
Introduction
-
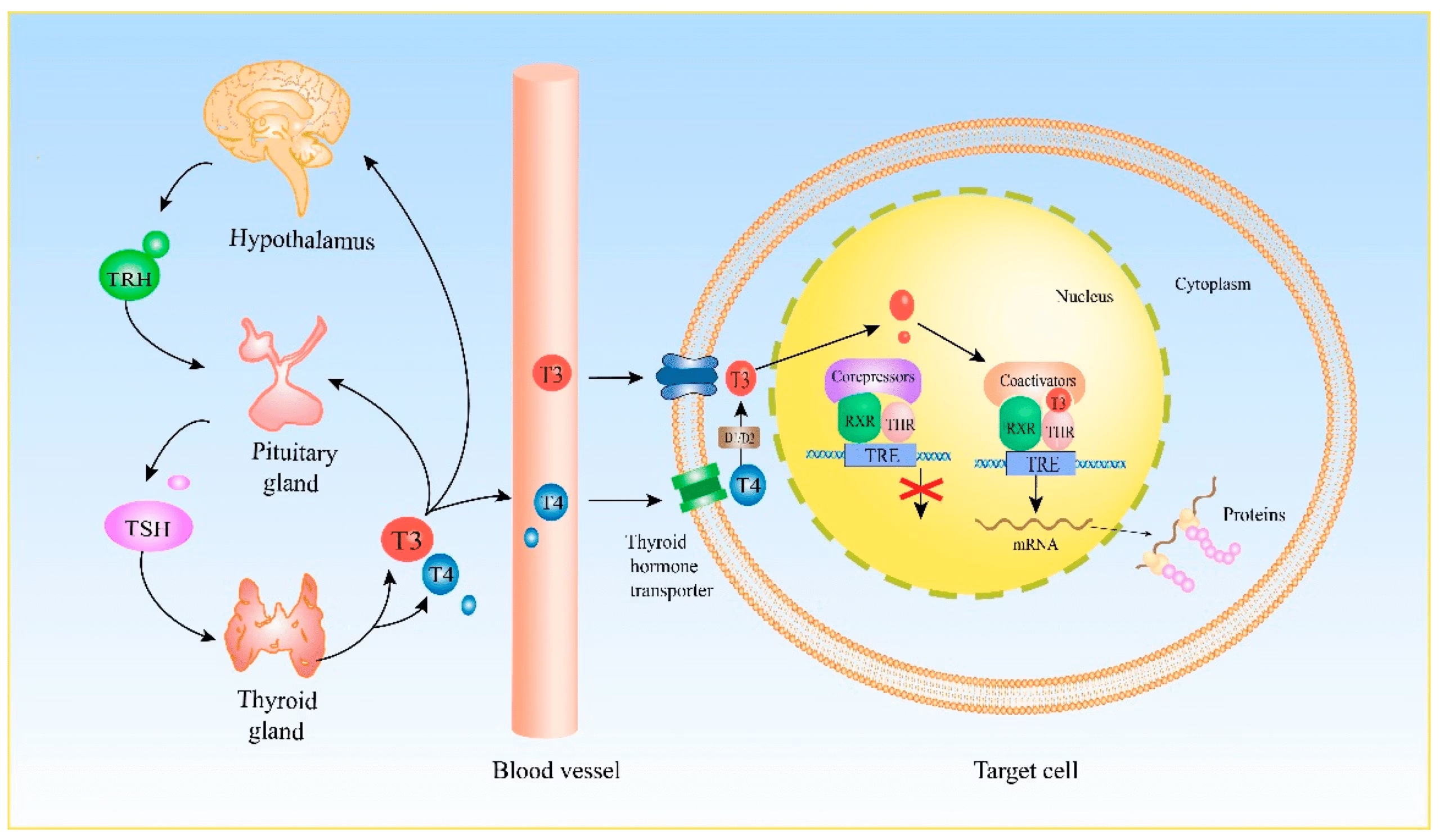
The thyroid gland plays a vital role in regulating metabolism, growth, and energy balance.
-
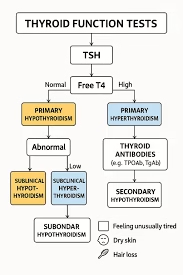
Thyroid Function Tests (TFTs) help evaluate how effectively the gland produces and manages thyroid hormones.
-
These tests assess hormone levels, feedback control, protein binding, and glandular activity.
-
They are essential for diagnosing hypothyroidism, hyperthyroidism, and autoimmune thyroid disorders.
-
TFTs also guide treatment decisions and help monitor therapy in thyroid patients.
