Introduction
- Streptococcus pneumoniae is a significant human pathogen responsible for various serious infections, including pneumonia, meningitis, and otitis media.
- Understanding its characteristics, pathogenic mechanisms, and effective laboratory diagnosis is crucial for managing infections caused by pneumococci.
- Continuous surveillance and research are essential to address the challenges of antibiotic resistance and improve prevention strategies through vaccination.
General Character
- Genus: Streptococcus
- Species: Streptococcus pneumoniae
- Family: Streptococcaceae
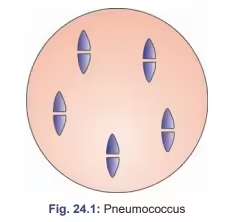
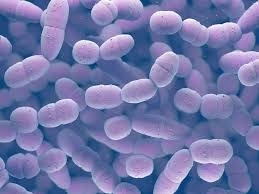
- Gram Staining: Pneumococci are Gram-positive cocci, appearing purple due to a thick peptidoglycan layer.
- Shape and Arrangement:
- Shape: They are lancet-shaped cocci, often described as elliptical.
- Arrangement: Typically found in pairs (diplococci) or short chains.
- Oxygen Requirements: S. pneumoniae is a facultative anaerobe, meaning it can grow in aerobic and anaerobic conditions but prefers aerobic environments.
Morphology
- Cell Wall Structure:
- It comprises a thick peptidoglycan layer, which is crucial for structural integrity and provides resistance to lysis.
- Contains teichoic and lipoteichoic acids, contributing to the cell wall’s properties and pathogenicity.
- Capsule:
- S. pneumoniae possesses a polysaccharide capsule that is a major virulence factor. The capsule protects against phagocytosis and is the basis for its classification into different serotypes.
- Surface Structures:
- The capsule is critical for virulence, preventing opsonization and phagocytosis by immune cells.
Cultural Characteristics
- Growth Media:
- Blood Agar: Grows well on blood agar, where it typically exhibits α-hemolysis (partial hemolysis) due to hydrogen peroxide production.
- Chocolate Agar: Often used for enhanced growth, especially in clinical specimens.
- Selective Media: It can be grown on bile-esculin agar but is not strictly necessary.
- Colony Appearance:
- Colonies are small, mucoid, and glistening, often with a greenish hue around them due to partial hemolysis.
- Temperature and pH Range:
- The optimal growth temperature is around 37°C, with a preferred pH range of 6.5 to 7.5.
Biochemical Reactions
- Catalase Test: S. pneumoniae is catalase-negative, which helps distinguish it from staphylococci.
- Bile Solubility Test: S. pneumoniae is bile-soluble, which means it can be lysed by bile salts, differentiating it from other alpha-hemolytic streptococci (like S. mitis).
- Optochin Sensitivity Test: S. pneumoniae is sensitive to optochin (disk diffusion test), another distinguishing feature.
- Fermentation: It ferments carbohydrates, producing lactic acid, but does not produce gas during fermentation.
Pathogenicity
- Virulence Factors:
- Capsule: Prevents phagocytosis and is a key virulence factor.
- Pneumolysin: A toxin that damages host tissues, activates the immune response, and contributes to inflammation and tissue injury.
- Autolysins: Enzymes that can contribute to releasing pneumolysin and other virulence factors during bacterial lysis.
- Surface adhesins: Facilitate adherence to respiratory epithelium, aiding colonization and infection.
- Clinical Infections:
- Pneumonia: The most common disease caused by S. pneumoniae, often called pneumococcal pneumonia. Symptoms include cough, fever, chest pain, and difficulty breathing.
- Meningitis: S. pneumoniae is one of the leading causes of bacterial meningitis in adults and children.
- Otitis Media: A common cause of middle ear infections, especially in children.
- Sinusitis: This can also lead to sinus infections.
- Bacteraemia: This can result in bloodstream infections, leading to sepsis.
Laboratory Diagnosis
- Specimen Collection: Clinical specimens can include sputum, blood, cerebrospinal fluid (CSF), or middle ear fluid.
- Microscopic Examination:
- A Gram stain reveals Gram-positive diplococci, often within white blood cells, indicating an active infection.
