Introduction
-
Hematology is the branch of laboratory medicine that deals with the study of blood, blood-forming organs, and blood diseases.
-
It includes analysis of red blood cells, white blood cells, platelets, hemoglobin, and coagulation factors.
-
The main objective of hematology is to diagnose and monitor conditions such as anemia, leukemia, infections, bleeding disorders, and bone marrow abnormalities.
-
Hematology laboratories perform both qualitative and quantitative tests such as complete blood count (CBC), peripheral smear examination, ESR, and coagulation profiles.
-
Proper laboratory organization ensures accuracy, reliability, and efficiency in test results.
-
It involves structured workflow, defined areas for sample collection, processing, analysis, and reporting.
-
The laboratory should have separate sections for hematology, biochemistry, microbiology, and clinical pathology, with trained staff and appropriate safety measures.
-
A well-organized hematology laboratory maintains standard operating procedures (SOPs), proper documentation, quality control programs, and regular maintenance of instruments to ensure precision and patient safety.
Hematology Laboratory
-
The hematology laboratory deals with the study and analysis of blood and its components.
-
It helps in diagnosing diseases like anemia, leukemia, infections, and bleeding disorders.
-
Common tests include CBC, hemoglobin estimation, ESR, PCV, and peripheral smear.
-
The lab uses instruments such as hematology analyzers, microscopes, and centrifuges.
-
Blood samples are collected in EDTA tubes and analyzed under controlled conditions.
-
Quality control and calibration ensure accuracy and reliability of test results.
-
Strict biosafety measures and proper waste disposal are followed to maintain safety and hygiene.
Importance of a Haematology Laboratory
Haematology laboratories are indispensable in healthcare for several reasons:
- Accurate Diagnosis of Blood Disorders:
- Haematology labs help diagnose various conditions, including anaemia, clotting disorders, leukaemia, and other blood-related cancers. Accurate diagnosis is key to developing effective treatment plans.
- Guiding Treatment:
- Haematology tests like complete blood counts (CBC), clotting factor analysis, and bone marrow examination provide critical data for guiding treatments, such as chemotherapy for leukaemia, blood transfusions, or anticoagulant therapy for clotting disorders.
- Monitoring Disease Progression:
- Haematology labs monitor patients with chronic blood disorders to assess disease progression or response to treatment. For instance, patients with anaemia might undergo periodic haemoglobin tests to evaluate the effectiveness of iron supplements or other therapies.
- Blood Transfusion and Donation Safety:
- Haematology labs are involved in blood typing and cross-matching for blood transfusions. They ensure that donated blood is safe and compatible with the recipient, minimizing adverse reactions or infection risks.
- Supporting Research:
- Haematology labs contribute to research in blood diseases, including developing new treatments for conditions like sickle cell anaemia or novel approaches to managing clotting disorders.
- Public Health and Epidemiology:
- Haematology labs can detect outbreaks of infectious diseases that affect the blood, such as malaria or certain viral infections, helping guide public health interventions.
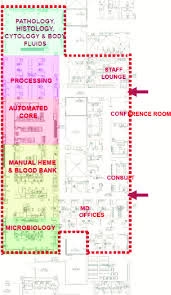
Laboratory Organization
-
Purpose
-
- The hematology laboratory is an essential part of a clinical diagnostic setup, responsible for examining blood and bone marrow samples.
- It helps in diagnosing diseases like anemia, leukemia, infections, clotting disorders, and other blood abnormalities.
- Proper organization ensures accurate, safe, and efficient functioning.
-
Layout and Division of Work Areas
The laboratory should be well-planned and divided into specific areas to prevent cross-contamination and confusion.-
Sample Collection Area: For receiving and labeling patient samples.
-
Analytical Area: Where hematology tests are performed (CBC, ESR, PCV, coagulation tests, etc.).
-
Microscopy Area: For preparing and examining peripheral smears and bone marrow slides.
-
Record and Reporting Section: For data entry, report preparation, and verification.
-
Storage Area: For storing reagents, controls, and specimens.
-
Waste Disposal Area: For proper segregation and disposal of biohazardous materials.
-
-
Essential Equipment and Instruments
A hematology laboratory should be equipped with:-
Hematology analyzer (for complete blood count)
-
Microscopes (binocular/compound)
-
Centrifuge (for plasma and PCV separation)
-
Pipettes and dispensers
-
Coagulometer (for PT, APTT tests)
-
ESR stand, hemocytometer, and counting chambers
-
Water bath and vortex mixer
-
Refrigerator (for reagent storage)
-
-
Personnel and Responsibilities
A well-organized hematology lab includes:-
Pathologist / Hematologist: Overall supervision, interpretation of results, and validation of reports.
-
Medical Laboratory Technologist (MLT): Performs sample analysis, maintains equipment, and records results.