-
Understanding key parameters like TSH, T3, T4, thyroglobulin, and binding indices is crucial for accurate diagnosis.
Thyroid-Stimulating Hormone
-
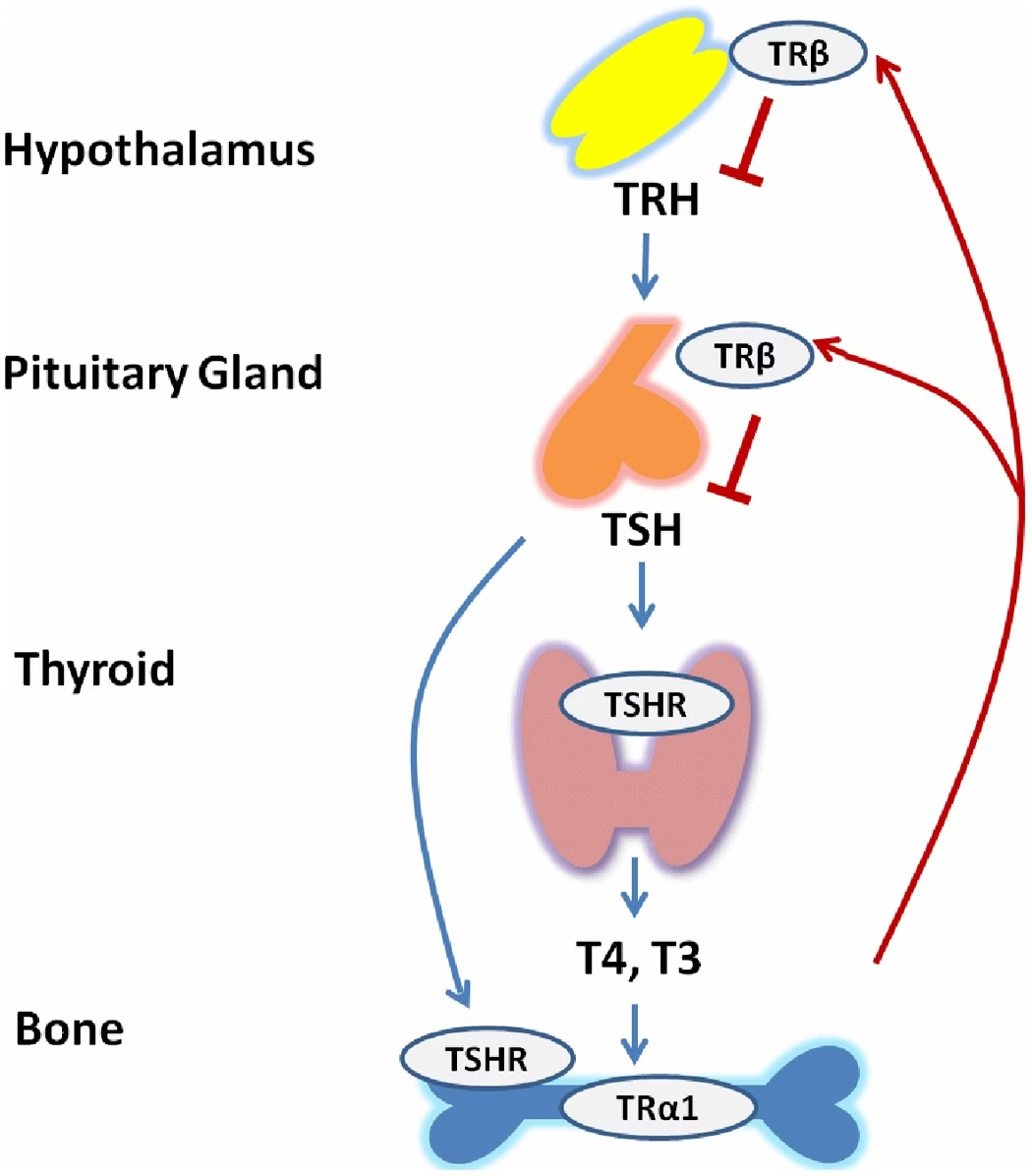
TSH is produced by the anterior pituitary gland.
-
It is the primary regulator of thyroid hormone production and release.
-
Even slight changes in thyroid hormone levels cause significant changes in TSH due to the sensitive negative-feedback mechanism.
-
High TSH usually indicates hypothyroidism, while low TSH indicates hyperthyroidism or thyroid hormone excess.
-
TSH is often considered the single most important initial test for thyroid assessment.
