Introduction
-
Salmonella is a clinically important Gram-negative bacterium belonging to the family Enterobacteriaceae.
-
It is a major cause of food-borne illnesses and systemic infections worldwide.
-
The genus Salmonella includes numerous serovars, with Salmonella Typhi, Salmonella Paratyphi, Salmonella Typhimurium, and Salmonella Enteritidis being most significant in humans.
-
Infection occurs primarily through contaminated food or water, especially poultry, eggs, meat, and dairy products.
-
Salmonella causes a wide spectrum of diseases ranging from acute gastroenteritis to enteric (typhoid) fever and septicemia.
-
The organism possesses multiple virulence factors that enable invasion, intracellular survival, and systemic spread.
-
Laboratory diagnosis relies on culture, biochemical tests, and serotyping.
-
Increasing antibiotic resistance among Salmonella strains poses a major public health challenge.
-
Prevention depends on food safety measures, vaccination (for typhoid), and public health surveillance.
-
Continuous research and monitoring are essential to control emerging resistant strains and outbreaks.
General Characteristics
-
Genus: Salmonella
-
Species: Salmonella enterica
-
Includes multiple serovars such as S. Typhi, S. Paratyphi, S. Typhimurium, and S. Enteritidis
-
-
Family: Enterobacteriaceae
-
Gram Staining:
-
Gram-negative bacteria
-
Appear pink on Gram stain due to a thin peptidoglycan layer and presence of an outer membrane
-
-
Shape: Rod-shaped (bacilli)
-
Arrangement:
-
Commonly seen as single bacilli
-
May occasionally appear in pairs or short chains
-
-
Oxygen Requirement:
-
Facultative anaerobes
-
Capable of growth in both aerobic and anaerobic environments
-
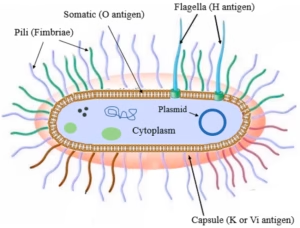
Morphology
Cell Wall Structure
-
Composed of:
-
Thin peptidoglycan layer
-
Outer membrane containing lipopolysaccharide (LPS)
-
-
LPS acts as endotoxin, playing a key role in:
-
Fever
-
Inflammation
-
Septic shock in severe infections
-
Flagella
-
Most Salmonella species are motile
-
Possess peritrichous flagella
-
Flagella enhance:
-
Motility
-
Invasion of intestinal mucosa
-
Spread within host tissues
-
Cultural Characteristics
 Growth Media
Growth Media
-
MacConkey Agar
-
Selective for Gram-negative bacteria
-
Salmonella produces colourless colonies (non-lactose fermenter)
-
-
XLD Agar (Xylose Lysine Deoxycholate)
-
Produces red colonies with black centres
-
Black colour due to hydrogen sulfide (H₂S) production
-
-
Hektoen Enteric Agar
-
Colonies appear green with black centres
-
Useful for differentiating Salmonella from Shigella
-
Colony Morphology
-
Pale or colourless colonies
-
Absence of lactose fermentation
-
Black centres indicate H₂S production
Growth Conditions
-
Optimal temperature: 37°C
-
pH range: 6.0 – 7.5
Biochemical Reactions
| Test | Reaction |
|---|---|
| Catalase | Positive |
| Oxidase | Negative |
| Lactose fermentation | Negative (rare exceptions) |
| Indole test | Variable (some strains positive) |
| Methyl Red | Positive |
| Voges–Proskauer | Negative |
These biochemical reactions help in laboratory confirmation and differentiation from other enteric bacteria.
