
Introduction
-
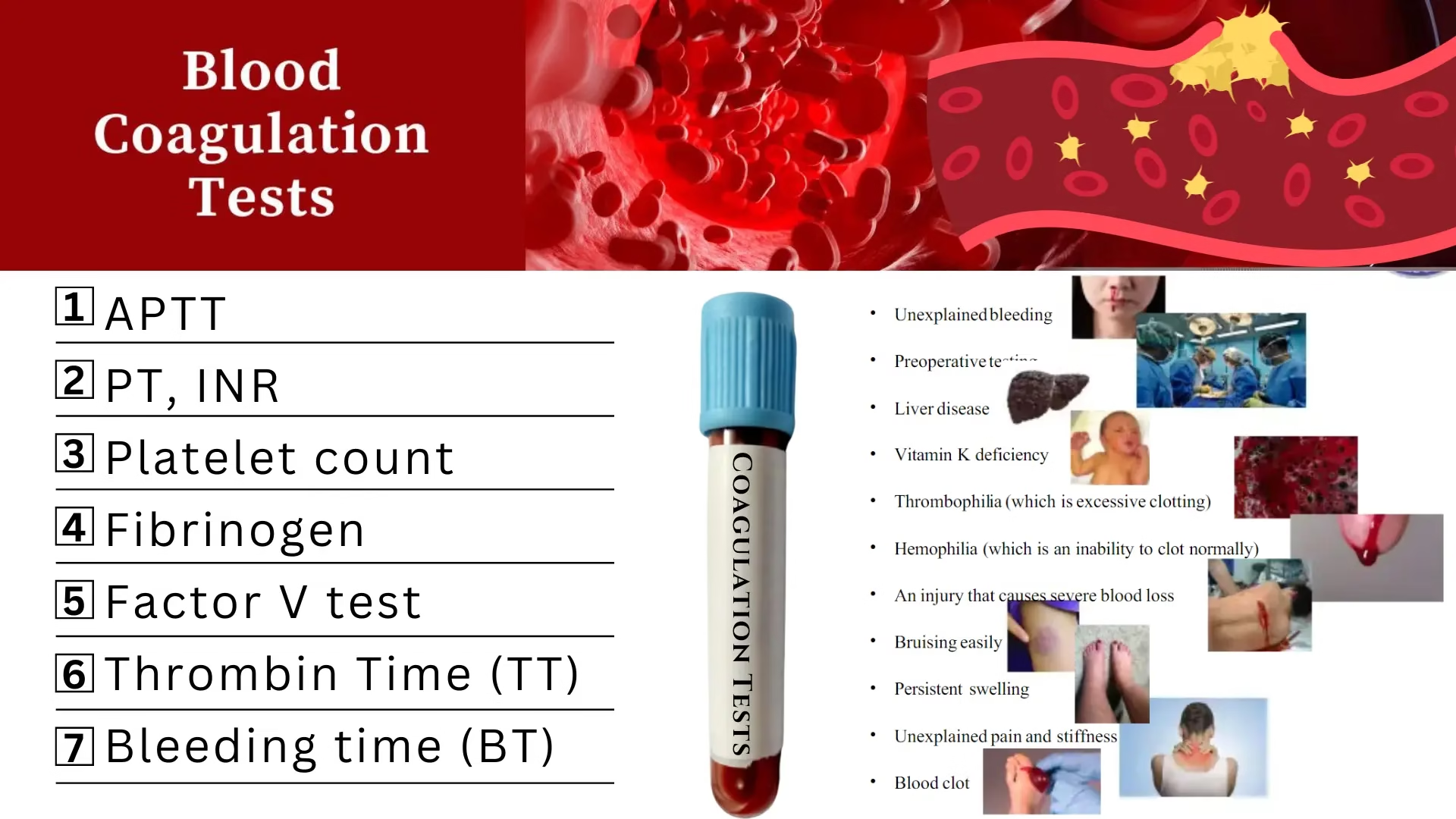
Screening coagulation tests are initial laboratory investigations used to assess the hemostatic system.
-
These tests help in the early detection of bleeding and clotting disorders.
-
They evaluate the integrity of the coagulation pathways rather than specific clotting factors.
-
Screening tests are used as first-line tests before performing specific factor assays.
-
They assess both primary and secondary hemostasis.
-
These tests are commonly performed in patients with bleeding tendency, pre-operative evaluation, and anticoagulant therapy monitoring.
