Introduction
-
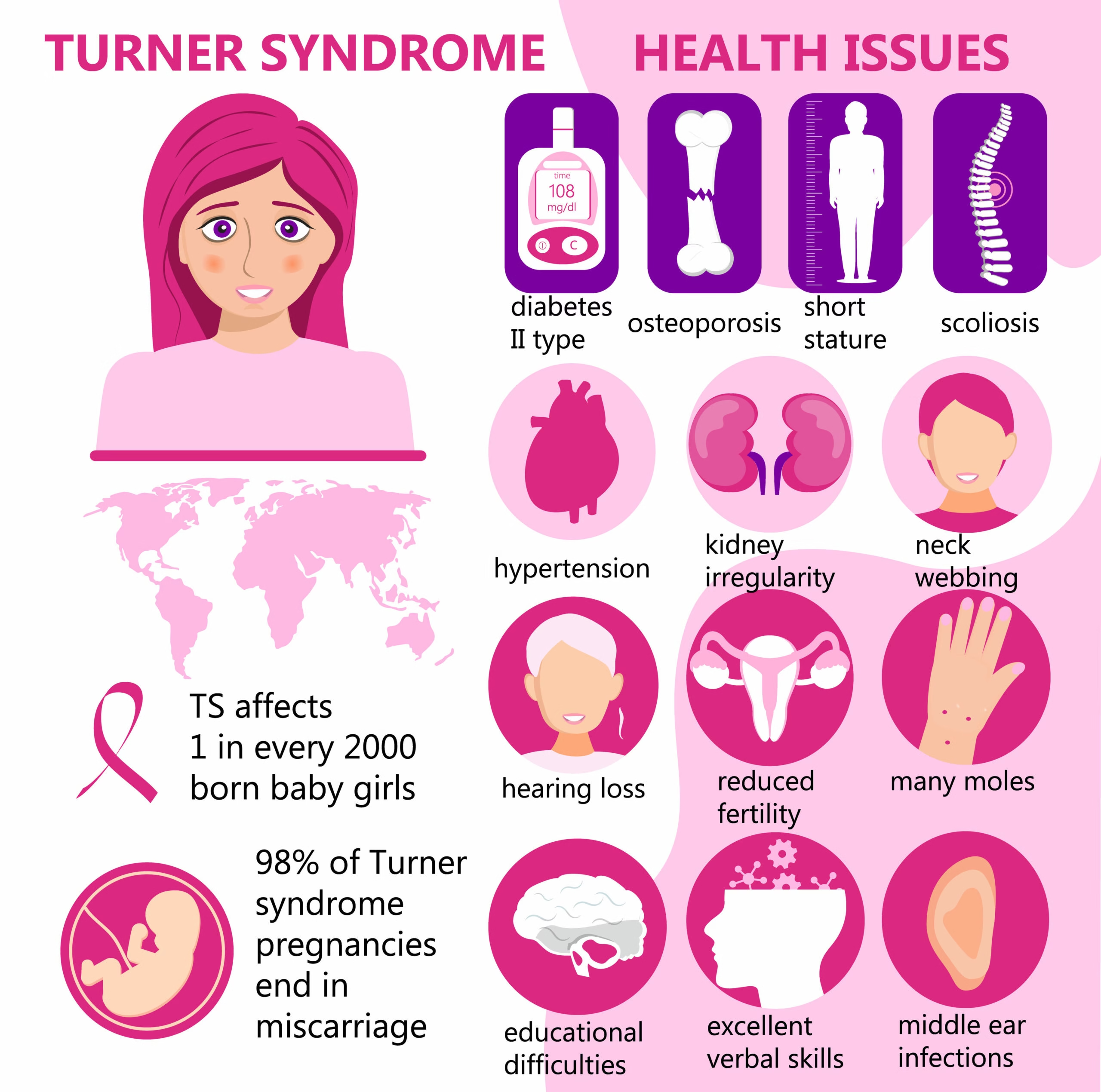
Turner’s Syndrome is a genetic condition that affects only females.
-
It occurs when one X chromosome is missing or partially missing.