- Culture Techniques:
- Specimens are inoculated onto blood agar and incubated in a CO₂-enriched atmosphere to enhance growth.
- Identification involves observing colony morphology and performing biochemical tests (bile solubility, optochin sensitivity).
- Antigen Detection: Rapid antigen tests can detect pneumococcal polysaccharides in urine or CSF, providing quick results.
- Molecular Methods: PCR techniques can be used for rapid identification and serotyping of pneumococci, especially in severe infections or when cultures are negative.
Antibiotic Resistance
- Resistance Patterns: S. pneumoniae has shown increasing resistance to penicillin and other antibiotics, complicating treatment options.
- Multidrug-Resistant Strains: The emergence of strains resistant to macrolides, tetracyclines, and fluoroquinolones has been reported.
- Treatment Options: Empirical treatment often includes ceftriaxone or vancomycin, particularly in severe cases. Antibiotic susceptibility testing is essential for guiding treatment.
Prevention
-
Vaccination is the most important measure.
-
PCV13/PCV15/PCV20 for infants, elderly, and immunocompromised.
-
PPSV23 for adults ≥65 years and high-risk groups.
-
-
Maintain respiratory hygiene:
-
Cover mouth/nose while coughing or sneezing
-
Use masks during infections
-
Frequent handwashing
-
-
High-risk groups require special care:
-
Asplenic, HIV-positive, elderly, chronic diseases
-
Combined PCV + PPSV23 schedule
-
-
Avoid smoking, as it increases colonization and pneumonia risk.
-
Prevent viral infections (especially influenza) through vaccination and hygiene practices.
-
Improve immunity through good nutrition and healthy lifestyle.
-
Reduce overcrowding and ensure good ventilation in closed spaces.
MCQs
1. Streptococcus pneumoniae is:
A. Gram-negative coccus
B. Gram-positive diplococcus
C. Acid-fast bacillus
D. Spirochete
2. The characteristic shape of S. pneumoniae is:
A. Kidney-shaped diplococci
B. Comma-shaped
C. Lancet-shaped diplococci
D. Coccobacilli
3. S. pneumoniae is commonly found as part of normal flora in:
A. Skin
B. Nasopharynx
C. Small intestine
D. Stomach
4. Major virulence factor of S. pneumoniae:
A. Lipid A
B. Capsule
C. Pili
D. Flagella
5. Colony appearance on blood agar is:
A. Large mucoid colonies
B. Metallic sheen colonies
C. “Draughtsman” or sunken colonies
D. Swarming growth
6. Type of hemolysis S. pneumoniae produces:
A. Beta hemolysis
B. Gamma hemolysis
C. Alpha hemolysis
D. Variable hemolysis
7. S. pneumoniae is bile:
A. Resistant
B. Sensitive
C. Partially resistant
D. Unaffected
8. S. pneumoniae is optochin:
A. Resistant
B. Sensitive
C. Negative
D. Indeterminate
9. Quellung reaction is used to detect:
A. Flagella
B. Capsule swelling
C. Cell wall teichoic acid
D. M protein
10. Pneumococcal pneumonia classically presents with:
A. Dry cough
B. Rust-colored sputum
C. Bloody diarrhea
D. Painless ulcers
11. Most common cause of bacterial pneumonia in adults:
A. K. pneumoniae
B. S. aureus
C. S. pneumoniae
D. H. influenzae
12. “Lancet-shaped diplococci” are seen in:
A. Gonorrhea
B. Pneumococcal infections
C. Meningitis from meningococcus
D. Diphtheria
13. In sputum smear, S. pneumoniae appears as:
A. Chains
B. Clusters
C. Pairs (diplococci)
D. Single bacilli
14. S. pneumoniae is a leading cause of:
A. Endocarditis
B. Otitis media
C. Gastroenteritis
D. UTI
15. Population at highest risk for pneumococcal infection:
A. Young healthy adults
B. Alcoholics and elderly
C. Teenagers
D. Athletes
16. Capsule of S. pneumoniae is composed of:
A. Peptidoglycan
B. Teichoic acid
C. Polysaccharide
D. Lipoprotein
17. Lobar pneumonia caused by S. pneumoniae typically affects:
A. One lobe of lung
B. Multiple lobes
C. Both lungs uniformly
D. Bronchi only
18. Pneumococcal meningitis is most common in:
A. Adults
B. Neonates
C. Elderly
D. Immunocompromised
19. Most important test to differentiate S. pneumoniae from viridans streptococci:
A. Gram stain
B. Optochin sensitivity
C. Catalase test
D. Coagulase test
20. S. pneumoniae is catalase:
A. Positive
B. Negative
C. Variable
D. Weak
21. Common complication of pneumococcal pneumonia:
A. Cavitation
B. Pleural effusion
C. Abscess
D. Pneumothorax
22. Pneumolysin is a:
A. Exotoxin
B. Cytotoxin
C. Neurotoxin
D. Enterotoxin
23. The capsule protects S. pneumoniae against:
A. Complement
B. Neutrophil phagocytosis
C. Antibodies
D. All of the above
24. Pneumococcal vaccine available as 13-valent is:
A. PPSV23
B. BCG
C. PCV13
D. DPT
25. PPSV23 vaccine is:
A. Polysaccharide vaccine
B. Conjugate vaccine
C. Live vaccine
D. Toxoid vaccine
26. PCV vaccines induce:
A. T-cell independent immunity
B. T-cell dependent immunity
C. No immunological memory
D. Immediate hypersensitivity
27. The drug of choice for pneumococcal infection is historically:
A. Penicillin
B. Vancomycin
C. Chloramphenicol
D. Tetracycline
28. Increasing resistance to penicillin is due to:
A. Beta-lactamase
B. Altered penicillin-binding proteins (PBPs)
C. Decreased capsule
D. Loss of pili
29. Pneumococcus is identified in CSF by:
A. India ink
B. Latex agglutination
C. Acid-fast staining
D. Albert stain
30. S. pneumoniae fermentation pattern:
A. Ferments glucose only
B. Ferments several sugars producing lactic acid
C. No fermentation
D. Ferments lactose only
31. Pneumococcal infection commonly follows:
A. Typhoid fever
B. Viral URTI or influenza
C. Dengue fever
D. Malaria
32. In blood agar, S. pneumoniae colonies become “draughtsman” due to:
A. Hemolysis
B. Autolysis
C. Toxin secretion
D. Capsule breakdown
33. Nasopharyngeal colonization is mediated by:
A. Pili
B. Capsule
C. Teichoic acid
D. Surface adhesins
34. Pneumococcal meningitis CSF findings include:
A. High protein, low glucose
B. Low protein, high glucose
C. High RBCs
D. Low WBCs
35. Pneumococcal bacteremia is common in:
A. Asplenic patients
B. Diabetics
C. Pregnant women
D. Athletes
36. Pneumococcal vaccine is contraindicated in:
A. Pregnancy
B. Immunocompromised states
C. Anaphylaxis to vaccine components
D. HIV
37. Most common cause of community-acquired meningitis in adults:
A. Listeria
B. Neisseria
C. Streptococcus pneumoniae
D. Haemophilus influenzae
38. Pneumococcus is bile soluble because of:
A. Capsule
B. Pneumolysin
C. Autolysin enzyme (amidase)
D. Bile salt permeability
39. The gram stain of S. pneumoniae shows:
A. Pink bacilli
B. Purple diplococci
C. Clustered cocci
D. Spiral rods
40. Pneumococcal pneumonia classically shows which sign on chest X-ray?
A. Ground-glass opacity
B. Lobar consolidation
C. Miliary pattern
D. Reticulonodular pattern
✅ Answer Key (Separate Section)
1-B
2-C
3-B
4-B
5-C
6-C
7-B
8-B
9-B
10-B
11-C
12-B
13-C
14-B
15-B
16-C
17-A
18-D
19-B
20-B
21-B
22-B
23-D
24-C
25-A
26-B
27-A
28-B
29-B
30-B
31-B
32-B
33-D
34-A
35-A
36-C
37-C
38-C
39-B
40-B