Introduction
Coccidioides is a dimorphic fungi that causes coccidioidomycosis, also known as Valley Fever. The disease primarily affects the lungs but can disseminate to other organs in severe cases. There are two primary pathogenic species:
-
- Coccidioides immitis
- Coccidioides posadasii
These fungi are thermally dimorphic:
-
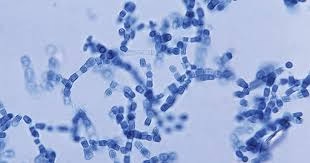
- Environmental form: Mold with arthroconidia (infectious spores).
- Host form: Spherules that produce endospores in tissues.
Key Features:
-
- Infection occurs via inhalation of arthroconidia.
- Coccidioidomycosis ranges from asymptomatic to severe, disseminated disease.
- It is considered one of the most virulent fungal infections, as only a few spores are needed to cause infection.
Epidemiology
- Geographic Distribution:
-
- Endemic in arid and semi-arid regions of the Americas:
- Southwestern United States: California (San Joaquin Valley), Arizona, Nevada, New Mexico, Texas, and Utah.
- Parts of Mexico and Central and South America.
- Found in desert soils with low rainfall and high temperatures.
- Endemic in arid and semi-arid regions of the Americas:
-
- Reservoir:
-
- The fungi live in the soil and survive as saprophytic molds.
- Arthroconidia are released into the air when soil is disturbed by wind, construction, or farming.
-
- Transmission:
-
- Inhalation of arthroconidia is the primary mode of infection.
- Rarely, direct inoculation into the skin can occur through trauma.
- No person-to-person transmission.
-
- At-Risk Populations:
-
- People living in or traveling to endemic areas.
- Occupations with high exposure to soil (e.g., construction workers, farmers, military personnel).
- Immunocompromised individuals (e.g., HIV/AIDS, organ transplant recipients).
-
- Incidence:
-
- In endemic areas, infection rates can be as high as 30–60% over a lifetime.
- Outbreaks are associated with environmental disturbances (e.g., dust storms and earthquakes).
-
Pathogenesis
The pathogenicity of Coccidioides involves its ability to evade immune defenses and survive in host tissues.
- Inhalation of Arthroconidia:
-
- Arthroconidia are small (2–5 µm), making them easily aerosolized and inhaled.
- Once in the lungs, they resist clearance by mucociliary mechanisms.
-
- Transition to Spherules:
-
- In the host (at 37°C), arthroconidia transform into spherules.
- Spherules enlarge (up to 100 µm) and produce endospores, released upon spherule rupture.
-
- Immune Evasion:
-
- Spherules are resistant to phagocytosis due to their size.
- Endospores spread locally or hematogenously to other tissues.
-
- Host Immune Response:
-
- Effective immunity requires a Th1 response (cell-mediated immunity), with the production of IFN-γ and activation of macrophages.
- Th2 responses are associated with poor outcomes and dissemination.
-
- Granuloma Formation:
-
- Granulomas form in response to fungal antigens, containing the infection in immunocompetent hosts.
- In immunosuppressed hosts, the fungus can replicate unchecked, leading to dissemination.
-
Clinical Manifestations
The clinical spectrum of coccidioidomycosis depends on the host’s immune status and the infectious dose.
- Primary Pulmonary Coccidioidomycosis:
-
- Most common presentation.
- Incubation period: 1–3 weeks after exposure.
- Asymptomatic: ~60% of cases.
- Symptomatic cases:
- Flu-like symptoms: Fever, cough, chest pain, fatigue, headache, myalgia.
- Erythema nodosum or erythema multiforme (hypersensitivity reactions, common in women).
- Resolves spontaneously in most immunocompetent individuals.
- Chronic Pulmonary Coccidioidomycosis:
-
- Develops in ~5% of symptomatic cases.
- Mimics tuberculosis with symptoms like:
- Cough, hemoptysis, night sweats, weight loss, and pulmonary cavitations.
- Disseminated Coccidioidomycosis:
-
- Occurs in ~1% of cases but more common in:
- Immunocompromised individuals.
- Pregnant women (especially during the third trimester).
- Ethnic groups: Filipinos, African Americans, Native Americans.
- Common sites of dissemination:
- Skin: Papules, plaques, or ulcers resembling bacterial cellulitis.
- Bones and joints: Osteomyelitis, arthritis.
- CNS: Meningitis (often fatal if untreated).
- Other organs: Liver, spleen, or genitourinary tract.
- Occurs in ~1% of cases but more common in:
Laboratory Diagnosis
The diagnosis of coccidioidomycosis involves a combination of clinical, radiologic, and laboratory findings.
- Microscopy
-
- Specimens: Sputum, BAL fluid, pleural fluid, or biopsies from infected tissue.
- Stains:
- KOH preparation: Rapid identification of fungal elements.
- Gomori methenamine silver (GMS) or PAS: Highlight fungal spherules.
Findings:
-
- Spherules (10–100 µm in diameter) containing multiple endospores (2–5 µm).
- Thick-walled spherules are diagnostic of Coccidioides.
- Culture
-
- Specimens: Respiratory secretions, tissue biopsies, or body fluids.
- Growth conditions:
- Media: Sabouraud dextrose agar or other fungal media.
- Temperature: Grows as a mold at 22–25°C.
- Growth time: 3–10 days (rapid for fungi).
Morphology:
-
- At 22°C: Hyphae with arthroconidia (barrel-shaped spores with alternating empty cells).
Safety Precautions:
-
- Cultures are highly infectious due to the production of arthroconidia. Handling must occur in a biosafety level 3 (BSL-3) laboratory.
- Serology
Serologic testing is a cornerstone of diagnosis, particularly for disseminated or chronic disease.
Tests Available:
-
- Enzyme Immunoassay (EIA):
- Detects IgM (acute infection) and IgG (chronic or disseminated infection).
- High sensitivity but some cross-reactivity with other fungi.
- Immunodiffusion (ID):
- Detects IgM and IgG antibodies.
- More specific than EIA.
- Complement Fixation (CF):
- Measures IgG titers to assess disease severity and progression.
- High titers (>1:16) indicate disseminated disease.
- Enzyme Immunoassay (EIA):
- Antigen Detection
-
- Detects Coccidioides antigens in urine, serum, or cerebrospinal fluid (CSF).
- Useful for rapid diagnosis, especially in immunocompromised patients.
- Cross-reactivity with Histoplasma and Blastomyces can occur.
- Histopathology
-
- A biopsy of affected tissue shows granulomas and spherules.
- Stains: H&E, GMS, or PAS.
- Molecular Testing (PCR)
-
- PCR assays can detect Coccidioides DNA in clinical specimens.
- Offers a rapid and specific diagnosis