Table of Contents
ToggleThrombocyte Disorder
Thrombocyte disorders are disorders affecting platelets (thrombocytes), the blood cells primarily involved in clot formation. These disorders can result in either a low platelet count (thrombocytopenia), a high platelet count (thrombocytosis), or impaired platelet function, all of which can lead to abnormal bleeding or clotting.
Thrombocytopenia
Thrombocytopenia occurs when the platelet count falls below the normal range, typically defined as less than 150,000 platelets per microliter of blood. Thrombocytopenia can result from several underlying causes, and the severity of symptoms depends on the degree of platelet reduction.
Causes of Thrombocytopenia:
-
Decreased Platelet Production:
-
Bone Marrow Disorders: Conditions like leukemia, myelodysplastic syndromes, aplastic anemia, or myelofibrosis reduce the bone marrow’s ability to produce platelets.
-
Viral Infections: Viral infections like HIV, Epstein-Barr virus (EBV), hepatitis, or cytomegalovirus (CMV) can suppress platelet production.
-
Chemotherapy or Radiation Therapy: These treatments often damage bone marrow, reducing platelet production.
-
Nutritional Deficiencies: Deficiencies in vitamin B12 or folic acid can impair platelet production.
-
-
Increased Platelet Destruction:
-
Immune-mediated Conditions (Autoimmune): Disorders like immune thrombocytopenic purpura (ITP), where the immune system produces antibodies that destroy platelets.
-
Drug-induced Thrombocytopenia: Medications such as heparin, quinine, penicillin, and sulfonamides can induce platelet destruction via immune mechanisms.
-
Infections: Certain bacterial or viral infections can trigger platelet destruction, as seen in dengue fever or sepsis.
-
Disseminated Intravascular Coagulation (DIC): In conditions where abnormal clotting occurs throughout the bloodstream, platelets are consumed in the formation of microclots, leading to a low platelet count.
-
-
Platelet Sequestration:
-
Splenomegaly (Enlarged Spleen): Conditions like cirrhosis or infections can cause the spleen to become enlarged, leading to increased sequestration and removal of platelets.
-
Symptoms of Thrombocytopenia:
-
Bruising (easy or spontaneous)
-
Petechiae (small red or purple spots under the skin)
-
Prolonged bleeding from minor cuts or after medical procedures
-
Excessive bleeding during menstruation (in females)
-
Gum bleeding or nosebleeds
-
Fatigue or weakness in severe cases
Thrombocytosis
Thrombocytosis refers to an abnormally high platelet count, generally above 450,000 platelets per microliter. It is categorized into two types: primary (essential) and secondary (reactive).
Causes of Thrombocytosis:
-
Primary Thrombocytosis (Essential Thrombocythemia):
-
This is a myeloproliferative disorder where the bone marrow produces excessive platelets without an underlying cause. It’s often caused by mutations in genes like JAK2, CALR, or MPL.
-
It can increase the risk of thrombosis (formation of abnormal blood clots), which can lead to stroke, heart attack, or deep vein thrombosis (DVT).
-
Symptoms may be subtle or involve thrombotic events, such as:
-
Headaches
-
Dizziness
-
Chest pain
-
Visual disturbances
-
-
-
Secondary Thrombocytosis (Reactive Thrombocytosis):
-
This form of thrombocytosis is caused by an underlying condition such as:
-
Infections: Bacterial, viral, or fungal infections can increase platelet production as part of the body’s acute-phase response.
-
Inflammatory Disorders: Diseases like rheumatoid arthritis, inflammatory bowel disease (IBD), or systemic lupus erythematosus (SLE) can lead to elevated platelets.
-
Iron Deficiency Anemia: Low iron levels can trigger an increase in platelet production.
-
Surgical Recovery: Platelet counts often rise as part of the post-surgical recovery process.
-
Cancer: Malignancies, especially those involving the gastrointestinal tract or lung, can also lead to reactive thrombocytosis.
-
-
Symptoms of Thrombocytosis:
-
Thrombotic complications, such as stroke, heart attack, or deep vein thrombosis.
-
Fatigue
-
Headaches
-
Dizziness
-
Chest pain
-
Splenomegaly (in some cases)
Platelet Dysfunction Disorders
These disorders occur when platelets are present in normal numbers but are unable to function properly, resulting in poor clot formation and abnormal bleeding tendencies.