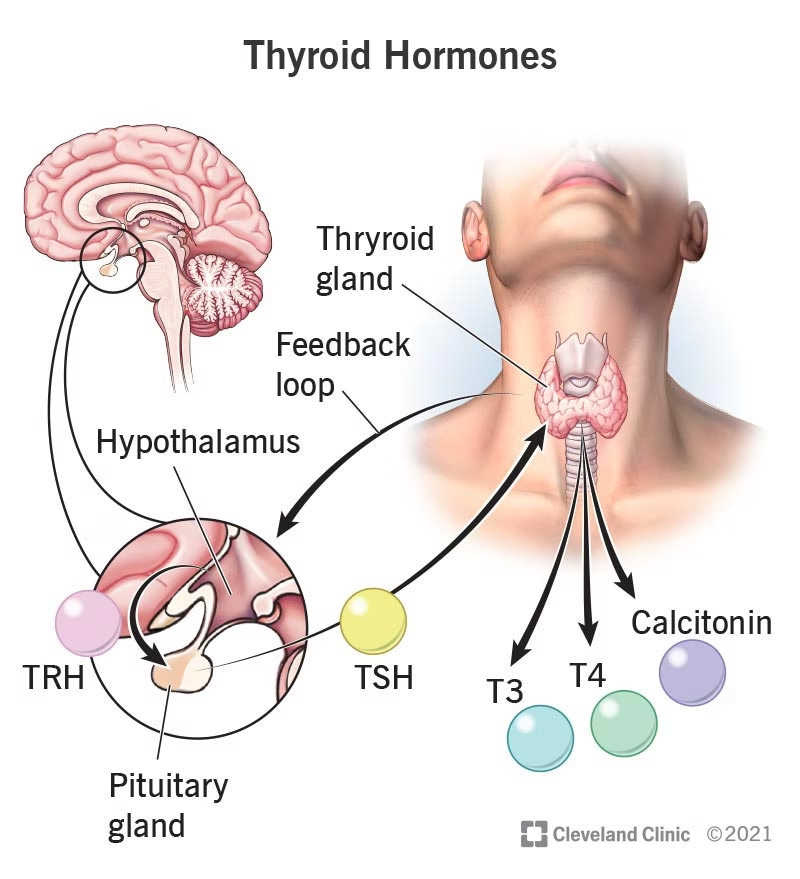
Thyroid Hormones
 Thyroxine (T4)
Thyroxine (T4)
-
Main hormone released by the thyroid gland.
-
Has a larger pool in circulation but lower potency.
-
Converts to T3 in peripheral tissues.
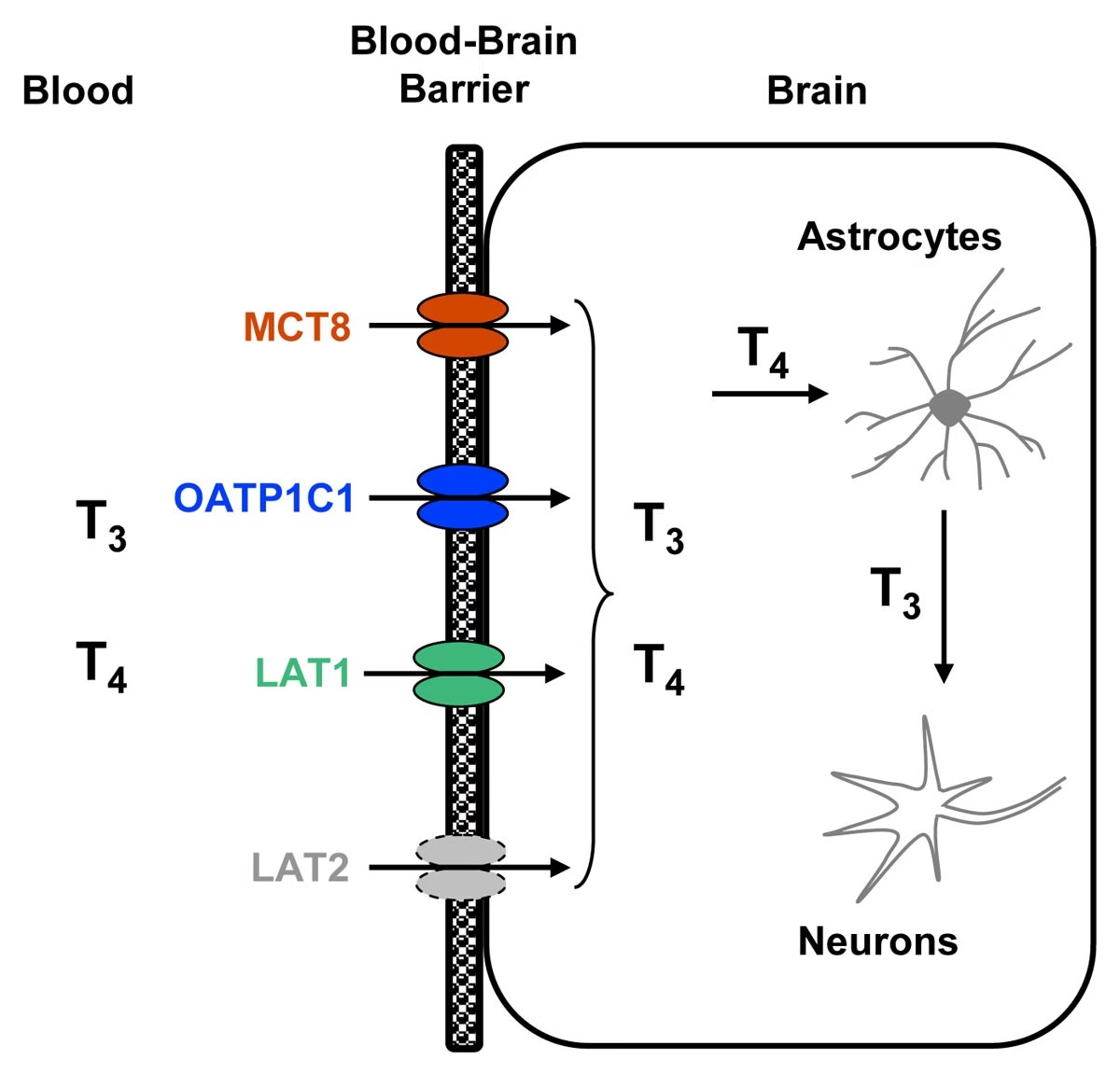
Triiodothyronine (T3)
-
More biologically active than T4.
-
Acts faster and has stronger metabolic effects.
-
Useful in diagnosing T3-toxicosis where T3 is elevated but T4 remains normal.
Free vs Total Forms
-
Free T3 and Free T4 are the physiologically active forms.
-
Total T3 and Total T4 change with protein levels in blood, so may not always reflect true thyroid status.
Difference Between T3 and T4
| Feature | T3 (Triiodothyronine) | T4 (Thyroxine) |
|---|---|---|
| Iodine Content | Contains 3 iodine atoms | Contains 4 iodine atoms |
| Biological Activity | More potent (3–4 times stronger) | Less potent |
| Amount Secreted by Thyroid | 20% secreted directly by thyroid | 80% secreted directly by thyroid |
| Source | Mostly formed by conversion of T4 to T3 in peripheral tissues | Primarily produced by the thyroid gland |
| Half-Life | Shorter (~1 day) | Longer (~7 days) |
| Protein Binding | Less protein-bound | Highly protein-bound |
| Circulating Levels | Low concentration in blood | High concentration in blood |
| Speed of Action | Faster action | Slower action |
