
Introduction
-
Haemoglobinometry is the quantitative measurement of haemoglobin concentration in blood.
-
Haemoglobin is an iron-containing respiratory pigment present in red blood cells.
-
It is responsible for the transport of oxygen from lungs to tissues and carbon dioxide from tissues to lungs.
-
Haemoglobinometry is a fundamental hematological investigation.
-
It is routinely performed as part of the Complete Blood Count (CBC).
-
The test helps in the diagnosis and classification of anemia.
-
It is useful in detecting polycythemia and hemoconcentration.
-
Haemoglobinometry is essential for clinical diagnosis, treatment monitoring, and follow-up.
-
It is widely used in hospitals, diagnostic laboratories, and blood donation camps.
-
Various manual, semi-automated, and automated methods are employed for haemoglobin estimation.

Importance
-
Haemoglobin estimation helps to assess the oxygen-carrying capacity of blood.
-
It is essential for the diagnosis of anemia and its severity.
-
Helps in the classification of anemia (mild, moderate, severe).
-
Useful in detecting polycythemia (increased hemoglobin level).
-
Important for nutritional assessment, especially iron, vitamin B12, and folate deficiency.
-
Routinely performed as a part of Complete Blood Count (CBC).
-
Essential in antenatal care to detect anemia in pregnant women.
-
Helps in pre-operative evaluation to assess surgical fitness.
-
Useful in monitoring response to treatment in anemia.
-
Important in screening programs and blood donation camps.
-
Aids in diagnosing chronic diseases such as chronic kidney disease and malignancy.
-
Helpful in assessing patients with chronic blood loss or hemorrhage.
-
Plays a role in evaluating hypoxia and respiratory disorders.
-
Important for public health assessment of anemia prevalence in the population.
Normal Values
| Group | Normal Range |
|---|---|
| Adult Male | 13–17 g/dL |
| Adult Female | 12–15 g/dL |
| Children | 11–14 g/dL |
| Newborn | 16–20 g/dL |
Principle of Haemoglobinometry
Haemoglobinometry is based on the principle that:
Haemoglobin is converted into a stable colored compound, and the intensity of the color produced is directly proportional to the haemoglobin concentration in the blood.
The color intensity is measured either visually or photometrically, depending on the method used.
Common Methods of Haemoglobin Estimation
-
Sahli’s (Acid Hematin) Method
-
Cyanmethemoglobin Method (Reference method)
-
Oxyhaemoglobin Method
-
Azidemethemoglobin Method
-
Automated Hematology Analyzer
Sahli’s (Acid Hematin) Method
Principle
Sahli’s method is based on the principle that:
Hemoglobin reacts with 0.1 N hydrochloric acid (HCl) to form brown-colored acid hematin.
The intensity of the color produced is directly proportional to the hemoglobin concentration in the blood.
The hemoglobin concentration is estimated by visual color comparison with a standard scale.
Requirements
-
Sahli hemoglobinometer (comparator with standard brown glass)
-
Sahli graduated tube
-
Sahli pipette (20 µL)
-
0.1 N Hydrochloric acid
-
Distilled water
-
Glass stirrer
-
Lancet
-
Blood sample (capillary or venous)
Procedure
-
Fill the Sahli graduated tube with 0.1 N HCl up to the 2 g% mark.
-
Using Sahli pipette, draw 20 µL of blood.
-
Add the blood carefully into the acid in the Sahli tube.
-
Mix thoroughly with a glass stirrer.
-
Allow the mixture to stand for 10 minutes for complete conversion to acid hematin.
-
Add distilled water drop by drop, mixing continuously.
-
Continue dilution until the color matches the standard comparator.
-
Read the hemoglobin value directly from the graduated scale in g/dL.