-
Screening coagulation tests help to localize the defect to a particular pathway of coagulation.
-
They are simple, rapid, and cost-effective laboratory tests.
-
Abnormal results indicate the need for further confirmatory investigations.
-
These tests are routinely included in the coagulation profile.
Prothrombin Time
Principle
Prothrombin Time is based on the principle that:
When tissue thromboplastin (factor III) and calcium ions are added to citrated plasma, clot formation occurs via activation of the extrinsic pathway.
The time taken for the formation of a visible fibrin clot is recorded as Prothrombin Time.
PT primarily evaluates:
-
Factor VII (extrinsic pathway)
-
Factors X, V, II (prothrombin), and fibrinogen (common pathway)
Specimen
-
Sample: Venous blood
-
Anticoagulant: 3.2% Sodium citrate
-
Blood : Anticoagulant ratio: 9 : 1
-
Specimen used: Platelet-poor plasma
Requirements
-
Citrated plasma (patient sample)
-
PT reagent (thromboplastin with calcium)
-
Test tubes
-
Water bath / Incubator at 37°C
-
Stopwatch
-
Pipettes
-
Centrifuge
Method
One-stage Prothrombin Time method
Procedure
-
Collect venous blood into a tube containing 3.2% sodium citrate (9:1 ratio).
-
Centrifuge the sample to obtain platelet-poor plasma.
-
Pre-warm PT reagent and plasma at 37°C.
-
Pipette 0.1 mL of plasma into a test tube.
-
Add 0.2 mL of pre-warmed thromboplastin reagent.
-
Start the stopwatch immediately.
-
Observe for clot formation.
-
Stop the timer at the first appearance of a visible clot.
-
Record the clotting time in seconds.
Normal Range
-
Prothrombin Time (PT):
11 – 15 seconds (may vary slightly with reagent and laboratory) -
INR (International Normalized Ratio):
0.8 – 1.2 (in normal individuals)
Clinical Significance
Prolonged PT is seen in:
-
Vitamin K deficiency
-
Liver diseases
-
Warfarin therapy
-
Disseminated intravascular coagulation (DIC)
-
Deficiency of clotting factors VII, X, V, II, fibrinogen.
Activated Partial Thromboplastin Time
Principle
Activated Partial Thromboplastin Time is based on the principle that:
When partial thromboplastin (phospholipid) and an activator are added to citrated plasma, followed by calcium ions, clot formation occurs via activation of the intrinsic pathway.
The time taken for the formation of a visible fibrin clot is measured as APTT.
APTT evaluates:
-
Intrinsic pathway factors: XII, XI, IX, VIII
-
Common pathway factors: X, V, II (prothrombin), fibrinogen
Specimen
-
Sample: Venous blood
-
Anticoagulant: 3.2% Sodium citrate
-
Blood : Anticoagulant ratio: 9 : 1
-
Specimen used: Platelet-poor plasma
Requirements
-
Citrated plasma (patient sample)
-
APTT reagent (partial thromboplastin with activator)
-
Calcium chloride (0.025 M)
-
Test tubes
-
Water bath / Incubator at 37°C
-
Stopwatch
-
Pipettes
-
Centrifuge
Method
One-stage Activated Partial Thromboplastin Time method
Procedure
-
Collect venous blood in a tube containing 3.2% sodium citrate (9:1 ratio).
-
Centrifuge to obtain platelet-poor plasma.
-
Pipette 0.1 mL of plasma into a test tube.
-
Add 0.1 mL of APTT reagent.
-
Mix gently and incubate at 37°C for 3 minutes.
-
Add 0.1 mL of pre-warmed calcium chloride.
-
Start the stopwatch immediately.
-
Observe for clot formation.
-
Stop the timer at the first appearance of a visible clot.
-
Record the time in seconds.
Normal Range
-
Activated Partial Thromboplastin Time (APTT): 35 – 40 seconds
Clinical Significance
Prolonged APTT is seen in:
-
Hemophilia A (Factor VIII deficiency)
-
Hemophilia B (Factor IX deficiency)
-
Von Willebrand disease
-
Heparin therapy
-
Disseminated intravascular coagulation (DIC)
-
Severe liver disease
-
Deficiency of intrinsic pathway factors
Thrombin Time
Principle
Thrombin Time is based on the principle that:
When a standard amount of thrombin is added to citrated plasma, it converts fibrinogen into fibrin, resulting in clot formation.