| Physiological Role | Immediate metabolic effects, increases heat production and oxygen consumption | Acts as a hormone reservoir and precursor for T3 |
| Diagnostic Value | Important in diagnosing T3-toxicosis | Important for assessing overall thyroid hormone output |
| Stability in Blood | Less stable due to lower binding | More stable due to higher binding |
| Important Feature | Active hormone directly acting on tissues | Storage hormone providing steady supply for T3 formation |
Carrier Proteins
 Thyroid hormones travel in the bloodstream bound to specific proteins:
Thyroid hormones travel in the bloodstream bound to specific proteins:
-
Thyroxine-Binding Globulin (TBG) – main carrier
-
Transthyretin (Pre-albumin)
-
Albumin
Functions of carrier proteins:
-
Transport thyroid hormones in blood
-
Maintain a stable hormone reservoir
-
Regulate availability of free (active) hormone
Changes in these proteins affect total T3/T4 levels but usually do not change free hormone levels.
Protein Binding Function Tests
These tests evaluate how much thyroid hormone is bound to proteins and how much is free.
Key points:
-
Only free hormones are biologically active.
-
Changes in binding proteins can falsely elevate or lower total T4/T3.
-
Assessing binding helps identify:
-
Pregnancy-related changes
-
Liver disorders
-
Nephrotic syndrome
-
Drug-induced protein changes
-
These tests prevent misdiagnosis when total hormones appear abnormal due to altered protein levels.