-
Lab Assistant: Helps in cleaning glassware, reagent preparation, and handling samples.
-
Phlebotomist / Technician: Collects patient blood samples and ensures proper labeling.
-
-
Standard Operating Procedures (SOPs)
Every hematology lab must follow written SOPs for all tests and processes to maintain uniformity and accuracy.-
SOPs should cover specimen collection, handling, storage, and disposal.
-
Procedures for calibrating, maintaining, and troubleshooting instruments must be documented.
-
Each test (e.g., CBC, ESR, coagulation) must have a step-by-step method and acceptable reference range.
-
-
Quality Assurance and Control
-
Internal Quality Control (IQC): Daily checks using control samples to ensure instrument accuracy.
-
External Quality Assessment (EQA): Participation in external programs for inter-laboratory comparison.
-
Regular calibration of analyzers and instruments must be maintained in a logbook.
-
Proper reagent preparation, expiration date monitoring, and maintenance of cleanliness are crucial.
-
-
Safety and Waste Management
-
Personnel must follow biosafety guidelines, wear PPE (lab coat, gloves, mask), and handle samples carefully.
-
Use color-coded containers for biomedical waste segregation (red, yellow, blue, black).
-
Dispose of sharps (needles, lancets) in puncture-proof containers.
-
Spills should be disinfected immediately with 1% sodium hypochlorite.
-
Fire safety, first-aid kits, and emergency exits must be clearly marked and accessible.
-
-
Record Keeping and Documentation
-
Maintain registers for sample receipt, test results, reagent preparation, and equipment maintenance.
-
Keep a daily work log for tests performed, results verified, and QC checks done.
-
Patient reports should be signed and verified by the authorized pathologist before release.
-
Electronic Laboratory Information Systems (LIS) are now widely used for efficiency and traceability.
-
-
Haematology Laboratory Tests
Common tests routinely performed include:-
Complete Blood Count (CBC)
-
Hemoglobin estimation
-
Hematocrit (PCV)
-
ESR (Erythrocyte Sedimentation Rate)
-
Peripheral blood smear examination
-
Reticulocyte count
-
Coagulation profile (PT, APTT, INR)
-
Bone marrow aspiration and cytology
-
-
Importance of Organisation
-
-
Reduces errors and contamination.
-
Improves efficiency and accuracy.
-
Ensures safety of personnel and reliability of results.
-
Facilitates smooth workflow and proper communication among staff.
-
Helps maintain compliance with NABL, WHO, and other accreditation standards.
-
Basic Equipment
- Haematology Analyser:
- A crucial machine for conducting complete blood counts (CBC) measures the levels of red and white blood cells, haemoglobin, hematocrit, and platelets. Modern analyzers provide rapid, automated results for multiple parameters.
- Centrifuge:
- Spinning samples at high speeds is used to separate blood components (e.g., plasma from cells). Centrifugation is essential for preparing samples for further tests.
- Microscope:
- It is essential to examine blood smears and bone marrow samples and identify abnormal cells or parasites (such as malaria) that can affect blood health.
- Coagulometer:
- Analyzes blood clotting ability by measuring parameters like prothrombin time (PT) and activated partial thromboplastin time (aPTT). It’s vital for diagnosing clotting disorders and monitoring patients on anticoagulant therapies.

- Analyzes blood clotting ability by measuring parameters like prothrombin time (PT) and activated partial thromboplastin time (aPTT). It’s vital for diagnosing clotting disorders and monitoring patients on anticoagulant therapies.
- Blood Gas Analyzer:
- Measures the levels of gases (e.g., oxygen, carbon dioxide) and electrolytes in blood samples. This equipment is used in critical care settings to assess the acid-base balance in patients.
- Flow Cytometer:
- A sophisticated tool used for counting and analyzing blood cells’ size, shape, and properties. It is especially useful in diagnosing hematologic cancers like leukemia and lymphoma.
- Bone Marrow Biopsy Equipment:
- Used to collect bone marrow samples for examination. This is a critical procedure in diagnosing blood cancers and other marrow disorders.
- Slide Stainer:
- Automatically stains blood smears or bone marrow samples, enabling clear visualization of cells under the microscope. Common stains include Wright-Giemsa, used for blood films.
- Refrigerator/Freezer:
- For storing blood samples, reagents, and other temperature-sensitive materials under controlled conditions to preserve their integrity for testing.
MCQs
-
Hematology is the study of:
A. Tissues
B. Blood and blood-forming organs
C. Enzymes
D. Hormones -
The main function of a hematology laboratory is to:
A. Prepare histological slides
B. Analyze blood samples
C. Grow bacterial cultures
D. Test urine samples -
Which of the following tests is included in a routine hematology profile?