The time taken for the appearance of a visible fibrin clot is recorded as Thrombin Time.
TT evaluates:
-
Fibrinogen concentration and function
-
Presence of inhibitors of thrombin or fibrin polymerization
Specimen
-
Sample: Venous blood
-
Anticoagulant: 3.2% Sodium citrate
-
Blood : Anticoagulant ratio: 9 : 1
-
Specimen used: Platelet-poor plasma
Requirements
-
Citrated plasma (patient sample)
-
Thrombin reagent
-
Test tubes
-
Water bath / Incubator at 37°C
-
Stopwatch
-
Pipettes
-
Centrifuge
Method
Direct Thrombin Time method
Procedure
-
Collect venous blood into a tube containing 3.2% sodium citrate (9:1 ratio).
-
Centrifuge to obtain platelet-poor plasma.
-
Pre-warm plasma and thrombin reagent at 37°C.
-
Pipette 0.1 mL of plasma into a test tube.
-
Add 0.1 mL of thrombin reagent.
-
Start the stopwatch immediately.
-
Observe for clot formation.
-
Stop the timer at the first appearance of a visible clot.
-
Record the clotting time in seconds.
Normal Range
-
Thrombin Time (TT): 14 – 19 seconds
Clinical Significance
Prolonged Thrombin Time is seen in:
-
Hypofibrinogenemia
-
Afibrinogenemia
-
Dysfibrinogenemia
-
Heparin therapy
-
Disseminated intravascular coagulation (DIC)
-
Presence of fibrin degradation products (FDPs)
Fibrinogen
Principle
Fibrinogen estimation is based on the principle that:
When excess thrombin is added to diluted citrated plasma, fibrinogen is converted into fibrin.
The clotting time is inversely proportional to the fibrinogen concentration in the plasma.
Using a calibration curve, the fibrinogen concentration is determined from the clotting time.
Specimen
-
Sample: Venous blood
-
Anticoagulant: 3.2% Sodium citrate
-
Blood : Anticoagulant ratio: 9 : 1
-
Specimen used: Platelet-poor plasma
Requirements
-
Citrated plasma (patient sample)
-
Thrombin reagent (high concentration)
-
Fibrinogen standard
-
Buffer solution
-
Test tubes
-
Water bath / Incubator at 37°C
-
Stopwatch
-
Pipettes
-
Centrifuge
Method
Clauss Fibrinogen Method
Procedure
-
Collect venous blood in a tube containing 3.2% sodium citrate (9:1 ratio).
-
Centrifuge to obtain platelet-poor plasma.
-
Dilute plasma with buffer as specified.
-
Pre-warm diluted plasma and thrombin reagent at 37°C.
-
Pipette 0.2 mL of diluted plasma into a test tube.
-
Add 0.1 mL of thrombin reagent.
-
Start the stopwatch immediately.
-
Observe for clot formation.
-
Record the clotting time.
-
Determine fibrinogen concentration using a standard calibration curve.
Normal Range
-
Plasma Fibrinogen: 200 – 400 mg/dL
Clinical Significance
Decreased Fibrinogen
-
Hypofibrinogenemia
-
Afibrinogenemia
-
Disseminated intravascular coagulation (DIC)
-
Severe liver disease
-
Massive hemorrhage
Increased Fibrinogen
-
Acute and chronic inflammation
-
Pregnancy
-
Diabetes mellitus
-
Cardiovascular diseases
-
Malignancy
Platelet Count
Principle
Platelet count is based on the principle that:
Platelets are counted either manually using a hemocytometer after appropriate dilution with a platelet diluting fluid, or automatically using hematology analyzers based on electrical impedance or optical methods.
In the manual method, platelets are counted under a microscope in a defined area, and the total number per microliter of blood is calculated.
Specimen
-
Sample: Venous blood
-
Anticoagulant: EDTA
-
Specimen used: Whole blood
-
Alternative sample: Capillary blood (finger prick)
Requirements (Manual Method)
-
EDTA anticoagulated blood
-
Platelet diluting fluid (e.g., Rees–Ecker fluid)
-
RBC pipette / micropipette
-
Hemocytometer (Neubauer chamber)
-
Cover slip
-
Microscope
-
Timer
Method
Manual Platelet Count using Hemocytometer
Procedure
-
Collect venous blood in an EDTA tube and mix gently.
-
Dilute blood with platelet diluting fluid (usually 1:100 dilution).
