Radioimmunoassay
- Radioimmunoassay (RIA) is a highly sensitive and specific laboratory technique that measures minute amounts of antigens or substances (such as hormones, drugs, and proteins) in biological samples.
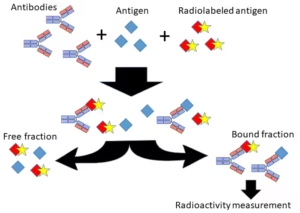
- RIA works on competitive binding between a radioactively labeled antigen and an unlabeled (unknown) antigen for a fixed number of antibody binding sites.
- The concentration of the unknown antigen can be determined by measuring the radioactivity of the antibody-antigen complex.
Principle of RIA
RIA is based on competitive inhibition, where the amount of radioactive labeled antigen (antigen with a radioisotope) in a sample competes with the non-radioactive or unlabeled antigen (from the sample) for binding to a fixed number of antibody sites. The radiolabeled antigen and the unlabeled antigen cannot both bind to the antibody at the same time.
- Radioactive Labeling: The radioactive isotope is typically iodine-125 (125I) or tritium (3H), which emits detectable radiation. The labeled antigen is usually the same as the measured antigen, except it is chemically modified to include a radioactive element.
- Antibody-Antigen Binding: Antibodies are proteins that recognize and bind to specific antigens. In RIA, the antibody is prepared to be highly specific for the antigen of interest.
- Separation: The unbound antigens are separated from the bound antigen-antibody complexes after forming the antigen-antibody complex. The radioactivity of the bound fraction is measured, which gives information about the concentration of the antigen in the sample.
Requirements for RIA
The procedure requires specific materials and reagents, including:
- Radioactive Labeled Antigen: The antigen of interest is labeled with a radioactive isotope, such as 125I (iodine-125), which is a commonly used isotope in RIA because it has a half-life of about 60 days, making it suitable for many experiments.
- Antibody: A specific antibody binding only to the antigen being measured. The antibody must have a high affinity for the antigen to ensure accurate and reliable results.
- Standard Antigen Solutions: These known antigen concentrations create a standard curve. The standard solutions help to calibrate the assay and allow the concentration of the unknown antigen in the sample to be calculated.
- Buffer Solutions: These solutions (e.g., phosphate-buffered saline) are used to maintain the pH of the reaction and help optimize the conditions for the antigen-antibody reaction.
- Separation System: Techniques to separate the bound antigen-antibody complexes from the unbound antigen, such as precipitation, centrifugation, or filtration. Solid-phase separation (e.g., antibody-coated microplates) can sometimes be used.
- Scintillation Counter: A device used to measure the radioactivity of the bound antigen-antibody complexes. This is typically done using scintillation liquid in which the sample is placed, and the radioactive decay is measured.
Procedure
The general procedure for conducting an RIA is as follows:
- Preparation of the Reagents:
- Prepare the radioactive-labeled antigen.
- Obtain or prepare the specific antibody to bind the antigen of interest.
- Prepare the standard curve with known concentrations of the antigen.
- Prepare the sample containing the unknown antigen.
- Incubation:
- Mix the sample, radioactive-labeled antigen, and specific antibody in a test tube or reaction vessel.
- The concentration of the labeled antigen is fixed, while the concentration of the unlabeled antigen varies (i.e., from the sample). Both the labeled and unlabeled antigens compete for the same antibody binding sites.
- The incubation period is typically set to ensure equilibrium between the antigen and antibody.
- Separation:
- After incubation, separate the antibody-bound antigen complexes from the free antigen (labeled or unlabeled).
- This can be done by using methods like:
- Centrifugation: The antigen-antibody complex precipitates, and the supernatant can be discarded.
- Filtration: Unbound antigen is removed via a filtration membrane.
- Chromatography: Separation based on physical properties.
- Measurement:
- Measure the radioactivity of the antibody-bound complex using a scintillation counter. This counter detects the radioactive decay emitted by the labeled antigen.
- Data Analysis:
- The amount of radioactivity measured is inversely proportional to the antigen concentration in the sample because the more unlabeled antigens, the fewer labeled antigens will bind to the antibody.
- The results are plotted against the standard curve, and the concentration of the antigen in the unknown sample is calculated.
- Results
- The amount of radioactivity in the bound fraction reflects the antigen concentration in the sample.
- A standard curve is generated by plotting known concentrations of the antigen against the measured radioactivity (counts per minute, CPM). The sample’s radioactivity is then compared to the standard curve to calculate the unknown concentration of the antigen.
The basic relationship in the results is:
- High Radioactivity: This means the concentration of the antigen in the sample is low (because less labeled antigen bound due to more competition).
- Low Radioactivity: This indicates that the antigen concentration is high in the sample (because more labeled antigens bound due to less competition).
Uses of RIA
RIA is used in various fields for the quantification of substances that can be detected via antigen-antibody binding:
- Hormonal Assays:
- Measurement of thyroid hormones (T3, T4), insulin, cortisol, and estrogen. RIA allows precise quantification of hormones at very low concentrations.
- Cancer Diagnosis:
- Detecting tumor markers, like prostate-specific antigen (PSA) or alpha-fetoprotein (AFP), can help diagnose and monitor cancer.
- Drug Monitoring:
- Therapeutic drug monitoring, where the concentration of drugs (e.g., digoxin, phenytoin) in patient blood samples is measured to ensure they are within the therapeutic range.
- Immunology:
- Measurement of antibodies in the blood, such as in detecting autoimmune diseases (e.g., rheumatoid factor in rheumatoid arthritis).
- Viral load measurement in HIV or other infectious diseases.
- Environmental and Toxicological Studies:
- Detection of toxic substances and pollutants, such as pesticides or heavy metals, in biological or environmental samples.
- Nutritional Studies:
- Measurement of vitamins (e.g., vitamin B12, vitamin D) or trace elements (e.g., iron, zinc) in biological fluids.
Advantages of RIA
- Sensitivity: RIA is highly sensitive and can measure low concentrations of substances (nanogram to picogram levels).
- Precision: Due to the high specificity of the antibody-antigen interaction, RIA provides accurate and precise results.
- Versatility: RIA can be used for various substances, including hormones, drugs, vitamins, and proteins.
- Quantification: Allows for the accurate quantification of substances in biological fluids.
Disadvantages of RIA
- Use of Radioactive Materials: The requirement to handle radioactive isotopes raises significant safety concerns and necessitates stringent handling and disposal protocols.
- Cost: Radioactive reagents, equipment (e.g., scintillation counters), and safety procedures increase the cost of RIA.
- Complexity: The technique is labour-intensive and requires trained personnel, including specialists handling radioactive materials.
- Environmental Impact: The disposal of radioactive waste requires adherence to strict regulations, which can be problematic and costly.
- Replacement by Non-Radioactive Techniques: Other techniques, like ELISA (Enzyme-Linked Immunosorbent Assay), have replaced RIA in many applications due to the absence of radioactive materials and simpler procedures.