Introduction
-
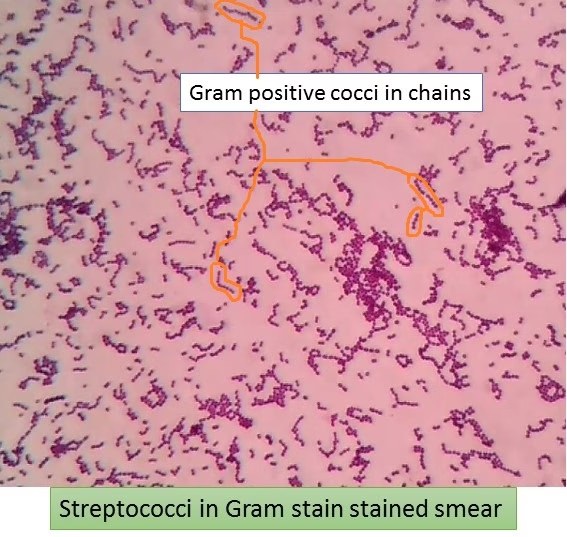
Streptococci are Gram-positive, spherical (cocci) bacteria that typically arrange in chains or pairs.
-
They belong to the family Streptococcaceae and are medically important pathogens.
-
Streptococci are non-motile, non-spore-forming, and usually non-capsulated (except some species).
-
They are facultative anaerobes, growing best in environments with reduced oxygen tension.
-
Streptococci are catalase-negative, which helps differentiate them from Staphylococci.
-
Many species are normal commensals of the upper respiratory tract, oral cavity, gastrointestinal tract, and skin.
-
Some species are pathogenic and cause diseases such as pharyngitis, pneumonia, rheumatic fever, endocarditis, and septicemia.
-
Classification is commonly based on hemolytic pattern on blood agar (alpha, beta, gamma hemolysis).
-
Further classification is done using Lancefield grouping based on cell wall carbohydrate antigens.
-
Streptococci are of major importance in clinical microbiology, laboratory diagnosis, and public health.
General Character
- Genus: Streptococcus
- Family: Streptococcaceae
- Gram Staining: Streptococci are Gram-positive bacteria, appearing purple due to their thick peptidoglycan layer.
- Shape and Arrangement:
- Shape: They are spherical (cocci).
- Arrangement: Streptococci typically occur in chains or pairs, resulting from division in one plane.
- Oxygen Requirements: Streptococci can be classified based on their oxygen requirements:
- Facultative anaerobes: Can grow in aerobic and anaerobic conditions (e.g., Streptococcus pneumoniae).
- Obligate anaerobes: Require an oxygen-free environment for growth (e.g., Streptococcus pyogenes).
Morphology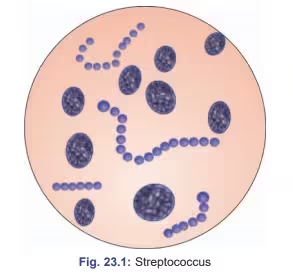
- Cell Wall Structure:
- It comprises a thick peptidoglycan layer, crucial for maintaining shape and protecting against osmotic lysis.
- The cell wall contains various polysaccharides, contributing to serological classification (Lancefield classification).
- Capsule: Some species (e.g., S. pneumoniae) produce a polysaccharide capsule that enhances virulence by preventing phagocytosis.
- Surface Structures:
- Teichoic Acids: Present in the cell wall, involved in cell wall maintenance and regulation of cell growth.
- M Protein: Found in the cell wall of certain species (e.g., S. pyogenes), it plays a key role in virulence by inhibiting phagocytosis and promoting adherence.
Cultural Characteristics
- Growth Media:
- Blood Agar: A differential medium that supports the growth of streptococci and allows for observing hemolytic patterns.
- α-Hemolysis: Partial hemolysis (e.g., S. pneumoniae).
- β-Hemolysis: Complete hemolysis (e.g., S. pyogenes).
- γ-Hemolysis: No hemolysis (e.g., S. epidermidis).
- Selective Media: Some species can be grown on selective media like bile esculin agar for certain enterococci.
- Blood Agar: A differential medium that supports the growth of streptococci and allows for observing hemolytic patterns.
- Colony Appearance:
- Colonies vary in size and color; β-hemolytic streptococci generally form clear zones around colonies on blood agar.
- Temperature and pH Range:
- Optimal growth occurs at 35-37°C. Some species can grow at temperatures as low as 10°C or as high as 45°C.
- They prefer a neutral pH for optimal growth.
Biochemical Reactions
- Catalase Test: Streptococci are catalase-negative, which distinguishes them from staphylococci.
- Hemolysis Patterns:
- Observed on blood agar as α, β, or γ hemolysis, used for preliminary classification.
- Lancefield Classification: Based on the carbohydrate composition of antigens found on the bacteria’s cell wall:
- Group A: Streptococcus pyogenes
- Group B: Streptococcus agalactiae
- Other groups include C, D (Enterococcus), F, and G.
- Additional Biochemical Tests:
- Bacitracin Sensitivity: S. pyogenes is sensitive, while S. agalactiae is resistant.
- Camp Test: S. agalactiae produces a zone of enhanced hemolysis when combined with S. aureus.
- Hippurate Hydrolysis: S. agalactiae is positive; S. pyogenes is negative.
Pathogenicity
- Virulence Factors:
- Toxins:
- Streptolysins (O and S): Lyse red and white blood cells, contributing to tissue damage and inflammation.
- Erythrogenic Toxin: Associated with scarlet fever.
- Enzymes:
- Hyaluronidase: Breaks down hyaluronic acid in connective tissues, aiding infection spread.