Advantages
-
Simple and easy to perform
-
Inexpensive method
-
Requires minimal equipment
-
Suitable for field surveys and teaching laboratories
-
Does not require electricity or sophisticated instruments
Limitations
-
Less accurate compared to photometric methods
-
Subjective error due to visual color matching
-
Not suitable for abnormal hemoglobin variants
-
Turbidity due to lipemia or high leukocyte count affects accuracy
-
Cannot measure carboxyhemoglobin and methemoglobin accurately
-
Not recommended as a reference method
Cyanmethemoglobin Method
Principle
The Cyanmethemoglobin method is based on the principle that:
Hemoglobin is oxidized to methemoglobin by potassium ferricyanide, which then reacts with potassium cyanide to form cyanmethemoglobin, a stable colored compound.
The intensity of the color produced is directly proportional to the hemoglobin concentration and is measured photometrically at 540 nm using a colorimeter or spectrophotometer.
This method is the reference method recommended by WHO for hemoglobin estimation.
Requirements
-
Whole blood sample (capillary or venous)
-
Drabkin’s reagent
(contains potassium ferricyanide, potassium cyanide, and buffer) -
Cyanmethemoglobin standard
-
Test tubes
-
Pipettes / Micropipettes
-
Colorimeter or spectrophotometer
-
Cuvettes
Procedure
-
Take 5.0 mL of Drabkin’s reagent in a test tube.
-
Add 20 µL of well-mixed blood to the reagent.
-
Mix gently to avoid frothing.
-
Allow the mixture to stand for 10 minutes at room temperature for complete color development.
-
Set the colorimeter at 540 nm using Drabkin’s reagent as blank.
-
Measure the absorbance of the test sample.
-
Compare the absorbance with that of the standard.
-
Calculate hemoglobin concentration and express the result in g/dL.
Calculation
Hemoglobin (g/dL) = Absorbance of test / Absorbance of standard × Concentration of standard
Advantages
-
High accuracy and reproducibility
-
Internationally accepted reference method
-
Measures almost all forms of hemoglobin (oxyHb, deoxyHb, metHb, carboxyHb)
-
Objective and less observer-dependent
-
Suitable for routine and research laboratories
Limitations
-
Drabkin’s reagent contains cyanide (toxic)
-
Requires colorimeter or spectrophotometer
-
Sulfhemoglobin is not measured accurately
-
Proper waste disposal is essential
Precautions
-
Handle Drabkin’s reagent carefully due to cyanide content
-
Use clean cuvettes and proper wavelength (540 nm)
-
Avoid hemolyzed or clotted samples
-
Calibrate the instrument properly
Oxyhaemoglobin Method
Principle
The oxyhaemoglobin method is based on the principle that:
Hemoglobin is converted into oxyhaemoglobin by dilution with an alkaline solution.
The intensity of the red color formed is directly proportional to the haemoglobin concentration and is measured photometrically.
Requirements
-
Whole blood sample
-
Distilled water or dilute ammonium hydroxide
-
Test tubes
-
Pipettes
-
Colorimeter / Spectrophotometer
-
Cuvettes
Procedure
-
Take a measured volume of distilled water in a test tube.
-
Add a fixed volume of blood and mix well.
-
Allow complete hemolysis and oxygenation to form oxyhaemoglobin.
-
Measure absorbance at 540 nm or 576 nm against a reagent blank.
-
Calculate haemoglobin concentration using a standard.
Advantages
-
Simple and rapid method
-
No toxic chemicals used
-
Suitable for routine laboratory work
Limitations
-
Measures only oxyhaemoglobin
-
Not suitable in presence of abnormal hemoglobin derivatives
-
Less accurate than cyanmethemoglobin method
Azidemethemoglobin Method
Principle
The azidemethemoglobin method is based on the principle that:
Hemoglobin is oxidized to methemoglobin and then reacts with sodium azide to form azidemethemoglobin, a stable colored compound.
The color intensity is measured photometrically and is directly proportional to haemoglobin concentration.
This method is widely used in modern hematology analyzers.
Requirements
-
Whole blood sample
-
Azide reagent
-
Test tubes
-
Pipettes
-
Colorimeter / Automated analyzer
Procedure
-
Mix blood with azide-containing reagent.
-
Allow complete reaction to form azidemethemoglobin.
-
Measure absorbance at 570 nm.
-
Determine haemoglobin concentration using calibration data.