Thyroid Tests
| Test | What It Measures | Clinical Use |
|---|---|---|
| TSH | Pituitary control of thyroid | First-line test |
| Free T4 | Active thyroxine | Hypo/Hyper diagnosis |
| Free T3 | Active triiodothyronine | Hyperthyroidism |
| Total T3/T4 | Hormone + protein-bound portion | Protein abnormalities |
| Anti-TPO / Anti-Tg / TRAb | Autoimmune markers | Hashimoto’s / Graves’ |
| Thyroglobulin | Thyroid tissue marker | Cancer follow-up |
| T3 Uptake / THBR | Protein binding | Binding abnormalities |
| FTI (Index) | Calculated free hormone | Corrected interpretation |
| RAIU | Iodine uptake | Hyperthyroid evaluation |
| Ultrasound | Thyroid structure | Goiter, nodules |
1. Thyroid-Stimulating Hormone (TSH)
Diagnostic Purpose
-
Primary screening test for thyroid disorders
-
Reflects pituitary response to circulating thyroid hormones
Clinical Significance
-
High TSH → Primary Hypothyroidism
-
Low TSH → Hyperthyroidism / thyroid hormone excess
-
Very sensitive to even minor changes in T3/T4
Reference Range
-
Adults: 0.4 – 4.0 mIU/L
-
Pregnancy 1st trimester: 0.1 – 2.5 mIU/L
Method
-
CLIA (Chemiluminescence Immunoassay)
-
ECLIA (Electrochemiluminescence)
-
ELISA
2. Free T4 (FT4)
Diagnostic Purpose
-
Measures biologically active thyroxine
-
Best indicator of thyroid hormone status
Clinical Significance
-
Low FT4: Hypothyroidism
-
High FT4: Hyperthyroidism, Graves’ disease
Reference Range
-
0.8 – 2.0 ng/dL
Method
-
CLIA
-
ECLIA
-
RIA (older)
3. Total T4 (TT4)
Diagnostic Purpose
-
Measures hormone bound to proteins + free hormone
Clinical Significance
-
Elevated in pregnancy (↑TBG)
-
Low in protein deficiency states
-
Useful when free hormone tests are unreliable
Reference Range
-
5.0 – 12.0 µg/dL
Method
-
Competitive immunoassays
-
CLIA, ELISA
4. Free T3 (FT3)
Diagnostic Purpose
-
Measures unbound, active T3
-
Important in hyperthyroidism
Clinical Significance
-
High FT3: T3-toxicosis, early hyperthyroidism
-
Low in severe illness
Reference Range
-
2.3 – 4.2 pg/mL
Method
-
CLIA / ECLIA
-
ELISA
5. Total T3 (TT3)
Diagnostic Purpose
-
Measures both bound + free T3
Clinical Significance
-
Changes with protein-binding alterations
-
Elevated in hyperthyroidism
Reference Range
-
80 – 180 ng/dL
Method
-
Competitive immunoassays (CLIA / ELISA)
6. Thyroid Antibody Tests
A. Anti-TPO Antibody
Purpose
-
Detects autoimmune destruction of thyroid
Clinical Significance
-
High in Hashimoto’s thyroiditis
-
High in Graves’ disease
Reference Range
-
< 35 IU/mL (positive if elevated)
Method
-
ELISA, CLIA, ECLIA
B. Anti-Thyroglobulin (Anti-Tg)
Purpose
-
Detects antibodies against thyroglobulin
Clinical Significance
-
Hashimoto’s thyroiditis
-
Thyroid cancer follow-up
Reference Range
-
< 40 IU/mL
Method
-
CLIA / ELISA
C. TSH-Receptor Antibodies (TRAb / TSI)
Purpose
-
Detects antibodies stimulating TSH receptor
Clinical Significance
-
Diagnostic test for Graves’ disease
Reference Range
-
< 1.75 IU/L
Method
-
ECLIA
-
Bioassays
7. Thyroglobulin (Tg)
Diagnostic Purpose
-
Protein precursor for thyroid hormone synthesis
-
Marker for thyroid cancer recurrence
Clinical Significance
-
High after thyroid damage, inflammation or cancer
-
Used to monitor thyroidectomy patients
Reference Range
-
Men: 1.4 – 29 ng/mL
-
Women: 1.5 – 38 ng/mL
Method
-
Immunoassays (CLIA / ECLIA)
-
Mass spectrometry (in specialized labs)
8. Reverse T3 (rT3)
Purpose
-
Inactive form of T3
-
Assesses metabolic dysfunction
Clinical Significance
-
High in Euthyroid Sick Syndrome
-
Used in critical care evaluations
Reference Range
-
10 – 24 ng/dL
Method
-
LC-MS/MS (Highly accurate)
-
RIA
9. T3 Uptake (T3U) / Thyroid Hormone Binding Ratio
Diagnostic Purpose
-
Measures availability of binding sites on TBG
Clinical Significance
-
High T3U: Low TBG (liver disease, androgens)
-
Low T3U: High TBG (pregnancy, estrogen therapy)