- Streptokinase: Converts plasminogen to plasmin, promoting the breakdown of blood clots.
- Adhesins: Promote attachment to host tissues, facilitating colonization.
- Toxins:
- Clinical Infections:
- Streptococcus pyogenes: Causes pharyngitis (strep throat), impetigo, cellulitis, and severe invasive infections (necrotizing fasciitis, toxic shock syndrome).
- Streptococcus agalactiae: Major cause of neonatal infections, including pneumonia and meningitis; also associated with infections in pregnant women.
- Streptococcus pneumoniae: Causes pneumonia, meningitis, and otitis media. It is known for its polysaccharide capsule, a major virulence factor.
- Enterococci (e.g., Enterococcus faecalis): Opportunistic pathogens that can cause urinary tract infections and endocarditis and are associated with antibiotic resistance.
Laboratory Diagnosis
1. Specimen Collection
Depends on the clinical condition:
-
Throat swab – Pharyngitis, tonsillitis
-
Sputum – Pneumonia
-
Blood – Septicemia, endocarditis
-
CSF – Meningitis
-
Pus / wound swab – Skin and soft tissue infections
Specimen should be collected aseptically and transported promptly.
2. Direct Microscopic Examination
-
Gram staining:
-
Gram-positive cocci
-
Arranged in chains or pairs
-
-
Presence of pus cells supports infection
Helps in presumptive diagnosis
3. Culture
-
Primary culture medium:
-
Blood agar (5% sheep blood)
-
-
Incubation:
-
37°C for 18–24 hours
-
Facultative anaerobic conditions
-
4. Hemolysis on Blood Agar
Important for preliminary identification:
| Type of Hemolysis | Appearance | Examples |
|---|---|---|
| Alpha (α) | Greenish partial hemolysis | S. pneumoniae, Viridans streptococci |
| Beta (β) | Clear complete hemolysis | S. pyogenes, S. agalactiae |
| Gamma (γ) | No hemolysis | Enterococci |
5. Catalase Test
-
Catalase negative → confirms Streptococci
-
Differentiates from Staphylococci (catalase positive)
6. Biochemical Tests (Important for MLT Exams)
For Beta-hemolytic Streptococci
-
Bacitracin sensitivity
-
Sensitive → Streptococcus pyogenes (Group A)
-
-
CAMP test
-
Positive → Streptococcus agalactiae (Group B)
-
-
PYR test
-
Positive → Group A streptococci
-
For Alpha-hemolytic Streptococci
-
Optochin sensitivity
-
Sensitive → Streptococcus pneumoniae
-
-
Bile solubility test
-
Positive → S. pneumoniae
-
For Enterococci
-
Bile esculin test – Positive
-
Growth in 6.5% NaCl – Positive
7. Serological Tests
Used mainly for post-streptococcal complications:
-
ASO (Antistreptolysin-O) test
-
Anti-DNase B test
Useful in diagnosing rheumatic fever and glomerulonephritis
8. Antigen Detection Tests
-
Rapid antigen detection tests (RADT) from throat swabs
-
Useful for quick diagnosis of Group A streptococcal pharyngitis
9. Molecular Methods (PG Level)
-
PCR-based assays
-
High sensitivity and specificity
-
Used in reference and research laboratories
10. Antibiotic Sensitivity Testing
-
Performed using Kirby–Bauer disk diffusion method
-
Guides appropriate antimicrobial therapy
-
Important due to emerging resistance
Antibiotic Resistance
Common Antibiotics Used Against Streptococci
-
Penicillin
-
Amoxicillin
-
Cephalosporins
-
Macrolides (Erythromycin, Azithromycin)
-
Tetracyclines
-
Vancomycin (for severe infections)
Antibiotic Resistance Pattern in Streptococci
1. Penicillin Resistance
-
Traditionally, Streptococci are penicillin-sensitive
-
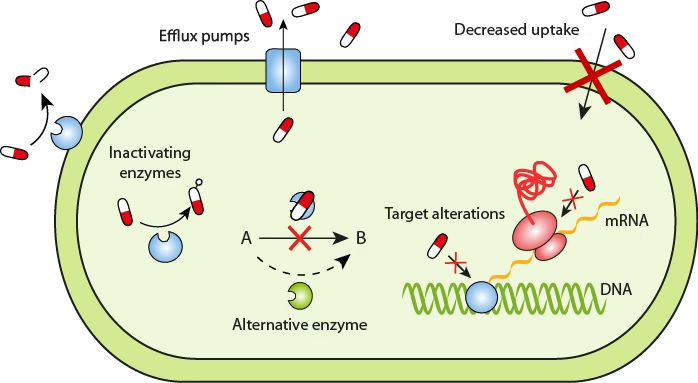
Resistance (especially in Streptococcus pneumoniae) occurs due to:
-
Alteration of Penicillin-Binding Proteins (PBPs)
-
-
Results in reduced binding of penicillin, not enzyme destruction
Important exam point:
Streptococci do not produce beta-lactamase
2. Macrolide Resistance (Erythromycin, Azithromycin)
Common in:
-
Streptococcus pyogenes
-
Streptococcus pneumoniae
Mechanisms:
-
Target site modification (methylation of ribosomal RNA)
-
Efflux pumps expelling antibiotic from the cell
3. Tetracycline Resistance
-
Occurs due to:
-
Efflux pumps
-
Ribosomal protection proteins
-
-
Commonly plasmid-mediated
4. Vancomycin Resistance
-
Rare in streptococci
-
More common in Enterococci
-
Resistance occurs due to:
-
Altered cell wall precursors
-