Pathogenicity
Virulence Factors
-
Type III Secretion System (T3SS):
-
Injects bacterial proteins into host cells
-
Facilitates invasion and intracellular survival
-
-
Adhesins:
-
Enable attachment to intestinal epithelial cells
-
-
Endotoxin (LPS):
-
Triggers strong inflammatory and immune responses
-
Mechanism of Infection
-
Entry through contaminated food or water
-
Invasion of intestinal mucosa
-
Survival within macrophages
-
Systemic dissemination in invasive strains
Clinical Infections
Gastroenteritis
-
Commonly caused by S. Typhimurium and S. Enteritidis
-
Symptoms:
-
Diarrhoea
-
Fever
-
Abdominal cramps
-
Vomiting
-
Typhoid Fever
-
Caused by S. Typhi
-
Characterized by:
-
Prolonged fever
-
Abdominal pain
-
Hepatosplenomegaly
-
Systemic toxicity
-
Enteric Fever
-
Caused by S. Typhi and S. Paratyphi
-
Severe systemic illness
Bacteremia and Sepsis
-
Seen in:
-
Immunocompromised patients
-
Elderly
-
Infants
-
Laboratory Diagnosis
1. Specimen Collection
The choice of specimen depends on the clinical syndrome:
-
Stool sample
-
Gastroenteritis
-
Carrier detection
-
-
Blood
-
Early stage of typhoid / enteric fever (1st week)
-
-
Urine
-
Later stages of enteric fever
-
-
Bone marrow
-
Most sensitive specimen in typhoid fever
-
-
Other samples
-
Pus, CSF, or tissue (in systemic infections)
-
Proper aseptic collection and rapid transport are crucial to avoid contamination.
2. Microscopic Examination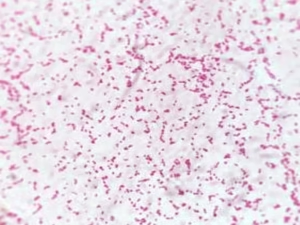
Gram Staining
-
Shows Gram-negative bacilli
-
Appear as pink, slender rods
-
Non-sporing, non-capsulated
🔹 Note: Microscopy alone is not confirmatory but helps in early suspicion.
3. Culture Techniques
A. Primary Culture
Specimens are inoculated onto selective and differential media:
-
MacConkey Agar
-
Non-lactose fermenting → colourless colonies
-
-
XLD Agar (Xylose Lysine Deoxycholate)
-
Red colonies with black centres
-
Black colour due to H₂S production
-
-
Hektoen Enteric Agar
-
Green colonies with black centres
-
-
Blood Agar
-
Non-haemolytic colonies
-
B. Enrichment Media
Used when bacterial load is low:
-
Selenite F broth
-
Tetrathionate broth
These suppress normal gut flora and promote Salmonella growth.
4. Biochemical Identification
Isolated colonies are subjected to biochemical tests:
| Test | Result |
|---|---|
| Catalase | Positive |
| Oxidase | Negative |
| Lactose fermentation | Negative |
| Indole | Variable |
| Methyl Red | Positive |
| Voges–Proskauer | Negative |
| H₂S production | Positive (most strains) |
These reactions confirm genus-level identification.
5. Serological Identification (Serotyping)
-
Based on Kauffmann–White classification
-
Detection of:
-
O (somatic) antigens
-
H (flagellar) antigens
-
-
Helps in:
-
Identifying specific serovars (e.g., S. Typhi)
-
Epidemiological surveillance
-
Outbreak investigations
-
6. Serological Tests (Indirect Diagnosis)
Widal Test
-
Detects antibodies against O and H antigens
-
Useful after 1st week of illness
-
Limitations:
-
False positives
-
Prior vaccination or infection
-
-
Interpretation must consider baseline titres
Widal test is supportive, not confirmatory.
7. Molecular Methods
-
PCR-based assays
-
Rapid and sensitive
-
Detect specific Salmonella genes
-
-
Used in:
-
Reference laboratories
-
Outbreak investigations
-
8. Antibiotic Susceptibility Testing
-
Performed on all confirmed isolates
-
Detects:
-
Multidrug-resistant strains
-
Fluoroquinolone resistance
-
-
Guides appropriate antibiotic therapy
Antibiotic Resistance
Emerging Resistance
-
Increasing resistance due to:
-
Overuse of antibiotics
-
Food-animal transmission
-
Multidrug-Resistant Salmonella
-
Resistance to:
-
Ampicillin
-
Chloramphenicol
-
Trimethoprim-sulfamethoxazole
-
Treatment Considerations
-
Antibiotic susceptibility testing is essential
-
Commonly used drugs:
-
Fluoroquinolones
-
Third-generation cephalosporins
-
Prevention and Control
Food Safety
-
Proper cooking of food
-
Safe water supply
-
Good personal hygiene
Vaccination
-
Typhoid vaccines available:
-
Oral (live attenuated)
-
Injectable (polysaccharide)
