Introduction
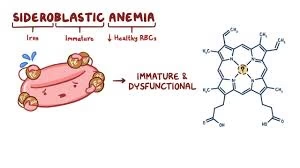
- Anaemia is a condition where the blood does not have enough healthy red blood cells or enough haemoglobin to carry oxygen.
- There are many types of anaemia, and each type has a different cause.
- One special and important type is called sideroblastic anaemia.
- In this condition, the problem is not the lack of iron itself, but the body’s inability to use the iron properly to make haemoglobin.
- Iron is present in the body, sometimes even in large amounts, but it gets trapped inside immature red blood cells.
- Because of this, the red blood cells cannot form normally, and the person develops anaemia.
Why is it called “Sideroblastic”?
-
“Sidero” means iron.
-
“Blast” refers to immature developing cells (in this case, young red blood cells in the bone marrow).
-
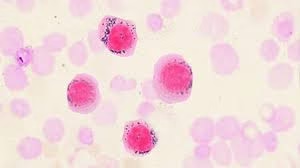
In sideroblastic anaemia, when doctors look at the bone marrow under the microscope and stain it with a special dye (Prussian blue), they see iron collected around the nucleus of the red cell precursors. These abnormal cells are called ring sideroblasts.
-
So, the name comes from the presence of these iron-loaded immature red blood cells.
Normal Iron and Haemoglobin Formation
To understand the disease, let’s quickly revise how haemoglobin is normally made:
-
Iron enters the body from food and is absorbed in the small intestine.
-
It is transported in the blood with the help of a protein called transferrin.
-
Iron goes to the bone marrow, where new red blood cells are formed.
-
Inside red blood cell precursors, iron is inserted into a molecule called protoporphyrin to form haem.
-
Haem then combines with globin proteins to form haemoglobin, which carries oxygen.
What Goes Wrong in Sideroblastic Anaemia?
In sideroblastic anaemia:
-
The body has iron, but it cannot be inserted properly into protoporphyrin to form haem.
-
This blockage may happen because of defective enzymes, toxins, drugs, or genetic mutations.
-
As a result, iron accumulates in the mitochondria of developing red cells.
-
These mitochondria form a ring around the nucleus, and this is visible as ring sideroblasts in the bone marrow.
-
Because haemoglobin is not formed properly, red cells become abnormal, small, and pale (microcytic hypochromic) or sometimes even large (macrocytic) depending on the cause.
Types of Sideroblastic Anaemia
There are two main categories:
1. Hereditary (Genetic) Sideroblastic Anaemia
-
Caused by mutations passed from parents to children.
-
The most common form is X-linked sideroblastic anaemia, due to mutation in the ALAS2 gene.
-
ALAS2 is an enzyme needed for the first step of haem production. This enzyme also requires Vitamin B6 (pyridoxine) as a cofactor.
-
Some forms respond to high doses of Vitamin B6.
2. Acquired Sideroblastic Anaemia
-
More common than hereditary.
-
It can be primary (part of a bone marrow disorder) or secondary (due to other causes).
a) Primary (Clonal)
-
-
Usually linked to myelodysplastic syndromes (MDS), especially a type called “Refractory anaemia with ring sideroblasts (RARS)”.
-
Common in older adults.
-
b) Secondary Causes
-
-
Alcoholism – alcohol damages mitochondria and blocks haem synthesis.
-
Drugs – e.g., isoniazid (TB medicine), chloramphenicol, linezolid.
-
Toxins – especially lead poisoning (blocks enzymes ALA dehydratase and ferrochelatase).
-
Nutritional deficiency – copper deficiency or zinc overload (zinc competes with copper).
-
Symptoms and Clinical Features
The symptoms depend on how severe the anaemia is and whether there is iron overload.
General symptoms of anaemia:
-
Fatigue and weakness
-
Shortness of breath, especially on exertion
-
Paleness of skin
-
Dizziness and headaches
-
Fast heart rate (palpitations)
Other possible findings:
-
Enlargement of the liver and spleen (due to iron deposition)
-
Symptoms of iron overload (secondary haemochromatosis) – diabetes, joint pains, skin darkening, heart failure, liver cirrhosis
-
In lead poisoning: abdominal pain, constipation, neurological problems, and blue line on gums
Laboratory Findings
Doctors use several tests to confirm sideroblastic anaemia:
-
Complete Blood Count (CBC):
-
Anaemia of varying severity.
-
Red blood cells may be microcytic (small), normocytic, or macrocytic depending on the cause.
-
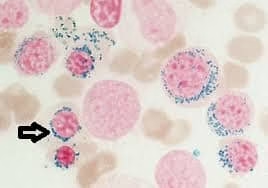
Blood smear may show a dimorphic picture – both small pale cells and normal/red cells together.
-
Basophilic stippling (tiny dots in red cells) in lead poisoning.
-
-
Iron Studies:
-
Serum iron: High
-
Serum ferritin: High
-
Total Iron Binding Capacity (TIBC): Low or normal
-
Transferrin saturation: Increased
👉 This is the opposite of iron deficiency anaemia, where iron and ferritin are low and TIBC is high.
-
-
Bone Marrow Examination:
-
Hypercellular marrow (increased activity).
-
Many immature red cells with iron-laden mitochondria are seen as ring sideroblasts with Prussian blue stain.
-
This is the diagnostic feature.
-
-
Other Investigations:
-
Blood lead levels (if poisoning suspected).
-
Genetic testing (for hereditary cases).
-
Copper and zinc levels if deficiency or excess is suspected.
-
Treatment
The treatment depends on the underlying cause.
General Measures:
-
Identify and remove the cause (stop alcohol, remove offending drug, treat lead poisoning, correct copper deficiency).
Specific Treatments:
-
Vitamin B6 (Pyridoxine) therapy:
-
Works especially in hereditary X-linked sideroblastic anaemia because the defective enzyme (ALAS2) requires B6.
-
Some patients improve significantly.
-
-
Blood transfusions:
-
Given when anaemia is severe and symptomatic.
-
Risk: repeated transfusions cause iron overload.
-
-
Iron chelation therapy:
-
To remove excess iron from the body (e.g., with drugs like deferoxamine, deferiprone, or deferasirox).
-
Prevents damage to organs like liver, heart, and pancreas.
-
-
Erythropoietin or newer drugs (like luspatercept):
-
Used in myelodysplastic syndromes to stimulate red cell production.
-
-
Bone marrow transplant:
-
Rarely used, but can be curative in severe congenital cases.
-
Comparison with Iron Deficiency Anaemia
Since both conditions may show microcytic hypochromic cells, they are often confused. Here is a simple comparison:
| Feature | Sideroblastic Anaemia | Iron Deficiency Anaemia |
|---|---|---|
| Serum Iron | High | Low |
| Ferritin | High | Low |
| TIBC | Low/Normal | High |
| Bone Marrow | Ring sideroblasts | No ring sideroblasts |
| RBC Picture | Dimorphic, stippling | Uniformly small, pale |
| Response to Iron Therapy | No | Yes |
Prognosis
-
Depends on the cause.
-
Hereditary cases may live normally with pyridoxine therapy.
-
Secondary cases improve if the toxin/deficiency is corrected.
-
Myelodysplastic syndromes have variable prognosis; some may progress to leukaemia.
-
Risk of iron overload is a major complication, which can damage liver, heart, and endocrine organs if not managed.