Advantages
-
Does not contain cyanide (safer than Drabkin’s method)
-
High accuracy and precision
-
Stable end product
-
Suitable for automated systems
Limitations
-
Sulfhemoglobin is not measured
-
Requires analyzer or photometric equipment
Automated Hematology Analyzer
Principle
Automated hematology analyzers estimate haemoglobin using:
Photometric measurement after chemical conversion of hemoglobin to a stable derivative (commonly azidemethemoglobin).
Modern analyzers also simultaneously measure RBC count, WBC count, platelet count, and red cell indices.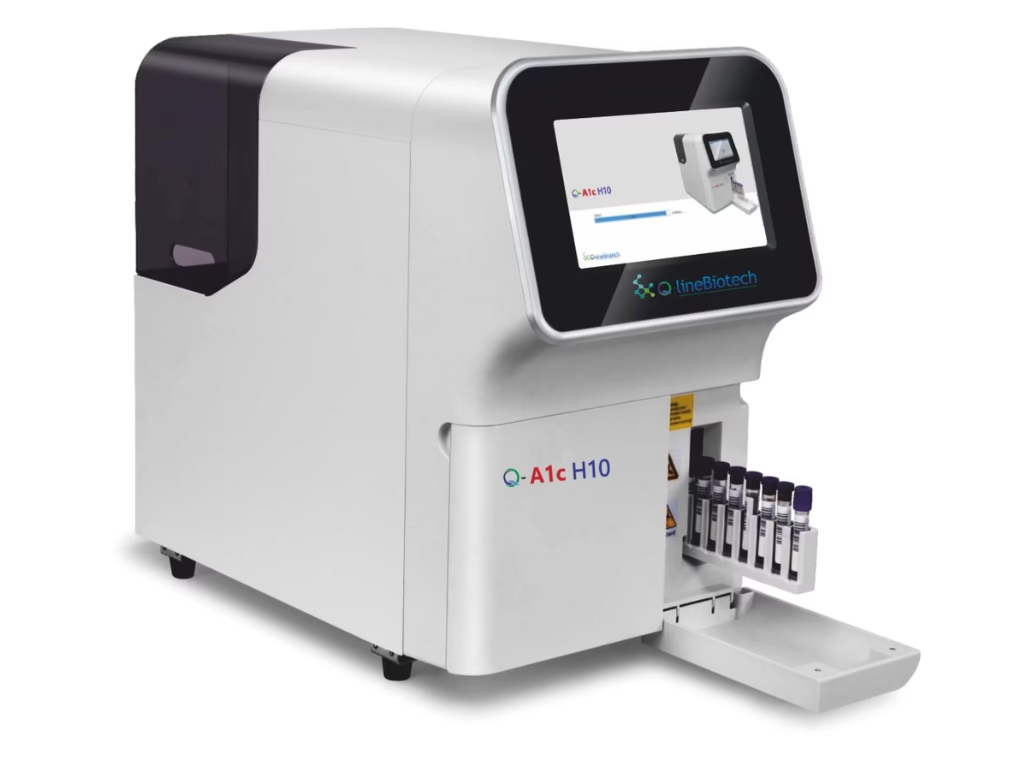
Requirements
-
EDTA anticoagulated blood
-
Automated hematology analyzer
-
Reagents specific to the analyzer
Procedure
-
Collect blood in an EDTA tube.
-
Load the sample into the analyzer.
-
The analyzer aspirates the sample automatically.
-
Hemoglobin is chemically converted and measured photometrically.
-
Results are displayed digitally and printed.