-
-
Recommended for travellers to endemic areas
Public Health Surveillance
-
Monitoring outbreaks
-
Food safety inspections
-
Antibiotic resistance tracking
MCQs
1. Salmonella belongs to which family?
A. Vibrionaceae
B. Enterobacteriaceae
C. Pseudomonadaceae
D. Neisseriaceae
Answer: B
2. Salmonella is a:
A. Gram-positive coccus
B. Gram-negative bacillus
C. Gram-positive bacillus
D. Acid-fast bacillus
Answer: B
3. Gram staining of Salmonella shows:
A. Purple cocci
B. Pink rods
C. Blue rods
D. Red cocci
Answer: B
4. Oxygen requirement of Salmonella is:
A. Obligate aerobe
B. Obligate anaerobe
C. Facultative anaerobe
D. Microaerophile
Answer: C
5. Most common habitat of Salmonella is:
A. Soil
B. Water
C. Intestinal tract
D. Skin
Answer: C
6. Salmonella Typhi primarily causes:
A. Food poisoning
B. Dysentery
C. Typhoid fever
D. Cholera
Answer: C
7. Salmonella Typhimurium commonly causes:
A. Typhoid fever
B. Gastroenteritis
C. Pneumonia
D. Meningitis
Answer: B
8. Motility in Salmonella is due to:
A. Pili
B. Fimbriae
C. Flagella
D. Capsule
Answer: C
9. Flagella arrangement in Salmonella is:
A. Monotrichous
B. Amphitrichous
C. Lophotrichous
D. Peritrichous
Answer: D
10. Salmonella is:
A. Lactose fermenter
B. Non-lactose fermenter
C. Late lactose fermenter
D. Sucrose fermenter
Answer: B
11. On MacConkey agar, Salmonella produces:
A. Pink colonies
B. Green colonies
C. Colourless colonies
D. Mucoid colonies
Answer: C
12. XLD agar shows Salmonella colonies as:
A. Yellow colonies
B. Red colonies with black centre
C. Green colonies without black centre
D. Pink colonies
Answer: B
13. Black centre in Salmonella colonies is due to:
A. Lactose fermentation
B. Gas production
C. Hydrogen sulfide production
D. Acid formation
Answer: C
14. Salmonella is oxidase:
A. Positive
B. Negative
C. Variable
D. Weakly positive
Answer: B
15. Salmonella is catalase:
A. Negative
B. Variable
C. Weakly positive
D. Positive
Answer: D
16. Methyl red test for Salmonella is:
A. Negative
B. Weak positive
C. Positive
D. Variable
Answer: C
17. Voges–Proskauer test in Salmonella is:
A. Positive
B. Negative
C. Variable
D. Weak positive
Answer: B
18. Indole production in Salmonella is:
A. Always positive
B. Always negative
C. Variable
D. Strongly positive
Answer: C
19. Major virulence factor of Salmonella is:
A. Capsule
B. Exotoxin
C. Type III secretion system
D. Coagulase
Answer: C
20. Endotoxin of Salmonella is:
A. Peptidoglycan
B. Lipopolysaccharide
C. Teichoic acid
D. Protein A
Answer: B
21. Route of transmission of Salmonella is mainly:
A. Airborne
B. Vector-borne
C. Feco-oral
D. Sexual
Answer: C
22. Most common specimen for diagnosis of gastroenteritis is:
A. Blood
B. Stool
C. Urine
D. CSF
Answer: B
23. Best specimen for early diagnosis of typhoid fever is:
A. Stool
B. Urine
C. Blood
D. Saliva
Answer: C
24. Most sensitive specimen for Salmonella Typhi isolation is:
A. Stool
B. Blood
C. Urine
D. Bone marrow
Answer: D
25. Gold standard for diagnosis of Salmonella infection is:
A. Widal test
B. PCR
C. Culture
D. ELISA
Answer: C
26. Widal test detects antibodies against:
A. K antigen
B. O and H antigens
C. Vi antigen only
D. Capsule
Answer: B
