Introduction
-
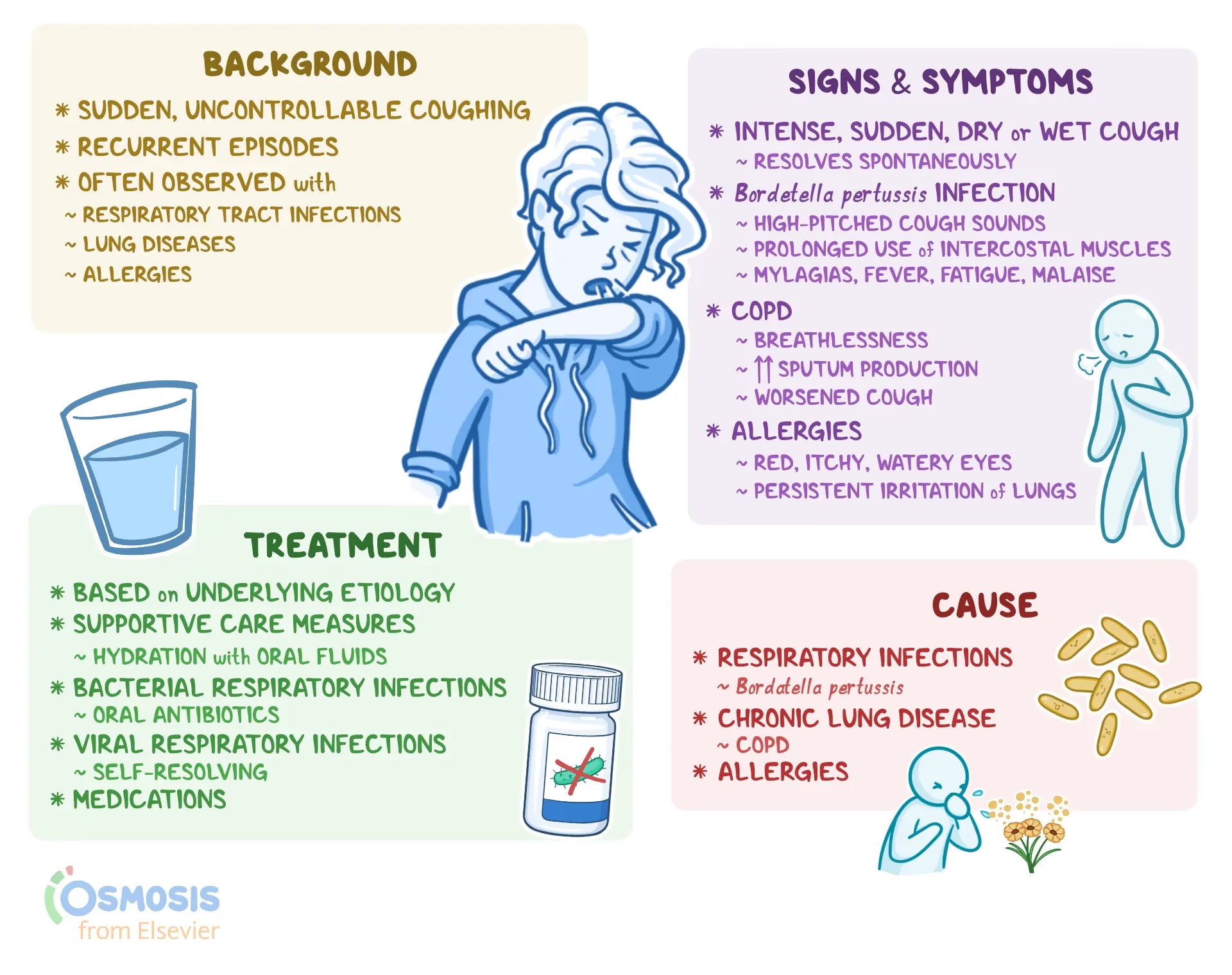
Whooping cough, also known as pertussis, is an acute and highly contagious bacterial infection.
-
It primarily affects the respiratory tract.
-
The disease is characterized by prolonged, severe bouts of coughing.
-
Each coughing episode is often followed by a high-pitched inspiratory “whoop”, especially in children.
-
Infants and young children are the most commonly affected age group.
-
Despite the availability of effective vaccines, whooping cough continues to occur worldwide.
-
It remains a major public health problem, particularly in:
-
Infants
-
Unimmunized or partially immunized children
-
Individuals with waning immunity
-
-
The disease is associated with significant morbidity.
-
Mortality is highest in neonates, especially in severe or untreated cases.
-
Early diagnosis, timely treatment, and complete immunization are essential to reduce disease burden.