Causes of Platelet Dysfunction:
-
Inherited Platelet Dysfunction:
-
Glanzmann Thrombasthenia: An autosomal recessive disorder in which platelets lack the glycoprotein IIb/IIIa complex, leading to impaired platelet aggregation.
-
Bernard-Soulier Syndrome: Another autosomal recessive disorder, where platelets lack the GPIb-IX-V complex, preventing them from binding to von Willebrand factor (vWF) during the clotting process.
-
May-Hegglin Anomaly: A genetic condition where large platelets are present, and platelet function is defective, leading to bleeding tendencies.
-
Storage Pool Disorders: Genetic defects in the platelet granules, impairing the release of clotting factors like ADP and serotonin.
-
-
Acquired Platelet Dysfunction:
-
Medications: Drugs like aspirin, NSAIDs, and clopidogrel inhibit platelet function and are used therapeutically to reduce the risk of thrombosis, but they may lead to bleeding complications.
-
Uremia: In patients with kidney failure, elevated urea levels can impair platelet function, leading to bleeding.
-
Liver Disease: In chronic liver diseases (e.g., cirrhosis), platelet dysfunction occurs due to impaired production of clotting factors and platelet aggregation defects.
-
Autoimmune Conditions: Disorders like systemic lupus erythematosus (SLE) can impair platelet function due to the presence of circulating antibodies.
-
Symptoms of Platelet Dysfunction:
-
Easy bruising
-
Prolonged bleeding from cuts or surgery
-
Epistaxis (nosebleeds)
-
Gingival bleeding (bleeding from the gums)
-
Heavy menstrual periods
-
Excessive bleeding following minor trauma
Laboratory Diagnosis
Laboratory tests are essential in diagnosing thrombocyte disorders, identifying the underlying cause, and determining the appropriate treatment. Here’s a more in-depth look at the tests used:
1. Complete Blood Count (CBC) with Platelet Count
-
Platelet Count: The primary test for thrombocytopenia or thrombocytosis. A platelet count less than 150,000 indicates thrombocytopenia, and above 450,000 suggests thrombocytosis.
-
Mean Platelet Volume (MPV): A measure of the average size of platelets. Large platelets may indicate increased production, which can be seen in conditions like immune thrombocytopenic purpura (ITP) or primary thrombocytosis.