Advantages
-
Highly accurate and reproducible
-
Rapid processing of large number of samples
-
Minimal human error
-
Provides complete CBC parameters
-
Suitable for high-throughput laboratories
Limitations
-
Expensive equipment and maintenance
-
Requires trained personnel
-
Instrument calibration and quality control essential
MCQs
1. Haemoglobin is primarily responsible for:
A. Immunity
B. Blood clotting
C. Oxygen transport
D. Hormone synthesis
Answer: C
2. Haemoglobin is present in:
A. Plasma
B. White blood cells
C. Platelets
D. Red blood cells
Answer: D
3. Haemoglobinometry refers to:
A. Measurement of RBC count
B. Measurement of hemoglobin concentration
C. Measurement of hematocrit
D. Measurement of plasma proteins
Answer: B
4. Normal hemoglobin level in adult males is:
A. 10–12 g/dL
B. 11–14 g/dL
C. 13–17 g/dL
D. 18–22 g/dL
Answer: C
5. Normal hemoglobin level in adult females is:
A. 9–11 g/dL
B. 10–12 g/dL
C. 12–15 g/dL
D. 15–18 g/dL
Answer: C
6. Low hemoglobin level indicates:
A. Polycythemia
B. Leukocytosis
C. Anemia
D. Thrombocytosis
Answer: C
7. Increased hemoglobin level is seen in:
A. Iron deficiency anemia
B. Polycythemia vera
C. Hemolytic anemia
D. Megaloblastic anemia
Answer: B
8. Haemoglobin estimation is part of:
A. Liver function test
B. Renal function test
C. Complete blood count
D. Lipid profile
Answer: C
9. Sahli’s method is also known as:
A. Cyanmethemoglobin method
B. Oxyhaemoglobin method
C. Acid hematin method
D. Azide method
Answer: C
10. In Sahli’s method, hemoglobin is converted into:
A. Cyanmethemoglobin
B. Methemoglobin
C. Oxyhaemoglobin
D. Acid hematin
Answer: D
11. Reagent used in Sahli’s method is:
A. Drabkin’s reagent
B. Sodium azide
C. 0.1 N Hydrochloric acid
D. Ammonium hydroxide
Answer: C
12. Main disadvantage of Sahli’s method is:
A. Expensive
B. Toxic reagent
C. Subjective color matching
D. Time consuming
Answer: C
13. Reference method recommended by WHO for hemoglobin estimation is:
A. Sahli’s method
B. Oxyhaemoglobin method
C. Cyanmethemoglobin method
D. Azidemethemoglobin method
Answer: C
14. Cyanmethemoglobin method uses which reagent?
A. Sahli reagent
B. Drabkin’s reagent
C. Sodium citrate
D. EDTA
Answer: B
15. Cyanmethemoglobin absorbance is measured at:
A. 400 nm
B. 480 nm
C. 540 nm
D. 620 nm
Answer: C
16. Drabkin’s reagent contains:
A. Potassium oxalate
B. Sodium azide only
C. Potassium ferricyanide and potassium cyanide
D. Hydrochloric acid
Answer: C
17. Major drawback of cyanmethemoglobin method is:
A. Low accuracy
B. Subjective error
C. Presence of toxic cyanide
D. Cannot measure hemoglobin
Answer: C
18. Oxyhaemoglobin method measures hemoglobin as:
A. Acid hematin
B. Cyanmethemoglobin
C. Oxyhaemoglobin
D. Methemoglobin
Answer: C
19. Oxyhaemoglobin method is less accurate because:
A. Uses cyanide
B. Measures only oxyhaemoglobin
C. Requires automation
D. Is time consuming
Answer: B
20. Safer alternative to cyanmethemoglobin method is:
A. Sahli’s method
B. Oxyhaemoglobin method
C. Azidemethemoglobin method
D. Haldane method
Answer: C
21. Azidemethemoglobin method forms:
A. Cyanmethemoglobin
B. Acid hematin
C. Azidemethemoglobin
D. Oxyhaemoglobin
Answer: C
22. Azidemethemoglobin method is commonly used in:
A. Sahli apparatus
B. Blood banks
C. Automated hematology analyzers
D. Field surveys
Answer: C
23. Advantage of azidemethemoglobin method is:
A. Very cheap
B. Visual matching
C. Cyanide-free and safe
D. No instrument needed
Answer: C