Etiological Agent
Whooping cough is caused by Bordetella pertussis, which has the following characteristics:
-
Small, Gram-negative coccobacillus
-
Strict aerobe
-
Non-motile, non-spore forming
-
Encapsulated
-
Extremely fastidious organism
Virulence Factors
The pathogenicity of B. pertussis is due to multiple toxins and adhesins:
-
Pertussis toxin (PT) – causes lymphocytosis, inhibits phagocytosis, and alters immune response
-
Adenylate cyclase toxin – increases intracellular cAMP, impairing neutrophil and macrophage function
-
Tracheal cytotoxin – damages ciliated epithelial cells
-
Filamentous hemagglutinin (FHA) – helps bacterial adherence
-
Fimbriae and pertactin – assist attachment to respiratory epithelium
Epidemiology
-
Occurs worldwide, both in developed and developing countries
-
Infants below 1 year of age are at highest risk
-
Adolescents and adults act as reservoirs of infection
-
Seasonal variation: more common in late summer and autumn
-
Immunity after infection or vaccination is not lifelong
Mode of Transmission
-
Spread by respiratory droplets during:
-
Coughing
-
Sneezing
-
Close personal contact
-
-
Highly infectious during the catarrhal stage
-
Secondary attack rate is very high in households
Incubation Period
-
Usually 7–10 days
-
Range: 5–21 days
Pathogenesis
-
Bordetella pertussis enters via the respiratory tract
-
Bacteria attach to ciliated epithelial cells of the trachea and bronchi
-
Toxins cause:
-
Destruction of cilia
-
Inhibition of mucus clearance
-
Accumulation of thick mucus
-
-
Airways become partially obstructed
-
Persistent stimulation of cough receptors leads to paroxysmal coughing
Clinical Features
The disease progresses through three classical stages:
1. Catarrhal Stage (1–2 Weeks)
-
Resembles a common upper respiratory tract infection
-
Symptoms include:
-
Mild fever
-
Coryza (runny nose)
-
Sneezing
-
Mild, irritating cough
-
-
Maximum infectivity occurs in this stage
-
Diagnosis is difficult due to non-specific symptoms
2. Paroxysmal Stage (2–6 Weeks)
-
Hallmark stage of pertussis
-
Features:
-
Repeated, violent coughing fits (paroxysms)
-
Each episode consists of 5–15 coughs
-
Followed by a loud inspiratory “whoop”
-
Post-tussive vomiting
-
Cyanosis during coughing
-
-
In infants:
-
Whoop may be absent
-
Apnea and choking episodes are common
-
3. Convalescent Stage (Weeks to Months)
-
Gradual decrease in frequency and severity of cough
-
Recovery is slow
-
Cough may recur with secondary respiratory infections
Laboratory Diagnosis
1. Specimen Collection
Specimen of Choice
-
Nasopharyngeal swab or nasopharyngeal aspirate
-
Throat swabs are not recommended due to low yield
Reason
-
Bordetella pertussis adheres firmly to the ciliated epithelium of the nasopharynx
Collection Technique
-
Use a Dacron or calcium alginate swab
-
Avoid cotton swabs (contain fatty acids toxic to bacteria)
-
Insert swab gently through nostril to posterior nasopharynx
-
Collect specimen during early (catarrhal or early paroxysmal stage) for best results
2. Microscopic Examination
Gram Staining
-
Shows:
-
Small, Gram-negative coccobacilli
-
-
Usually present singly or in pairs
Limitation
-
Low sensitivity and specificity
-
Cannot be relied upon for definitive diagnosis
3. Culture (Gold Standard)
Importance
-
Confirms diagnosis
-
Useful for epidemiological studies and antibiotic sensitivity testing
Culture Media
-
Bordet–Gengou Agar
-
Potato-based medium
-
Contains blood and glycerol
-
-
Regan–Lowe Medium
-
Charcoal-based medium
-
More commonly used today
-
Inhibits toxic substances and improves bacterial survival
-
Incubation
-
Temperature: 35–37°C
-
Atmosphere: Moist aerobic conditions
-
Duration: 3–7 days (sometimes up to 10 days)
Colony Characteristics
-
Small, smooth, glistening colonies
-
Described as “mercury drop” appearance
Limitations
-
Sensitivity decreases after:
-
2 weeks of illness
-
Prior antibiotic therapy
-
-
Time-consuming
4. Molecular Diagnosis (PCR)
Polymerase Chain Reaction (PCR)
-
Detects specific DNA sequences of B. pertussis
-
Most sensitive and rapid diagnostic method
Advantages
-
High sensitivity and specificity
-
Results available within hours
-
Useful even after antibiotic initiation
-
Preferred test in modern laboratories
Best Time
-
Catarrhal and early paroxysmal stages
5. Serological Tests
Antibody Detection
-
Measures antibodies against:
-
Pertussis toxin
-
Filamentous hemagglutinin
-
Methods
-
Enzyme-linked immunosorbent assay (ELISA)
Clinical Use
-
Helpful in:
-
Adolescents and adults
-
Late stages of disease
-
-
Not useful in early infection
Limitation
-
Interpretation difficult in vaccinated individuals
6. Hematological Findings
Complete Blood Count (CBC)
-
Marked absolute lymphocytosis is characteristic
-
Total leukocyte count may reach 20,000–50,000/µL
Mechanism
-
Caused by pertussis toxin, which inhibits lymphocyte migration from blood to tissues
Important Exam Point:
Lymphocytosis in a coughing child strongly suggests pertussis.