-
This chromosomal abnormality affects growth, puberty, fertility, and multiple organs such as the heart, kidneys, and thyroid.
-
The condition is present from birth, though signs may appear at infancy, childhood, or adolescence.
-
Turner’s Syndrome happens randomly during cell division and is not caused by anything parents did.
-
With early diagnosis and proper medical care, most girls and women with Turner’s Syndrome can lead normal, healthy, and productive lives.
- First described by Dr. Henry Turner in 1938, it remains one of the most common chromosomal disorders, affecting approximately 1 in 2,000–2,500 live female births.
What Is Turner’s Syndrome?
Turner’s Syndrome (also known as Monosomy X) is a chromosomal abnormality where a female is born with:
-
One missing X chromosome (45,X)
-
Or a structurally altered X chromosome
-
Or mosaicism (some cells are normal, others are missing an X)
Because the X chromosome carries important genes for growth, sexual development, and organ functioning, the condition leads to a characteristic set of physical and medical problems.
Types
Understanding the genetic variations helps explain the differences in symptoms and severity.
1. Classic Monosomy X (45,X)
-
Complete loss of one X chromosome in all cells
-
Most severe form
-
Occurs in about 50% of cases
2. Mosaic Turner’s Syndrome (45,X/46,XX or others)
-
Some cells have monosomy X, others are normal
-
Milder symptoms; some women may menstruate or conceive
3. Structural Abnormalities of X Chromosome
-
Isochromosomes
-
Ring chromosomes
-
Deletions
These cause variable clinical features depending on which part of the chromosome is missing.
Causes
Turner’s Syndrome is not inherited in the vast majority of cases.
It occurs due to random nondisjunction, meaning:
-
There is an error during the formation of reproductive cells (sperm or egg).
-
One X chromosome fails to copy or separates incorrectly.
Key Point: Nothing the mother or father did causes Turner’s Syndrome.
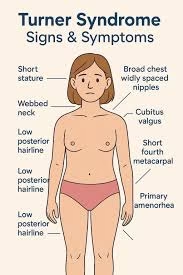
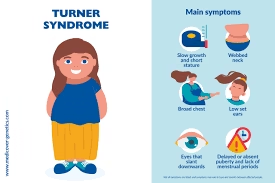
Characteristic Features and Symptoms
Symptoms vary depending on the type and severity of chromosomal alteration.
Physical Features
-
Short stature (most common)
-
Webbed neck
-
Low hairline at the back of the head
-
Broad chest with widely spaced nipples
-
High-arched palate
-
Short 4th metacarpal
-
Lymphedema of hands and feet in newborns
-
Low-set ears
-
Narrow, upturned fingernails
Medical Problems and Organ Involvement
1. Cardiovascular Abnormalities
-
Coarctation of aorta
-
Bicuspid aortic valve
-
Hypertension
-
Risk of aortic dissection (important in adults)
2. Endocrine and Metabolic Issues
-
Hypothyroidism (often autoimmune)
-
Diabetes mellitus risk
-
Obesity tendency
-
Hyperlipidemia
3. Gonadal Dysgenesis
-
Streak ovaries
-
Ovarian failure
-
Absent or delayed puberty
-
Infertility
-
No menarche or irregular menses
4. Renal Abnormalities
-
Horseshoe kidney
-
Duplex collecting system
-
Increased risk of UTIs and hypertension
5. Skeletal Problems
-
Scoliosis
-
Osteoporosis due to estrogen deficiency
6. Ear and Hearing Problems
-
Recurrent otitis media in childhood
-
Sensorineural hearing loss in adulthood
7. Eye Problems
-
Strabismus
-
Ptosis
-
Refractive errors
8. Learning and Cognitive Profile
Most girls have normal intelligence, but may show:
-
Difficulty with spatial reasoning
-
Math difficulties
-
Non-verbal learning disability
-
Social anxiety
Diagnosis
1. Prenatal Diagnosis
-
Ultrasound findings: Cystic hygroma, fetal edema, congenital heart defect
-
Non-invasive prenatal testing (NIPT)
-
Chorionic villus sampling (CVS)
-
Amniocentesis
2. Postnatal Diagnosis
-
Short stature
-
Delayed puberty
-
Lymphedema
-
Cardiac anomalies
3. Confirmatory Test
🧬 Karyotyping is the gold standard.
