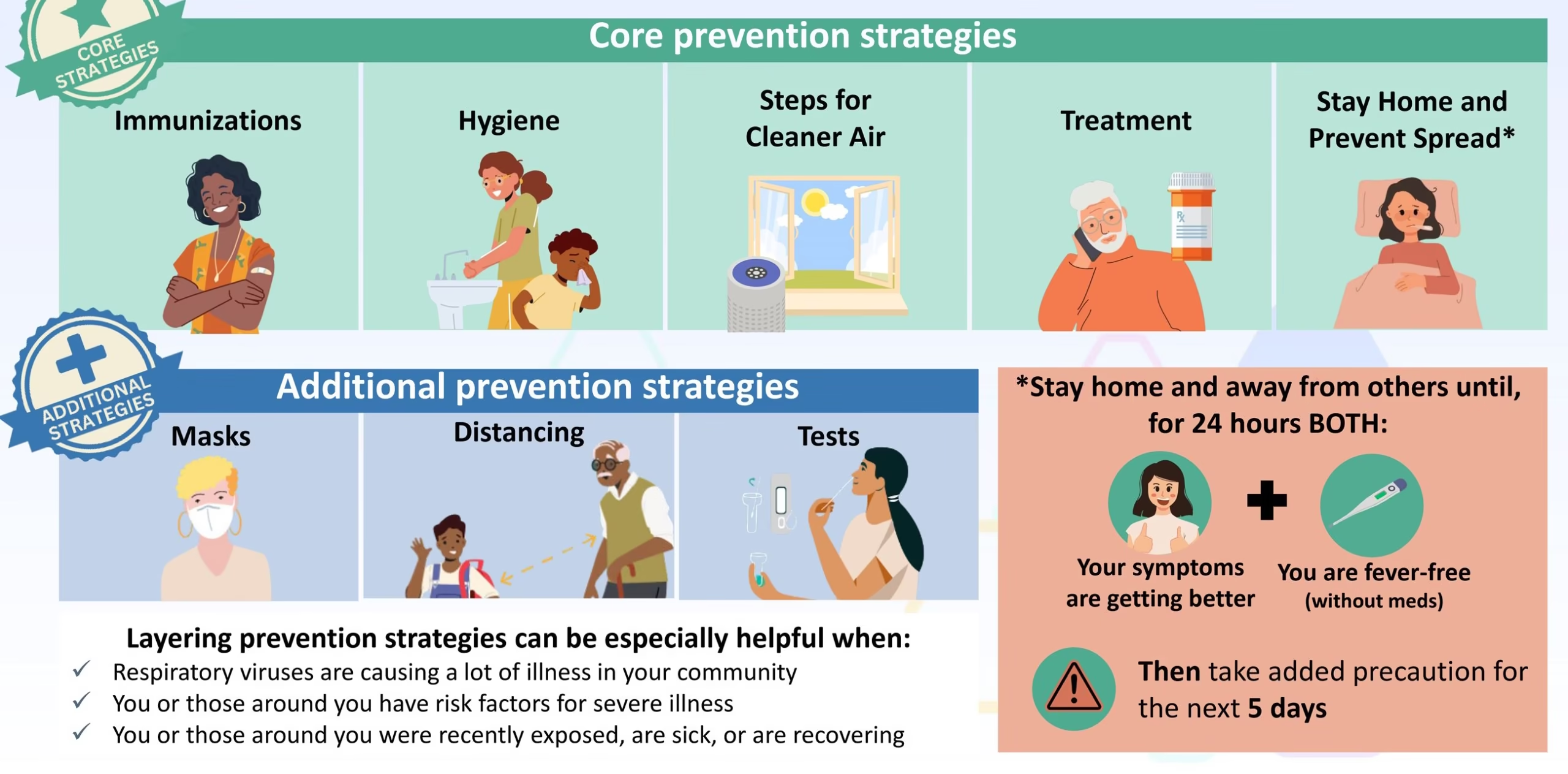
-
Mechanism: Vaccines contain weakened or inactivated parts of a virus (antigens), or sometimes a piece of its genetic material, which primes the immune system to produce antibodies. In the event of actual infection, the immune system can quickly recognize and fight the virus.