Reference Range
-
25 – 35%
Method
-
Competitive binding tests
-
RIA / CLIA
10. Free T4 Index (FTI)
Diagnosis
-
Calculated: FTI = Total T4 × T3 Uptake
Clinical Significance
-
Used when protein abnormalities alter total T4
-
Reliable substitute when free assays interfere
Reference Range
-
4.5 – 12.0 μg/dL
Method
-
Calculated parameter based on lab values
11. Serum TBG (Thyroxine-Binding Globulin)
Diagnostic Purpose
-
Measures concentration of main binding protein
Clinical Significance
-
High TBG → Pregnancy, estrogen therapy
-
Low TBG → Malnutrition, nephrotic syndrome
Reference Range
-
13 – 30 mg/L
Method
-
Immunoassays (CLIA / ELISA)
12. Calcitonin
Diagnostic Purpose
-
Hormone secreted by thyroid C-cells
Clinical Significance
-
High in Medullary Thyroid Carcinoma (MTC)
-
Used in screening of MEN syndrome
Reference Range
-
Men < 10 pg/mL
-
Women < 5 pg/mL
Method
-
ECLIA
-
CLIA
13. Radioactive Iodine Uptake (RAIU)
Diagnostic Purpose
-
Assesses iodine absorption by thyroid
Clinical Significance
-
High uptake → Graves’ disease, toxic nodular goiter
-
Low uptake → Thyroiditis, iodine overload
Reference Range
-
6-hour uptake: 5–15%
-
24-hour uptake: 10–30%
Method
-
Nuclear medicine scan
-
Using I-123 or I-131 isotopes
14. Thyroid Scan (Nuclear Imaging)
Purpose
-
Visualization of thyroid structure and function
Clinical Significance
-
Detects hot/cold nodules
-
Evaluates cancer spread
-
Differentiates Graves’ disease from thyroiditis
Method
-
Gamma camera imaging with radioactive iodine
15. Thyroid Ultrasound
Purpose
-
Structural imaging of thyroid gland
Clinical Significance
-
Detects nodules, cysts, goiter, thyroiditis
-
Guides FNA biopsy
Method
-
High-resolution ultrasonography
16. Fine Needle Aspiration (FNA)
Diagnostic Purpose
-
Cytological evaluation of thyroid nodules
Clinical Significance
-
Gold standard for diagnosing:
-
Papillary carcinoma
-
Follicular neoplasm
-
Benign nodules
-
Thyroiditis
-
Method
-
Ultrasound-guided aspiration
-
Cytology smear evaluation
Mixed Parameters
Mixed parameters combine two or more thyroid-related measurements to improve diagnostic accuracy.
Examples:
-
Free hormones + TSH together
-
Total T4 + binding index
-
T3 uptake + T4 levels
They help in:
-
Distinguishing true thyroid disease from protein-binding abnormalities
-
Providing a broader clinical interpretation
-
Understanding “intermediate” thyroid states
Mixed parameters are especially helpful when results are borderline or conflicting.
Calculated and Structural Parameters
These are derived or mathematically adjusted values that provide deeper insights into thyroid physiology.
Common Calculated Parameters
-
Free T4 Index (FTI) – combines total T4 and T3 uptake
-
Free T3 Index (FT3I)
-
Thyroid Hormone Binding Ratio (THBR)
-
Corrected values when free hormone assays are not available
Structural / Functional Indicators
-
Reflect thyroid gland reserve and activity
-
Help assess:
-
Thyroid gland stimulating capacity
-
Peripheral conversion of T4 to T3
-
Degree of hormone saturation on binding proteins
-
Calculated parameters are essential when standard free hormone assays show interference or when binding-protein abnormalities are suspected.
Clinical Significance of Thyroid Function Tests
Thyroid Function Tests (TFTs) provide essential information about the functional, biochemical, and regulatory status of the thyroid gland. Their overall clinical significance includes:
1. Diagnosis of Thyroid Disorders
TFTs are the primary tool for diagnosing:
-
Hypothyroidism (primary, secondary, subclinical)
-
Hyperthyroidism (overt & subclinical)
-
Thyroiditis (Hashimoto’s, painless, postpartum)
-
Autoimmune thyroid diseases (via antibody testing)
They help differentiate between disorders originating from the thyroid gland vs. the pituitary gland.