It detects:
-
Monosomy X
-
Mosaicism
-
Structural abnormalities
Other tests:
-
FISH
-
Microarray
Treatment and Management
There is no cure, but early intervention helps ensure normal development and quality of life.
1. Growth Hormone Therapy
-
Started in early childhood
-
Increases adult height by 5–10 cm
-
Safe and widely recommended
2. Estrogen Replacement Therapy (ERT)
-
Begins around age 11–12
-
Induces puberty
-
Helps in bone development
-
Improves cardiovascular and metabolic health
3. Progesterone Therapy
-
Started after 1–2 years of estrogen treatment
-
Establishes menstrual cycles
4. Management of Infertility
Although most women are infertile, options include:
-
IVF with donor eggs
-
Cryopreservation (for those with mosaicism and residual ovarian function)
-
Gestational surrogacy
-
Strict cardiac evaluation before pregnancy due to high maternal risk
5. Cardiac Monitoring
-
Regular echocardiography
-
MRI of aorta
-
Blood pressure monitoring
6. Renal and Urinary System Care
-
Renal ultrasound
-
Monitoring hypertension
7. Hearing and ENT Evaluation
-
Yearly audiology tests
-
Early treatment for ear infections
8. Psychological and Behavioral Support
-
Counseling for social and emotional difficulties
-
Educational support for math or spatial learning difficulties
Complications Associated with Turner’s Syndrome
-
Infertility
-
Aortic dissection (life-threatening)