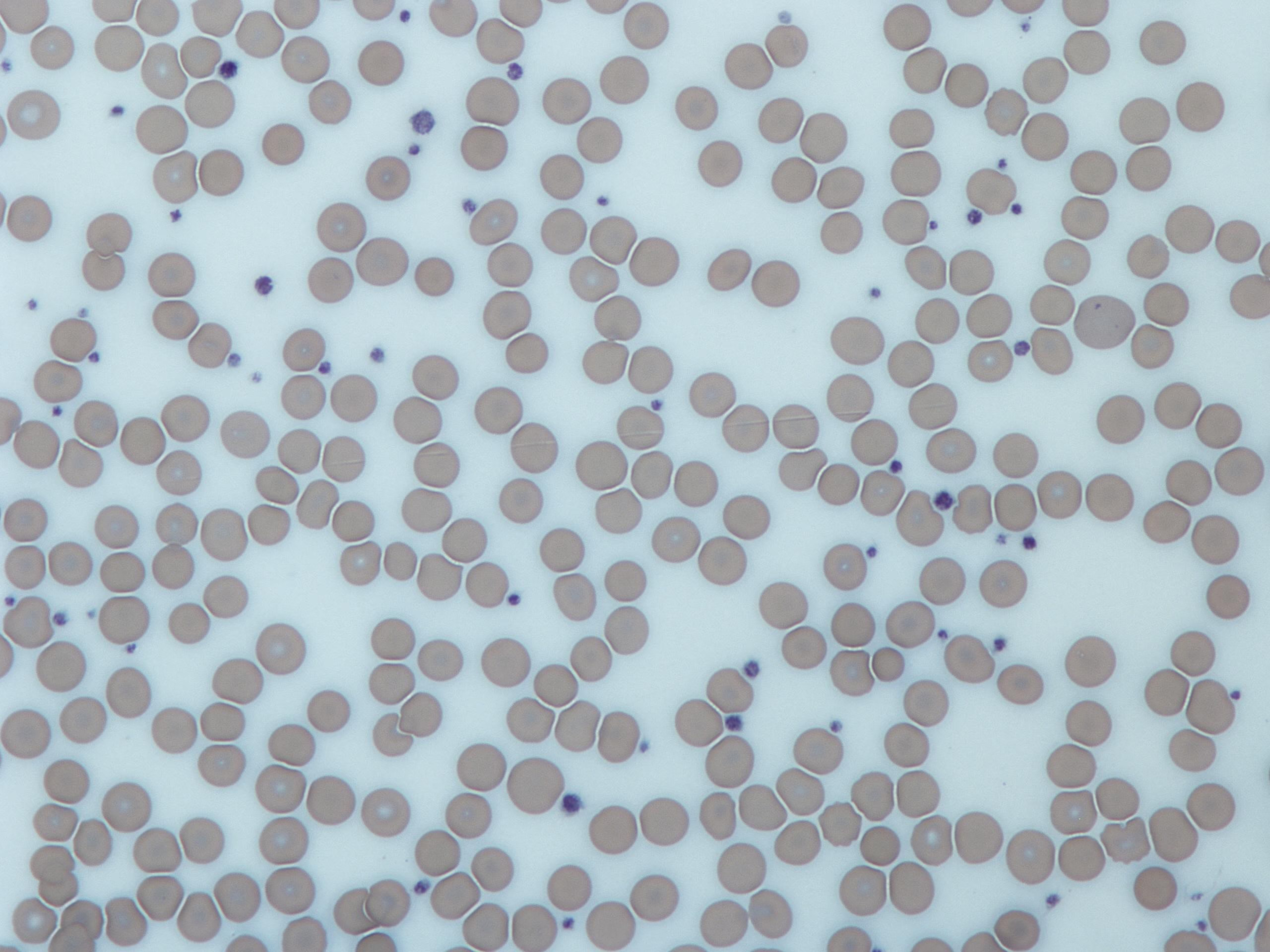
2. Peripheral Blood Smear
-
Provides a visual assessment of platelets and other blood cells. In thrombocytopenia, you might see giant platelets or platelet clumps.
-
In thrombocytosis, a blood smear can reveal abnormal platelet shapes or sizes.
-
Can also detect abnormal white blood cells in conditions like leukemia or myelodysplastic syndromes.
3. Bone Marrow Aspiration/Biopsy
-
A bone marrow biopsy is performed if a primary bone marrow disorder (e.g., leukemia, aplastic anemia, myelofibrosis) is suspected.
-
It helps to assess the megakaryocytes (platelet-producing cells) and provides insight into whether platelet production is decreased, increased, or abnormal.
4. Platelet Function Tests
-
Platelet Aggregation Studies: Evaluate how well platelets clump together when exposed to various agonists like ADP, collagen, and epinephrine. Defective aggregation suggests platelet dysfunction.
-
PFA-100 (Platelet Function Analyzer): This test simulates conditions in blood vessels and evaluates platelet function in response to collagen and epinephrine. It is commonly used to detect platelet dysfunction in bleeding disorders.
5. Thromboelastography (TEG)
-
This is an advanced test that assesses the overall coagulation status, including platelet function. It provides real-time data on clot formation, strength, and dissolution.
6. Immunological Tests
-
Anti-platelet Antibody Tests: Used to diagnose immune thrombocytopenic purpura (ITP), where antibodies target and destroy platelets.
-
Flow Cytometry: Used to evaluate platelet surface markers and defects in platelet receptors, especially in hereditary platelet disorders like Glanzmann thrombasthenia.
7. Coagulation Profile
-
Measures clotting factors like PT, aPTT, and fibrinogen. While these tests mainly assess the coagulation pathway, they can be useful in ruling out concurrent clotting factor deficiencies or other bleeding disorders.
8. Genetic Testing
-
Genetic Testing is used to confirm inherited platelet dysfunctions like Glanzmann thrombasthenia, Bernard-Soulier syndrome, or other genetic platelet disorders.