Treatment
Antibiotic Therapy
-
Most effective in early (catarrhal) stage
-
Drugs of choice:
-
Azithromycin
-
Clarithromycin
-
Erythromycin
-
-
Alternatives: Trimethoprim-sulfamethoxazole
Supportive Management
-
Oxygen therapy
-
Adequate nutrition and hydration
-
Monitoring for apnea in infants
-
Isolation for at least 5 days after starting antibiotics
Complications
More common in infants and unvaccinated children:
-
Pneumonia (most common cause of death)
-
Apnea
-
Seizures
-
Encephalopathy
-
Subconjunctival hemorrhage
-
Rectal prolapse
-
Failure to thrive
Prevention
Immunization
-
Most effective preventive measure
-
Given as:
-
DTaP in infants and children
-
Tdap booster in adolescents and adults
-
-
Part of national immunization programs
Chemoprophylaxis
-
Macrolide antibiotics for close contacts
Public Health Importance
-
Pertussis remains a re-emerging infection
-
Incomplete vaccination and waning immunity contribute to outbreaks
-
Early diagnosis, vaccination, and surveillance are essential for control
MCQs
1. Whooping cough is also known as:
A. Diphtheria
B. Bronchiolitis
C. Pertussis
D. Tuberculosis
Answer: C
2. Whooping cough is caused by:
A. Streptococcus pneumoniae
B. Haemophilus influenzae
C. Bordetella pertussis
D. Corynebacterium diphtheriae
Answer: C
3. Bordetella pertussis is:
A. Gram-positive bacillus
B. Gram-negative coccobacillus
C. Gram-positive cocci
D. Acid-fast bacillus
Answer: B
4. The disease mainly affects:
A. Elderly
B. Neonates and infants
C. Only adults
D. Pregnant women
Answer: B
5. Mode of transmission of pertussis is:
A. Feco-oral
B. Vector-borne
C. Respiratory droplets
D. Blood transfusion
Answer: C
6. Incubation period of whooping cough is usually:
A. 1–3 days
B. 3–5 days
C. 7–10 days
D. 30 days
Answer: C
7. Which stage of pertussis is most infectious?
A. Convalescent stage
B. Paroxysmal stage
C. Catarrhal stage
D. Recovery stage
Answer: C
8. The hallmark feature of whooping cough is:
A. Rash
B. Fever
C. Inspiratory whoop
D. Diarrhea
Answer: C
9. Severe coughing spells occur in which stage?
A. Catarrhal
B. Paroxysmal
C. Convalescent
D. Incubation
Answer: B
10. Post-tussive vomiting is seen in:
A. Catarrhal stage
B. Paroxysmal stage
C. Incubation stage
D. Latent stage
Answer: B
11. In infants, whooping cough may present with:
A. Diarrhea
B. Apnea
C. Skin lesions
D. Joint pain
Answer: B
12. The organism attaches to which cells?
A. Alveolar macrophages
B. Squamous cells
C. Ciliated epithelial cells
D. Endothelial cells
Answer: C
13. Which toxin causes lymphocytosis?
A. Endotoxin
B. Exotoxin A
C. Pertussis toxin
D. Hemolysin
Answer: C
14. Pertussis is mainly a:
A. Invasive disease
B. Toxin-mediated disease
C. Blood-borne disease
D. Zoonotic disease
Answer: B
15. Specimen of choice for diagnosis is:
A. Throat swab
B. Sputum
C. Nasopharyngeal swab
D. Blood
Answer: C
16. Best time to collect specimen is during:
A. Late convalescent stage
B. Early catarrhal stage
C. After 6 weeks
D. After antibiotics
Answer: B
17. Gold standard diagnostic method is:
A. Gram stain
B. PCR
C. Culture
D. Serology
Answer: C
18. Culture medium for Bordetella pertussis is:
A. Blood agar
B. Chocolate agar
C. Bordet–Gengou agar
D. MacConkey agar
Answer: C
19. Regan–Lowe medium contains:
A. Serum
B. Charcoal
C. Egg yolk
D. Tellurite
Answer: B
20. Colony appearance of B. pertussis is described as:
A. Rough colonies
B. Mucoid colonies
C. Mercury drop colonies