-
Osteoporosis
-
Hearing impairment
-
Hypertension and cardiovascular disease
-
Thyroid disorders
-
Obesity and diabetes
-
Psychosocial challenges
MCQs
1. Turner’s Syndrome is caused by:
A. Trisomy 21
B. Monosomy X
C. Trisomy 18
D. Triploidy
2. The most common karyotype in Turner’s Syndrome is:
A. 47,XXX
B. 45,X
C. 45,X/46,XY
D. 46,XX
3. Turner’s Syndrome affects which sex?
A. Male only
B. Female only
C. Both sexes
D. Neither
4. A newborn girl with puffy hands and feet most likely has:
A. Down syndrome
B. Turner’s syndrome
C. Patau syndrome
D. Edwards syndrome
5. Short stature in Turner’s syndrome is mainly due to deficiency of:
A. PTH gene
B. SHOX gene
C. FMR1 gene
D. SRY gene
6. The ovarian morphology typically seen in Turner’s Syndrome is:
A. Polycystic ovaries
B. Streak ovaries
C. Hyperplastic ovaries
D. Normal ovaries
7. The most common cardiac defect in Turner’s syndrome is:
A. Tetralogy of Fallot
B. Transposition
C. Bicuspid aortic valve
D. Atrial septal defect
8. A classic physical feature of Turner’s syndrome is:
A. Webbed neck
B. Simian crease
C. Brushfield spots
D. Microcephaly
9. Primary amenorrhea with normal pubic hair but absent breasts suggests:
A. Turner’s syndrome
B. Müllerian agenesis
C. PCOS
D. Kallmann syndrome
10. Girls with Turner’s syndrome typically have:
A. Tall stature
B. Short stature
C. Obesity always
D. Macroglossia
11. Which hormone is elevated in Turner’s Syndrome?
A. FSH
B. Estrogen
C. Progesterone
D. Testosterone
12. Most cases of Turner’s Syndrome arise due to errors in:
A. Meiosis
B. Mitosis
C. DNA repair
D. Transcription
13. Common renal anomaly seen in Turner’s Syndrome:
A. Horseshoe kidney
B. Polycystic kidney
C. Renal agenesis
D. Hydronephrosis only
14. Which diagnostic test is the gold standard?
A. Ultrasound
B. Karyotype analysis
C. FISH
D. NIPT
15. Turner’s Syndrome is associated with increased risk of:
A. Hypothyroidism
B. Hyperthyroidism
C. Cushing syndrome
D. Acromegaly
16. Hearing issues in Turner’s Syndrome are due to:
A. Sensorineural loss
B. Conductive loss
C. Both A and B
D. Central auditory loss
17. Intelligence in Turner’s Syndrome is usually:
A. Severely impaired
B. Normal
C. Borderline
D. Always low
18. Growth hormone therapy is started to improve:
A. Puberty onset
B. Height
C. Fertility
D. Cardiac function
19. Estrogen therapy should ideally start at:
A. 1–2 years
B. 5 years
C. 11–12 years
D. At menopause
20. Progesterone therapy is added after estrogen to:
A. Stop menstruation
B. Induce ovulation
C. Protect the endometrium
D. Treat acne
21. Spontaneous puberty is more common in:
A. Classic 45,X
B. Mosaic 45,X/46,XX
C. Ring chromosome
D. Isochromosome
22. Turner’s Syndrome increases risk of which metabolic disorder?
A. Addison disease
B. Diabetes mellitus
C. Nephrotic syndrome
D. Wilson disease
23. Which prenatal finding suggests Turner’s Syndrome?
A. Omphalocele
B. Cystic hygroma
C. Holoprosencephaly
D. Polydactyly
24. Most common cause of death in adults with Turner’s Syndrome:
A. Infection
B. Aortic dissection
C. Cancer
D. Renal failure
25. Turner’s Syndrome patients commonly have:
A. Normal uterus
B. Absent uterus
C. Rudimentary uterus
D. Double uterus
26. A typical lab finding in Turner’s Syndrome:
A. High estrogen
B. Low FSH
C. High FSH and LH
D. Low prolactin
27. The genetic condition is:
A. Always inherited
B. Sporadic, due to nondisjunction
C. Autosomal dominant
D. Autosomal recessive
28. Turner’s Syndrome is associated with which orthopedic condition?
A. Scoliosis
B. Genu varum
C. Hip dysplasia
D. Osteopetrosis
29. The neck webbing in Turner’s syndrome is due to:
A. Lymphatic obstruction
B. Muscle hypertrophy
C. Bone fusion
D. Neural tube defect
30. Pigmented nevi are:
A. Absent
B. Common
C. Diagnostic
D. Cancerous in 90%
31. Which chromosome is involved?
A. Chromosome 13
B. X chromosome
C. Y chromosome
D. Chromosome 21
32. Turner’s Syndrome can be detected in pregnancy via:
A. MRI
B. NIPT
C. Endoscopy
D. X-ray
33. Patients typically have which blood pressure pattern?
A. Low BP
B. Normal always
C. Hypertension risk
D. Shock
34. Turner’s Syndrome has increased risk of:
A. Osteoporosis
B. Hypercalcemia
C. Gout
D. Megaloblastic anemia
35. Which feature differentiates Turner’s from androgen insensitivity syndrome?
A. Short stature
B. Primary amenorrhea
C. Breast development
D. Female phenotype
36. Turner’s patients have:
A. Absence of pubic hair
B. Normal pubic hair
C. Excess pubic hair
D. Male pattern hair
37. Which screening is essential yearly?
A. Dental X-ray
B. Aortic imaging
C. EEG
D. Liver biopsy
38. Most Turner’s Syndrome individuals are:
A. Fertile naturally
B. Infertile
C. Fertile only at puberty
D. Fertile after GH therapy
39. Best fertility option for Turner’s Syndrome:
A. Natural conception
B. IVF with donor oocytes
C. Surrogate pregnancy only
D. No option exists
40. Which IQ domain is usually affected?
A. Verbal IQ
B. Spatial IQ
C. Writing skills
D. Memory
Answer Key
1-B
2-B
3-B
4-B
5-B
6-B
7-C
8-A
9-A
10-B
11-A
12-A
13-A
14-B
15-A
16-C
17-B
18-B
19-C
20-C
21-B
22-B
23-B
24-B
25-A
26-C
27-B
28-A
29-A
30-B
31-B
32-B
33-C
34-A
35-A
36-B
37-B
38-B
39-B
40-B