
AIM: Determination of Erythrocyte sedimentation rate (ESR)
Principle
- The ESR is based on the principle of gravity and the aggregation tendency of erythrocytes.
- In normal blood, erythrocytes have a negative charge, which causes them to repel each other and settle slowly.
- However, the acute phase increases in the bloodstream when inflammatory processes occur.
- These proteins cause erythrocytes to lose their negative charge and form rouleaux stacks, which settle faster due to increased density.
- The ESR reflects the extent of inflammation, where a faster settling rate correlates with more inflammation.
Methods
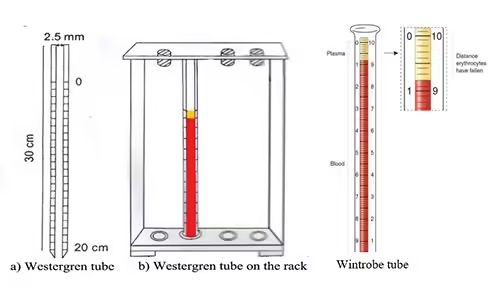
Westergren Method
Materials Required
- Blood with sodium citrate
- Westergren tube
- Rack/Stand
- Pipette
- Timer
Procedure
- Blood Collection:
- Collect 2 mL of venous blood from the patient and mix it with 0.5 mL of sodium citrate (3.8%) in a collection tube. The blood should be mixed gently to prevent clotting without causing hemolysis.
- Filling the Westergren Tube:
- Place the anticoagulated blood in the Westergren tube, using a pipette, up to the zero mark (0 mm).
- Ensure no air bubbles are present in the tube, as air bubbles can interfere with the accuracy of the reading.
- Placing the Tube in the Stand:
- Place the tube vertically in the rack or stand. Ensure the tube is upright and undisturbed. Any tilting or movement can alter the sedimentation rate.
- Sedimentation Time:
- Allow the blood to sediment for exactly 1 hour at room temperature (18-25°C). External factors like vibrations, temperature changes, or light exposure should be avoided during this time, as they may affect the result.
- Reading the ESR:
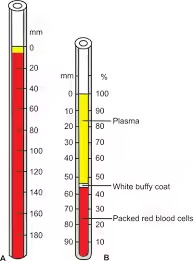
- After 1 hour, measure the distance in millimeters from the zero mark to the top of the red blood cell column. This distance represents the ESR in mm/hour.
- If sedimentation is unusually high or low, recheck the process for any errors or interference.
Normal ESR Values
- Men:
- Under 50 years: 0-15 mm/hour
- Over 50 years: 0-20 mm/hour
- Women:
- Under 50 years: 0-20 mm/hour
- Over 50 years: 0-30 mm/hour
- Children: 0-10 mm/hour
- Newborns: 0-2 mm/hour
- Pregnant women May show values up to 20-50 mm/hour, especially during the second and third trimesters due to physiological changes.
Wintrobe Method
Materials Required
- Wintrobe tube
- Anticoagulant: EDTA blood
- Rack/Stand
- Pipette
- Timer
Procedure
- Blood Collection:
- Draw approximately 1-2 mL of venous blood from the patient into an anticoagulant (EDTA or sodium citrate) tube. Mix gently to avoid hemolysis or clotting.
- Filling the Wintrobe Tube:
- Transfer the anticoagulated blood to the Wintrobe tube using a pipette to the ESR scale’s zero mark. Ensure no air bubbles are present, as this can affect the accuracy of the result.
- Positioning the Tube:
- Place the Wintrobe tube vertically in a stand. Ensure the tube is perfectly upright because any tilt can affect the erythrocyte sedimentation rate.
- Sedimentation Time:
- Leave the tube undisturbed at room temperature (18-25°C) for exactly 1 hour. External vibrations or temperature fluctuations should be avoided, as they can impact the sedimentation rate.
- Reading the ESR:
- After 1 hour, measure the distance in millimeters that the red blood cells have fallen from the zero mark to the top of the column of red blood cells.
- This distance represents the ESR in mm/hour.
- Recording the Results:
- Report the result as the ESR in mm/hour. A higher sedimentation rate indicates a greater degree of inflammation.
Normal Values
- Men: 0-9 mm/hour
- Women: 0-20 mm/hour
- Children: 0-10 mm/hour
Advantages of the Wintrobe Method
- Less blood required: This method is often used when a smaller blood sample is available (such as in pediatric patients).