D. Hemolytic colonies
Answer: C
21. Most sensitive diagnostic test is:
A. Culture
B. PCR
C. Gram stain
D. CBC
Answer: B
22. PCR is useful because it is:
A. Cheap
B. Slow
C. Highly sensitive and rapid
D. Non-specific
Answer: C
23. CBC in pertussis shows:
A. Neutrophilia
B. Eosinophilia
C. Lymphocytosis
D. Thrombocytopenia
Answer: C
24. Lymphocytosis is caused due to:
A. Bone marrow failure
B. Pertussis toxin
C. Secondary infection
D. Antibiotics
Answer: B
25. Drug of choice for treatment is:
A. Penicillin
B. Cephalosporin
C. Macrolide
D. Aminoglycoside
Answer: C
26. Most effective stage for antibiotic therapy is:
A. Convalescent
B. Late paroxysmal
C. Early catarrhal
D. Recovery
Answer: C
27. Which antibiotic is commonly used?
A. Ciprofloxacin
B. Azithromycin
C. Vancomycin
D. Doxycycline
Answer: B
28. Most common complication of pertussis is:
A. Otitis media
B. Pneumonia
C. Arthritis
D. Nephritis
Answer: B
29. Severe complication seen in infants includes:
A. Hypertension
B. Apnea
C. Jaundice
D. Rash
Answer: B
30. Whooping cough vaccine is given as part of:
A. BCG
B. OPV
C. DPT
D. Measles
Answer: C
31. Pertussis vaccine is a:
A. Live attenuated vaccine
B. Killed vaccine
C. Toxoid
D. Recombinant vaccine
Answer: B
32. Acellular pertussis vaccine contains:
A. Whole bacteria
B. Only endotoxin
C. Purified antigens
D. Spores
Answer: C
33. Booster dose is required because immunity is:
A. Lifelong
B. Permanent
C. Short-lived
D. Genetic
Answer: C
34. Adolescents and adults act as:
A. Dead-end hosts
B. Reservoirs of infection
C. Immune carriers
D. Resistant hosts
Answer: B
35. Whooping sound is produced due to:
A. Bronchospasm
B. Sudden inspiration after coughing
C. Vocal cord damage
D. Lung collapse
Answer: B
36. Duration of paroxysmal stage is about:
A. 2–3 days
B. 1 week
C. 2–6 weeks
D. 6 months
Answer: C
37. The disease is most dangerous in:
A. Adults
B. Elderly
C. Infants
D. Teenagers
Answer: C
38. Throat swab is not preferred because:
A. Difficult to collect
B. Painful
C. Low bacterial yield
D. Expensive
Answer: C
39. Serology is useful mainly in:
A. Early disease
B. Neonates
C. Late disease in adults
D. Vaccinated infants
Answer: C
40. Culture sensitivity decreases after:
A. 24 hours
B. 3 days
C. 2 weeks
D. 6 months
Answer: C
41. The organism is:
A. Anaerobic
B. Facultative anaerobe
C. Strict aerobe
D. Microaerophile
Answer: C
42. Bordetella pertussis is:
A. Spore forming
B. Motile
C. Non-motile
D. Flagellated
Answer: C
43. Disease control mainly depends on:
A. Isolation only
B. Antibiotics only
C. Vaccination
D. Nutrition
Answer: C
44. Chemoprophylaxis is recommended for:
A. General population
B. Close contacts
C. Recovered patients
D. Vaccinated individuals
Answer: B
45. Most characteristic lab finding in a coughing child is:
A. Anemia
B. Neutropenia
C. Lymphocytosis
D. Thrombocytosis
Answer: C
46. Whooping cough primarily affects which system?
A. Digestive
B. Nervous
C. Respiratory
D. Urinary
Answer: C
47. Disease spreads fastest in:
A. Hospitals
B. Households
C. Open areas
D. Laboratories
Answer: B
48. Which stage shows gradual recovery?
A. Catarrhal
B. Paroxysmal
C. Convalescent
D. Incubation
Answer: C
49. Death in pertussis is usually due to:
A. Dehydration
B. Pneumonia
C. Renal failure
D. Liver failure
Answer: B
50. Best preventive strategy for pertussis is:
A. Early diagnosis
B. Antibiotic therapy
C. Vaccination
D. Isolation
Answer: C