27. Limitation of Widal test is:
A. Low sensitivity
B. False positivity
C. Cannot detect antibodies
D. Always negative
Answer: B
28. Serotyping of Salmonella is based on:
A. Sugar fermentation
B. Antibiotic resistance
C. O and H antigens
D. Capsule
Answer: C
29. Kauffmann–White scheme is used for:
A. Antibiotic testing
B. Serotyping
C. Culture identification
D. Molecular diagnosis
Answer: B
30. Salmonella causes bacteremia commonly in:
A. Healthy adults
B. Immunocompromised patients
C. Athletes
D. Pregnant women only
Answer: B
31. Enteric fever is caused by:
A. Salmonella Typhimurium
B. Salmonella Enteritidis
C. Salmonella Typhi
D. Salmonella Arizonae
Answer: C
32. Incubation period of typhoid fever is approximately:
A. 1–2 days
B. 3–5 days
C. 7–14 days
D. 1 month
Answer: C
33. Chronic carrier state in typhoid is associated with:
A. Kidney
B. Gall bladder
C. Intestine
D. Liver
Answer: B
34. Multidrug-resistant Salmonella shows resistance to:
A. Penicillin only
B. Ampicillin, chloramphenicol, cotrimoxazole
C. Vancomycin
D. Linezolid
Answer: B
35. Preferred treatment for MDR typhoid fever is:
A. Penicillin
B. Aminoglycosides
C. Fluoroquinolones / Cephalosporins
D. Tetracycline
Answer: C
36. Antibiotic susceptibility testing is important because of:
A. High virulence
B. Emerging resistance
C. Slow growth
D. Capsule formation
Answer: B
37. Typhoid vaccine is available against:
A. Salmonella Typhimurium
B. Salmonella Enteritidis
C. Salmonella Typhi
D. All Salmonella species
Answer: C
38. Oral typhoid vaccine is:
A. Killed vaccine
B. Subunit vaccine
C. Live attenuated vaccine
D. Toxoid
Answer: C
39. Injectable typhoid vaccine is:
A. Live vaccine
B. Polysaccharide vaccine
C. DNA vaccine
D. Vector vaccine
Answer: B
40. Main source of Salmonella infection is:
A. Air
B. Soil
C. Contaminated food and water
D. Insects
Answer: C
41. Common food associated with Salmonella is:
A. Fruits
B. Milk products
C. Poultry and eggs
D. Cereals
Answer: C
42. Salmonella survives inside host cells mainly in:
A. Neutrophils
B. Macrophages
C. RBCs
D. Platelets
Answer: B
43. Fever in typhoid is due to:
A. Exotoxin
B. Endotoxin
C. Capsule
D. Enzyme
Answer: B
44. Rose spots in typhoid are due to:
A. Allergy
B. Endotoxin-induced vasodilation
C. Platelet destruction
D. Hemorrhage
Answer: B
45. Relapse in typhoid fever occurs due to:
A. Reinfection
B. Incomplete treatment
C. New strain
D. Vaccine failure
Answer: B
46. Which test differentiates Salmonella from E. coli?
A. Gram stain
B. Lactose fermentation
C. Catalase test
D. Capsule stain
Answer: B
47. Salmonella is non-spore forming and:
A. Capsulated
B. Acid-fast
C. Non-capsulated
D. Branching
Answer: C
48. Public health control of Salmonella includes:
A. Isolation only
B. Vaccination and food hygiene
C. Chemoprophylaxis
D. Sterilization
Answer: B
49. Most important preventive measure for Salmonella infection is:
A. Antibiotics
B. Vaccination alone
C. Food safety and hygiene
D. Hospitalization
Answer: C
50. Salmonella remains a public health problem mainly due to:
A. Fastidious nature
B. Antibiotic resistance and foodborne spread
C. Capsule formation
D. Lack of diagnosis
Answer: B