2. Assessment of Thyroid Hormone Levels in the Body
TFTs show how much active or inactive hormone is available, helping confirm:
-
Hormone deficiency
-
Hormone excess
-
Abnormal conversion of T4 → T3
-
Altered hormone binding due to protein abnormalities
This provides insight into actual metabolic hormone activity in tissues.
3. Evaluation of Pituitary–Thyroid Axis
TSH reflects the brain’s response to circulating thyroid hormones.
TFTs help understand:
-
Whether the pituitary gland is responding correctly
-
Feedback regulation
-
Disorders like secondary or tertiary hypothyroidism
This distinguishes central causes from thyroid gland dysfunction.
4. Monitoring of Thyroid Treatment
TFTs are essential in guiding therapy:
-
Adjusting levothyroxine dose in hypothyroid patients
-
Monitoring antithyroid drugs in hyperthyroidism
-
Evaluating response after radioactive iodine therapy
-
Assessing stability during pregnancy
They ensure proper hormone balance is maintained.
5. Detection of Autoimmune Thyroid Conditions
Antibody tests (Anti-TPO, Anti-Tg, TRAb) help:
-
Confirm autoimmune thyroiditis
-
Diagnose Graves’ disease
-
Predict risk of future thyroid dysfunction
-
Monitor remission or relapse
Autoimmunity is the most common cause of thyroid disease.
6. Evaluation of Thyroid Nodules and Cancer
Certain TFT parameters support cancer diagnosis and follow-up:
-
Thyroglobulin – tumor marker for papillary & follicular cancer
-
Calcitonin – marker for medullary thyroid carcinoma
-
Imaging tests support structural evaluation
They help detect recurrence and guide long-term management.
7. Assessment of Binding Protein Abnormalities
Tests like Total T3/T4, T3 Uptake, TBG levels, and FTI help identify:
-
Changes in thyroid hormone–binding proteins
-
Conditions like pregnancy, liver disease, nephrotic syndrome, malnutrition
-
Whether total hormone levels truly reflect thyroid status
This prevents misinterpretation due to protein disorders.
8. Differentiation of Thyrotoxicosis Causes
RAIU and thyroid scans differentiate:
-
Graves’ disease
-
Toxic nodules
-
Thyroiditis
-
Iodine-induced thyrotoxicosis
Correct diagnosis ensures appropriate treatment.
9. Evaluation During Critical Illness
TFTs help detect:
-
Euthyroid Sick Syndrome
-
Altered hormone metabolism under stress, starvation, trauma, sepsis
This prevents unnecessary thyroid treatment during severe illness.
10. Support in Pregnancy and Fertility Management
Pregnancy significantly alters thyroid physiology. TFTs help:
-
Manage maternal hypothyroidism (important for fetal brain development)
-
Diagnose hyperthyroidism
-
Monitor TSH/FT4 trimester-specific ranges
-
Evaluate recurrent miscarriages related to thyroid autoimmunity
TFTs protect both maternal and fetal health.