24. Sulfhemoglobin is not measured accurately by:
A. Sahli’s method
B. Cyanmethemoglobin method
C. Azidemethemoglobin method
D. Automated analyzers
Answer: C
25. Sample used for hemoglobin estimation is:
A. Serum
B. Plasma
C. Whole blood
D. Urine
Answer: C
26. Anticoagulant used for automated Hb estimation is:
A. Sodium citrate
B. Heparin
C. EDTA
D. Oxalate
Answer: C
27. Automated hematology analyzers estimate hemoglobin by:
A. Visual color comparison
B. Gravimetric method
C. Photometric method
D. Titration
Answer: C
28. Major advantage of automated analyzers is:
A. Low cost
B. Manual calculation
C. High accuracy and speed
D. No reagents required
Answer: C
29. Automated analyzers provide:
A. Only hemoglobin value
B. Only RBC count
C. Complete blood count
D. Only WBC count
Answer: C
30. Hemoglobin estimation is especially important in:
A. Hypertension
B. Diabetes mellitus
C. Anemia
D. Hyperlipidemia
Answer: C
31. Hemoglobin estimation is routinely done in:
A. Blood sugar test
B. Urine analysis
C. Antenatal screening
D. ECG
Answer: C
32. Normal hemoglobin level in newborn is:
A. 8–10 g/dL
B. 10–12 g/dL
C. 12–14 g/dL
D. 16–20 g/dL
Answer: D
33. Hemoglobin estimation helps to assess:
A. Renal function
B. Oxygen-carrying capacity
C. Liver enzymes
D. Immune status
Answer: B
34. Color matching error is mainly seen in:
A. Cyanmethemoglobin method
B. Automated analyzers
C. Sahli’s method
D. Azide method
Answer: C
35. Hemoglobin is an example of:
A. Enzyme
B. Hormone
C. Glycoprotein
D. Metalloprotein
Answer: D
36. Iron in hemoglobin is present in which form?
A. Ferric (Fe³⁺)
B. Ferrous (Fe²⁺)
C. Ferritin
D. Hemosiderin
Answer: B
37. Hemoglobin estimation is useful for monitoring:
A. Antibiotic therapy
B. Response to anemia treatment
C. Blood pressure
D. Blood sugar
Answer: B
38. Which method is least accurate?
A. Automated analyzer
B. Cyanmethemoglobin
C. Azidemethemoglobin
D. Sahli’s method
Answer: D
39. Hemoglobin estimation should be avoided in which sample?
A. Fresh blood
B. EDTA blood
C. Clotted blood
D. Capillary blood
Answer: C
40. High hemoglobin value may be seen in:
A. Chronic blood loss
B. Iron deficiency
C. Dehydration
D. Pregnancy
Answer: C
41. Hemoglobin estimation in blood donation is done to:
A. Check blood group
B. Detect infection
C. Prevent anemia in donor
D. Measure platelet count
Answer: C
42. Hemoglobinometry mainly reflects:
A. RBC size
B. RBC shape
C. RBC oxygen-carrying function
D. RBC lifespan
Answer: C
43. Hemoglobin estimation is a:
A. Biochemical test
B. Hematological test
C. Immunological test
D. Microbiological test
Answer: B
44. Which method uses visual comparison?
A. Automated analyzer
B. Cyanmethemoglobin
C. Sahli’s method
D. Azidemethemoglobin
Answer: C
45. Azidemethemoglobin absorbance is measured around:
A. 450 nm
B. 500 nm
C. 570 nm
D. 620 nm
Answer: C
46. Most commonly used method in modern labs is:
A. Sahli’s method
B. Oxyhaemoglobin method
C. Automated analyzer
D. Haldane method
Answer: C
47. Hemoglobin estimation helps in diagnosing:
A. Leukemia
B. Anemia
C. Thrombocytopenia
D. Hemophilia
Answer: B
48. Hemoglobin is synthesized in:
A. Liver
B. Bone marrow
C. Spleen
D. Kidney
Answer: B
49. Which method is suitable for field surveys?
A. Automated analyzer
B. Cyanmethemoglobin
C. Sahli’s method
D. Azidemethemoglobin
Answer: C
50. Haemoglobinometry is best described as:
A. Qualitative test
B. Semi-quantitative test
C. Quantitative test
D. Screening test only
Answer: C