-
Mix thoroughly to ensure uniform distribution of platelets.
-
Charge the Neubauer counting chamber with diluted sample.
-
Allow the platelets to settle for 10–15 minutes.
-
Focus under high power objective.
-
Count platelets in the central large square of the chamber.
-
Calculate platelet count using the standard formula.
Calculation
Platelet count = Number of platelets counted × Dilution factor / Volume counted
Result expressed as:
-
cells/µL or cells/mm³
Normal Range
-
Platelet count:
150,000 – 400,000 /µL
Clinical Significance
Decreased Platelet Count (Thrombocytopenia)
-
Aplastic anemia
-
Bone marrow suppression
-
Dengue fever
-
Disseminated intravascular coagulation (DIC)
-
Drug-induced thrombocytopenia
Increased Platelet Count (Thrombocytosis)
-
Chronic infections
-
Iron deficiency anemia
-
Myeloproliferative disorders
-
Post-splenectomy
-
Inflammatory conditions
MCQs
1. Screening coagulation tests are primarily used to assess:
A. RBC disorders
B. Platelet morphology
C. Hemostatic function
D. Immune response
Answer: C
2. Which of the following is NOT a screening coagulation test?
A. Prothrombin Time
B. Activated Partial Thromboplastin Time
C. Thrombin Time
D. Bleeding Time
E. Factor VIII assay
Answer: E
3. Prothrombin Time (PT) assesses which pathway?
A. Intrinsic
B. Extrinsic
C. Fibrinolytic
D. Platelet pathway
Answer: B
4. APTT evaluates which coagulation pathway?
A. Extrinsic
B. Common only
C. Intrinsic
D. Platelet activation
Answer: C
5. Thrombin Time primarily evaluates:
A. Prothrombin
B. Platelet function
C. Fibrinogen conversion to fibrin
D. Factor VII activity
Answer: C
6. Platelet count is a test of:
A. Secondary hemostasis
B. Fibrinolysis
C. Primary hemostasis
D. Coagulation cascade
Answer: C
7. Normal Prothrombin Time range is approximately:
A. 5–8 seconds
B. 8–10 seconds
C. 11–15 seconds
D. 20–30 seconds
Answer: C
8. Normal APTT range is:
A. 10–15 seconds
B. 15–20 seconds
C. 25–35 seconds
D. 40–60 seconds
Answer: C
9. Normal Thrombin Time is:
A. 5–8 seconds
B. 10–12 seconds
C. 14–19 seconds
D. 25–30 seconds
Answer: C
10. Normal platelet count is:
A. 50,000–100,000/µL
B. 100,000–150,000/µL
C. 150,000–400,000/µL
D. 400,000–600,000/µL
Answer: C
11. PT is prolonged in deficiency of:
A. Factor VIII
B. Factor IX
C. Factor VII
D. Factor XII
Answer: C
12. APTT is prolonged in:
A. Hemophilia A
B. Vitamin K deficiency
C. Factor VII deficiency
D. Polycythemia
Answer: A
13. Thrombin Time is prolonged in:
A. Thrombocytopenia
B. Heparin therapy
C. Factor VII deficiency
D. Iron deficiency anemia
Answer: B
14. Screening coagulation tests are performed using which specimen?
A. Serum
B. Whole blood
C. Citrated plasma
D. Heparinized plasma
Answer: C
15. Anticoagulant used for PT and APTT is:
A. EDTA
B. Heparin
C. Sodium citrate
D. Oxalate
Answer: C
16. Blood to anticoagulant ratio for coagulation tests is:
A. 1:1
B. 4:1
C. 9:1
D. 10:1
Answer: C
17. PT is commonly used to monitor therapy with:
A. Heparin
B. Aspirin
C. Warfarin
D. Clopidogrel
Answer: C
18. APTT is commonly used to monitor:
A. Warfarin therapy
B. Heparin therapy
C. Fibrinolytic therapy
D. Platelet transfusion
Answer: B
19. Bleeding Time primarily assesses:
A. Coagulation factors
B. Platelet function
C. Fibrinogen level
D. Liver function
Answer: B
20. A prolonged PT with normal APTT suggests deficiency of:
A. Factor VIII
B. Factor IX
C. Factor VII
D. Factor XII
Answer: C
21. A prolonged APTT with normal PT indicates deficiency of:
A. Factor VII
B. Factor VIII
C. Factor V
D. Fibrinogen