A. Blood sugar test
B. Complete Blood Count (CBC)
C. Liver function test
D. Lipid profile -
The liquid portion of blood is called:
A. Plasma
B. Serum
C. Lymph
D. Water -
Hemoglobin is present in:
A. WBCs
B. RBCs
C. Platelets
D. Plasma -
Which of the following tubes is commonly used for hematology testing?
A. Heparin tube
B. Citrate tube
C. EDTA tube
D. Fluoride tube -
The function of hemoglobin is to:
A. Help in blood clotting
B. Carry oxygen
C. Fight infection
D. Transport hormones -
The normal color of healthy plasma is:
A. Red
B. Yellow
C. Colorless
D. Blue -
The study of WBCs is called:
A. Erythrology
B. Leukocytology
C. Cytology
D. Immunology -
ESR stands for:
A. Erythrocyte Sedimentation Rate
B. Erythrocyte Sensitivity Ratio
C. Enzyme Stability Range
D. Erythrocyte Structural Ratio -
Which instrument is used for ESR determination?
A. Wintrobe or Westergren tube
B. Hemocytometer
C. Spectrophotometer
D. Colorimeter -
The normal ESR value for an adult male is approximately:
A. 0–5 mm/hr
B. 10–20 mm/hr
C. 20–40 mm/hr
D. 40–60 mm/hr -
The hematocrit (PCV) represents:
A. Volume of plasma
B. Volume of packed red cells
C. Amount of hemoglobin
D. Number of WBCs -
Which cell is responsible for blood clotting?
A. RBC
B. WBC
C. Platelet
D. Neutrophil -
The main anticoagulant used in hematology is:
A. Sodium citrate
B. EDTA
C. Potassium oxalate
D. Sodium fluoride -
The normal lifespan of red blood cells is:
A. 60 days
B. 90 days
C. 120 days
D. 180 days -
A fall in hemoglobin level indicates:
A. Leukemia
B. Anemia
C. Infection
D. Dehydration -
Peripheral smear examination is done to:
A. Check blood glucose
B. Identify shape and size of blood cells
C. Measure ESR
D. Test urea level -
Which stain is commonly used in peripheral smear preparation?
A. Gram stain
B. Leishman stain
C. Acid-fast stain
D. Giemsa stain -
WBCs are mainly responsible for:
A. Carrying oxygen
B. Fighting infection
C. Clotting blood
D. Transporting nutrients -
Platelets are also known as:
A. Thrombocytes
B. Erythrocytes
C. Leukocytes
D. Lymphocytes -
The main purpose of laboratory organization is to:
A. Increase cost
B. Maintain workflow and accuracy
C. Delay reporting
D. Reduce staff -
The hematology laboratory is usually divided into:
A. Collection, analysis, microscopy, and reporting sections
B. Kitchen and storage only
C. Analysis and waste only
D. None of these -
Which area is used for reagent preparation in a hematology lab?
A. Reception area
B. Microscopy room
C. Reagent preparation room
D. Storage area -
The microscope used in hematology laboratory is usually:
A. Electron microscope
B. Binocular microscope
C. Stereo microscope
D. Projection microscope -
Which of the following is not a hematology test?
A. Hemoglobin test
B. Lipid profile
C. ESR
D. Peripheral smear -
The safety measure in the hematology lab includes:
A. Wearing PPE
B. Eating in lab
C. Ignoring spills
D. Open footwear -
Quality control ensures:
A. Incorrect test results
B. Accuracy and precision of reports
C. Delay in reporting
D. Cost reduction only -
Standard Operating Procedures (SOPs) are important because they:
A. Increase workload
B. Maintain uniformity and reliability in tests
C. Are optional
D. Are used only for emergencies -
Which color-coded container is used for sharp waste?
A. Yellow
B. Red
C. Blue
D. White (translucent puncture-proof) -
The supervisor of a hematology laboratory is usually a:
A. Microbiologist
B. Pathologist or Hematologist
C. Pharmacist
D. Technician -
Proper labeling of blood samples prevents:
A. Delays
B. Sample mix-ups and reporting errors
C. Quality control
D. Power failure -
In a hematology lab, the sample is usually collected in:
A. Urine container
B. Sterile swab
C. EDTA tube
D. Plain tube -
The term “biosafety” in laboratory refers to:
A. Preventing infections and accidents
B. Increasing sample speed
C. Storing food
D. Office safety -
A well-organized hematology lab ensures:
A. Accuracy, efficiency, and safety
B. Wastage and confusion
C. More contamination
D. Slower workflow
✅ Answer Key
-
B
-
B
-
B
-
A
-
B
-
C
-
B
-
B
-
B
-
A
-
A
-
A
-
B
-
C
-
B
-
C
-
B
-
B
-
B
-
B
-
A
-
B
-
A
-
C
-
B
-
B
-
A
-
B
-
B
-
D
-
B
-
B
-
C
-
A
-
A