- Simultaneous hematocrit measurement: Using the same blood sample, the Wintrobe tube can also measure hematocrit (the proportion of blood that consists of red blood cells).
Disadvantages of the Wintrobe Method
- Less sensitive to high ESR values: The shorter tube means this method is not as effective at measuring very high ESR levels (>100 mm/hour), making it less sensitive for detecting significant inflammatory processes.
- Standardisation: The Westergren method is more commonly used and is better standardised, which is why many clinicians prefer it.
Clinical Significance
The ESR test is a nonspecific marker, meaning it cannot diagnose specific diseases, but it is a valuable indicator of the presence and extent of inflammation in the body. ESR values can be elevated or decreased in a wide range of conditions:
Elevated ESR (conditions causing faster red cell sedimentation)
- Infections: Bacterial infections (e.g., pneumonia, tuberculosis), abscesses, and chronic infections.
- Inflammatory diseases:
- Autoimmune diseases (e.g., rheumatoid arthritis, systemic lupus erythematosus)
- Vasculitis (e.g., temporal arteritis)
- Inflammatory bowel diseases (e.g., Crohn’s disease, ulcerative colitis)
- Cancers:
- Malignancies (e.g., lymphoma, multiple myeloma, metastatic cancers)
- Chronic diseases:
- Chronic kidney disease
- Endocarditis
- Polymyalgia rheumatica
- Pregnancy: Due to increased fibrinogen levels.
Decreased ESR (conditions causing slower red cell sedimentation)
- Polycythemia: Increased number of red blood cells can cause a low ESR.
- Sickle cell anaemia: The abnormal shape of red blood cells prevents rouleaux formation, resulting in decreased ESR.
- Heart failure: Chronic heart conditions can sometimes result in a decreased ESR.
- Hyperviscosity syndromes: Conditions that increase blood thickness, such as Waldenstrom’s macroglobulinemia.
Factors Influencing ESR
A wide range of factors, both physiological and pathological, influences ESR. Understanding these factors is essential for accurate interpretation of ESR results:
-
Physiological Factors
- Age: ESR tends to increase with age, especially in the elderly, due to physiological changes, even without disease.
- Gender: Women typically have higher ESR values than men due to hormonal differences, especially during menstruation and pregnancy.
- Pregnancy: ESR increases significantly in pregnancy, particularly during the second and third trimesters. This is due to increased fibrinogen levels and other physiological changes.
- Menstruation: Due to hormonal variations, ESR may rise slightly during the menstrual cycle.
- Haemoglobin concentration: Anemia can elevate ESR as there are fewer red blood cells, making it easier for them to form rouleaux and sediment faster.
-
Pathological Factors
- Inflammation: Acute-phase proteins (e.g., fibrinogen, C-reactive protein, immunoglobulins) produced during inflammation promote rouleaux formation, increasing ESR.
- Infections: Bacterial and chronic infections significantly raise ESR due to the inflammatory response.
- Chronic diseases: Conditions like rheumatoid arthritis, systemic lupus erythematosus, and malignancies can increase ESR due to chronic inflammation.
- Cancer: Some cancers (e.g., lymphoma, multiple myeloma, metastatic tumours) cause elevated ESR due to the presence of cancer-related inflammation and tissue damage.
- Kidney disease: chronic kidney disease can cause elevated ESR due to the buildup of inflammatory proteins and other metabolic factors.
- Heart failure: Congestive heart failure can lower ESR, likely due to reduced fibrinogen levels and changes in blood viscosity.
- Polycythemia: Increased red blood cells in polycythemia can reduce ESR because the cells crowd the plasma and hinder rouleaux formation.
-
Technical and Environmental Factors
- Tilt of the ESR tube: A tube that is not perfectly vertical will cause the red blood cells to settle faster, artificially elevating the ESR.
- Temperature: ESR is temperature-sensitive. At higher temperatures, ESR may increase, while lower temperatures can slow sedimentation.
- Sample processing time: ESR measurements must be taken within 2 hours of blood collection. Delayed measurement can cause falsely elevated ESR due to blood changes over time.
- Tube size: The diameter and length of the ESR tube (Westergren vs. Wintrobe tubes) influence the sedimentation rate.
- Clotting: Inadequate anticoagulation or improper mixing can cause clumping of red blood cells, falsely lowering ESR.