Answer: B
22. Prolongation of both PT and APTT is seen in:
A. Hemophilia A
B. Vitamin K deficiency
C. Platelet disorders
D. Von Willebrand disease
Answer: B
23. Thrombin Time is unaffected by deficiency of:
A. Fibrinogen
B. Prothrombin
C. Heparin
D. FDPs
Answer: B
24. Platelet count is decreased in:
A. Dengue fever
B. Polycythemia vera
C. Dehydration
D. Iron overload
Answer: A
25. Screening coagulation tests are performed at:
A. Room temperature
B. 25°C
C. 37°C
D. 40°C
Answer: C
26. INR is derived from which test?
A. APTT
B. TT
C. PT
D. Bleeding time
Answer: C
27. Normal INR value is:
A. 0.5–0.7
B. 0.8–1.2
C. 1.5–2.0
D. 2.5–3.5
Answer: B
28. Screening tests are first-line tests for:
A. Specific factor assay
B. Bleeding disorders
C. Genetic studies
D. Bone marrow disorders
Answer: B
29. APTT reagent contains:
A. Thrombin only
B. Tissue thromboplastin
C. Phospholipid and activator
D. Calcium only
Answer: C
30. PT reagent contains:
A. Thrombin
B. Partial thromboplastin
C. Tissue thromboplastin with calcium
D. EDTA
Answer: C
31. Platelet count is part of:
A. Coagulation profile
B. Bleeding profile
C. Complete blood count
D. Liver function test
Answer: C
32. Screening coagulation tests do NOT include:
A. PT
B. APTT
C. TT
D. Factor IX assay
Answer: D
33. Thrombin Time bypasses which step?
A. Intrinsic pathway
B. Extrinsic pathway
C. Prothrombin activation
D. Fibrin formation
Answer: C
34. Platelet count is best measured using:
A. Citrated plasma
B. EDTA blood
C. Serum
D. Heparinized blood
Answer: B
35. Prolonged bleeding time with normal PT and APTT suggests:
A. Factor deficiency
B. Platelet disorder
C. Liver disease
D. Vitamin K deficiency
Answer: B
36. Which factor is NOT assessed by APTT?
A. Factor VIII
B. Factor IX
C. Factor XII
D. Factor VII
Answer: D
37. Which factor is NOT assessed by PT?
A. Factor VII
B. Factor X
C. Factor V
D. Factor VIII
Answer: D
38. Thrombin Time is useful in detecting:
A. Platelet defects
B. Heparin contamination
C. Factor VII deficiency
D. Vitamin K deficiency
Answer: B
39. Screening coagulation tests help in diagnosing:
A. Leukemia
B. Anemia
C. Bleeding disorders
D. Diabetes
Answer: C
40. Which condition prolongs only APTT?
A. Hemophilia A
B. Vitamin K deficiency
C. Liver disease
D. DIC
Answer: A
41. PT, APTT, and TT together assess:
A. Primary hemostasis only
B. Secondary hemostasis
C. Fibrinolysis only
D. Platelet adhesion
Answer: B
42. Screening coagulation tests are performed before:
A. Platelet count
B. Factor assays
C. CBC
D. Blood grouping
Answer: B
43. Which test is most sensitive to fibrinogen abnormalities?
A. PT
B. APTT
C. TT
D. Bleeding time
Answer: C
44. Platelet count below 150,000/µL is called:
A. Thrombocytosis
B. Thrombocythemia
C. Thrombocytopenia
D. Pancytopenia
Answer: C
45. Screening coagulation tests are usually ordered in:
A. Fever
B. Bleeding tendency
C. Hypertension
D. Diabetes
Answer: B
46. APTT is prolonged in which anticoagulant therapy?
A. Warfarin
B. Aspirin
C. Heparin
D. Clopidogrel
Answer: C
47. PT is prolonged earliest in:
A. Factor VIII deficiency
B. Factor IX deficiency
C. Factor VII deficiency
D. Factor XII deficiency
Answer: C
48. Which test evaluates platelet number?
A. Bleeding time
B. Platelet count
C. PT
D. APTT
Answer: B
49. Screening coagulation tests require plasma that is:
A. Hemolyzed
B. Clotted
C. Platelet-poor
D. Lipemic
Answer: C
50. Screening coagulation tests are best described as:
A. Diagnostic tests
B. Confirmatory tests
C. Preliminary tests
D. Genetic tests
Answer: C