-
Common Vaccines for Viral Diseases:
- MMR (Measles, Mumps, Rubella): Provides protection against these three viral infections, which can cause serious complications like encephalitis, deafness, and birth defects. The MMR vaccine is typically administered in early childhood.
- Hepatitis B Vaccine: Prevents Hepatitis B infection, a liver disease that can lead to chronic liver disease, cirrhosis, or liver cancer. The vaccine is given in a series of doses starting at birth.
- Influenza Vaccine: Updated annually to protect against the most common circulating strains of the flu virus. The flu vaccine is crucial for high-risk populations, such as the elderly, children, and immunocompromised individuals.
- HPV Vaccine: Prevents infection by the human papillomavirus (HPV), which is linked to several cancers, including cervical cancer. This vaccine is typically given to adolescents before they become sexually active.
- Polio Vaccine: Protects against polio, a paralyzing disease nearly eradicated worldwide through extensive vaccination programs.
-
Herd Immunity: Widespread vaccination in a population helps protect those who cannot be vaccinated (e.g., infants and immunocompromised individuals) because the virus cannot spread easily when most of the population is immune.
Antiviral Medications
While vaccines help prevent infection, antiviral medications are crucial for treating existing viral infections, especially in cases where no vaccine exists or the virus has already been contracted. These medications can reduce the severity of infections, prevent complications, or even cure some viral diseases.
-
Mechanism of Action: Antiviral drugs work by inhibiting the replication of viruses. They may block the virus from entering cells, prevent the virus from using the host cell machinery to replicate or inhibit the maturation and release of viral particles.
-
Examples of Antiviral Drugs:
- HIV: Antiretroviral therapy (ART) helps reduce the viral load in HIV patients, preventing progression to AIDS and lowering the risk of transmission to others.
- Hepatitis C: Direct-acting antivirals (DAAs) have revolutionized the treatment of Hepatitis C, providing a cure for many patients.
- Influenza: Drugs like Oseltamivir (Tamiflu) and Zanamivir (Relenza) can reduce the severity and duration of flu symptoms, especially when taken early during the illness.
- Herpes: Acyclovir, Valacyclovir, and Famciclovir are antiviral drugs that treat Herpes simplex virus (HSV) infections, reducing the severity and frequency of outbreaks.
-
Prevention of Resistance: Just like antibiotics, the misuse or overuse of antiviral medications can lead to resistance. Proper diagnosis, treatment adherence, and stewardship are essential to avoid resistance.
Hygiene and Sanitation Practices
Proper hygiene and sanitation practices are fundamental in preventing the spread of viruses, especially those transmitted through direct contact or contaminated surfaces. Here’s a detailed look at the key hygiene practices that help prevent viral diseases:
- Hand Hygiene:
- Handwashing with soap and water is the most effective way to remove viruses from the hands. Soap breaks down the virus’s lipid coating, while water rinses it away.
- When soap and water are unavailable, alcohol-based hand sanitizers (with at least 60% alcohol) are a good alternative to kill most viruses, including rhinovirus (common cold) and influenza.
- Surface Cleaning and Disinfection:
- Viruses such as Norovirus and Rhinovirus can survive on surfaces for hours to days. Regularly cleaning high-touch surfaces such as doorknobs, light switches, and phones with bleach or hydrogen peroxide disinfectants can help kill the virus and prevent transmission.
- Respiratory Hygiene:
- Viruses like COVID-19, Influenza, and the common cold are spread through respiratory droplets. Teaching people to cover their mouth and nose with a tissue or elbow when coughing or sneezing helps prevent the release of infectious droplets into the air and onto surfaces.
- Proper disposal of tissues and wearing masks during an outbreak or when sick can also reduce the spread of viruses.
- Food Safety:
- Viral infections like Hepatitis A and Norovirus are often spread through contaminated food. Proper food handling, cooking, storage, and regular handwashing before preparing or consuming food, reduce the risk of transmission.