MCQs
1. Which hormone is most commonly measured to assess primary thyroid function?
A. T3
B. T4
C. TSH
D. TRH
2. The biologically active form of thyroid hormone is:
A. Total T4
B. Total T3
C. Free T4
D. Reverse T3
3. Elevated TSH with low T4 indicates:
A. Primary hyperthyroidism
B. Primary hypothyroidism
C. Secondary hyperthyroidism
D. Euthyroid state
4. Low TSH and low T4 suggest:
A. Primary hypothyroidism
B. Secondary hypothyroidism
C. Hashimoto’s thyroiditis
D. Graves’ disease
5. Excess production of thyroid hormone is best indicated by:
A. High TSH
B. Low TSH
C. High TRH
D. High prolactin
6. Free T3 is most useful for diagnosing:
A. Subclinical hypothyroidism
B. Early hyperthyroidism
C. Euthyroid sick syndrome
D. Normal thyroid function
7. Which test detects autoimmune thyroid disease?
A. TSH
B. Free T4
C. Anti-TPO antibodies
D. Thyroglobulin
8. Anti-TPO antibody is strongly associated with:
A. Graves’ disease
B. Hashimoto’s thyroiditis
C. Subacute thyroiditis
D. Goiter
9. Elevated T3 with normal T4 and low TSH suggests:
A. T4 toxicosis
B. T3 toxicosis
C. Hypothyroidism
D. Euthyroid sick syndrome
10. Which is the most sensitive test for early thyroid dysfunction?
A. Free T4
B. Total T4
C. TSH
D. Thyroglobulin
11. Thyroglobulin is mainly used for monitoring:
A. Graves’ disease
B. Thyroid cancer recurrence
C. Hypothyroidism treatment
D. Pituitary function
12. A high TSH and normal T4 indicate:
A. Overt hypothyroidism
B. Subclinical hypothyroidism
C. Hyperthyroidism
D. Thyroid storm
13. Low TSH and normal T4 indicate:
A. Subclinical hyperthyroidism
B. Overt hypothyroidism
C. Overt hyperthyroidism
D. Thyroiditis
14. Which test differentiates Graves’ disease from thyroiditis?
A. TSH
B. T3
C. T4
D. TSH receptor antibodies (TRAb)
15. Reverse T3 is elevated in:
A. Hyperthyroidism
B. Euthyroid sick syndrome
C. Primary hypothyroidism
D. Hashimoto’s disease
16. Thyroid-stimulating immunoglobulin (TSI) indicates:
A. Hashimoto’s
B. Graves’ disease
C. Goiter
D. Hypothyroidism
17. A patient with high free T4 and high TSH likely has:
A. Pituitary adenoma
B. Thyroid storm
C. Hashimoto’s
D. Euthyroid state
18. Which hormone provides negative feedback to TSH?
A. TRH
B. Free T4
C. Prolactin
D. ACTH
19. TSH reference range in adults is approximately:
A. 0.4–4.0 mIU/L
B. 5–10 mIU/L
C. 10–20 mIU/L
D. 20–30 mIU/L
20. A low TSH but normal T3 and T4 may occur after:
A. Pregnancy
B. Severe illness
C. Hypothyroidism
D. Pituitary hyperfunction
21. Total T4 levels depend mainly on:
A. Liver function
B. TSH secretion
C. Thyroxine-binding globulin
D. Iodine levels
22. Pregnancy increases:
A. Free T4
B. Free T3
C. TBG
D. TRH
23. In primary hyperthyroidism, free T4 levels are:
A. Low
B. Normal
C. High
D. Variable
24. The best test to monitor levothyroxine therapy is:
A. Total T3
B. Free T4
C. TSH
D. Anti-TPO
25. Thyroid peroxidase is essential for:
A. TSH secretion
B. Iodine trapping
C. Thyroid hormone synthesis
D. TBG production
26. In Hashimoto’s, TSH is typically:
A. Low
B. Normal
C. High
D. Extremely low
27. TSH receptor antibodies stimulate thyroid hormone release in:
A. Thyroiditis
B. Hashimoto’s
C. Graves’ disease
D. Endemic goiter
28. Which parameter decreases in euthyroid sick syndrome?
A. Free T4
B. Total T3
C. TSH
D. TBG
29. Thyroid-binding globulin (TBG) levels increase in:
A. Liver failure
B. Nephrotic syndrome
C. Pregnancy
D. Hyperthyroidism
30. A patient taking amiodarone may have elevated:
A. TSH
B. TBG
C. Reverse T3
D. TSI
31. TRH stimulates release of:
A. T3
B. T4
C. TSH
D. TBG
32. TSH levels are lowest in:
A. Morning
B. Afternoon
C. Midnight
D. Early morning (2–4 AM)
33. Thyroid storm typically shows:
A. High TSH
B. Extremely high T4 and T3
C. High TRH
D. Low reverse T3
34. Anti-thyroglobulin antibodies interfere with measurement of:
A. TSH
B. Thyroglobulin
C. Free T4
D. TBG
35. The first-line test in newborn thyroid screening is:
A. T4
B. T3
C. TSH
D. TRH
36. Low free T4 with normal TSH suggests:
A. Central hypothyroidism
B. Subclinical hypothyroidism
C. Hyperthyroidism
D. Euthyroid state
37. TSH levels rise when:
A. T4 increases
B. T4 decreases
C. TRH decreases
D. Iodine increases
38. A radioactive iodine uptake (RAIU) test is used to evaluate:
A. TSI levels
B. Thyroid autoantibodies
C. Thyroid function and hyperthyroidism
D. Thyroid cancer staging
39. Which TFT abnormality is seen in Graves’ disease?
A. High TSH
B. Low T4
C. High free T4, low TSH
D. Low TRAb
40. Which test is least influenced by binding protein abnormalities?
A. Total T4
B. Total T3
C. Free T4
D. Total rT3
✅ Answer Key
-
C
-
C
-
B
-
B
-
B
-
B
-
C
-
B
-
B
-
C
-
B
-
B
-
A
-
D
-
B
-
B
-
A
-
B
-
A
-
B
-
C
-
C
-
C
-
C
-
C
-
C
-
C
-
B
-
C
-
C
-
C
-
C
-
B
-
B
-
C
-
A
-
B
-
C
-
C
-
C