Vector Control
Viral infections transmitted by vectors (insects like mosquitoes, ticks, and fleas) require specific control measures to limit the spread of viruses. These measures are especially crucial for diseases such as Dengue, Zika, and Malaria. Here’s how vector control works:
-
Mosquito Control:
- Eliminating Breeding Sites: Mosquitoes lay their eggs in stagnant water. Eliminating standing water in containers, tires, flower pots, or puddles prevents mosquito breeding.
- Use of Insecticides: Insecticides and larvicides help kill adult mosquitoes or prevent larvae from developing into adults in water bodies.
- Personal Protection: Using mosquito nets treated with insecticides, wearing long-sleeved clothing, and applying DEET-containing repellents on exposed skin can prevent mosquito bites and the transmission of viruses.
- Biological Control: Introducing natural predators like fish that eat mosquito larvae or using genetically modified mosquitoes to reduce mosquito populations are emerging methods.
-
Tick and Flea Control:
- Personal Protective Measures: When entering tick-prone areas, wear long sleeves and pants, and tuck pants into socks to prevent ticks from attaching to skin.
- Tick Repellents: Apply repellents containing permethrin or DEET to reduce the chances of tick attachment.
- Control in Pets: Pets should be treated with tick and flea preventatives to reduce the risk of transmission of Tick-borne Encephalitis or Lyme disease.
Safe Practices for Blood and Bodily Fluids
Bloodborne viral infections like HIV, Hepatitis B, and Hepatitis C require special precautions to prevent transmission. Here’s how safe practices help reduce viral transmission:
-
Safe Injection Practices:
- In healthcare settings, using sterile needles and syringes for each patient prevents transmission of viruses like HIV and Hepatitis B.
- For individuals who inject drugs, harm reduction programs such as needle exchange services can help reduce the risk of infection.
-
Safe Sexual Practices:
- Condoms (male and female) are one of the most effective ways to prevent the transmission of HIV, HPV, Herpes, and Hepatitis B. They act as a barrier to prevent the exchange of bodily fluids.
- Regular screening for sexually transmitted infections (STIs) and reducing the number of sexual partners can also lower the risk of contracting or spreading viral infections.
-
Blood Donation and Screening:
- Donated blood is rigorously tested for HIV, Hepatitis B, and Hepatitis C to ensure that it is free from viral infections. This minimizes the risk of viral transmission through blood transfusions.
Quarantine and Isolation
For highly contagious viral diseases, isolation and quarantine are essential to prevent the spread of the virus to others.
-
Isolation: Individuals infected with a contagious virus (such as COVID-19 or Measles) should be isolated from healthy individuals to prevent person-to-person transmission. Isolation can occur in a hospital or at home, depending on the severity of the illness.
-
Quarantine: Individuals exposed to a viral agent (but not showing symptoms) may be placed under quarantine. This precautionary measure prevents potential spread if the virus manifests later. For example, individuals exposed to COVID-19 may be quarantined for a specific period.
-
Travel Restrictions: In cases of emerging viral outbreaks (e.g., Ebola, Zika), travel restrictions or advisories may be issued to reduce the risk of cross-border transmission.
Education and Public Awareness
Education and awareness campaigns are essential for preventing viral diseases. When individuals understand the modes of transmission, they are more likely to adopt preventive measures.
-
Public Health Campaigns: Governments and health organizations can run campaigns emphasising the importance of vaccination, handwashing, and proper hygiene. These campaigns often target specific high-risk groups or geographical regions.
-
Community Engagement: Community-based approaches help educate local populations about viral disease risks and preventive measures. In areas where vector-borne diseases like Dengue or Malaria are common, educating people on mosquito control and using insect repellents can significantly reduce transmission.
Environmental and Ecological Measures
Environmental and ecological factors can influence the spread of viral diseases, especially vector-borne diseases. Preventing or minimizing these risks involves managing both human behaviour and environmental conditions.
-
Climate and Geography: Climate change can expand the range of many viruses, particularly vector-borne ones. Monitoring environmental factors like temperature, rainfall, and humidity can help predict and prevent outbreaks of Dengue or Malaria.
-
Wildlife Management: Many zoonotic viruses (e.g., Ebola, Zika) can spread from animals to humans. Managing wildlife populations, avoiding close contact with animals, and promoting safe handling of animals can help reduce the transmission of such viruses.