Introduction
-
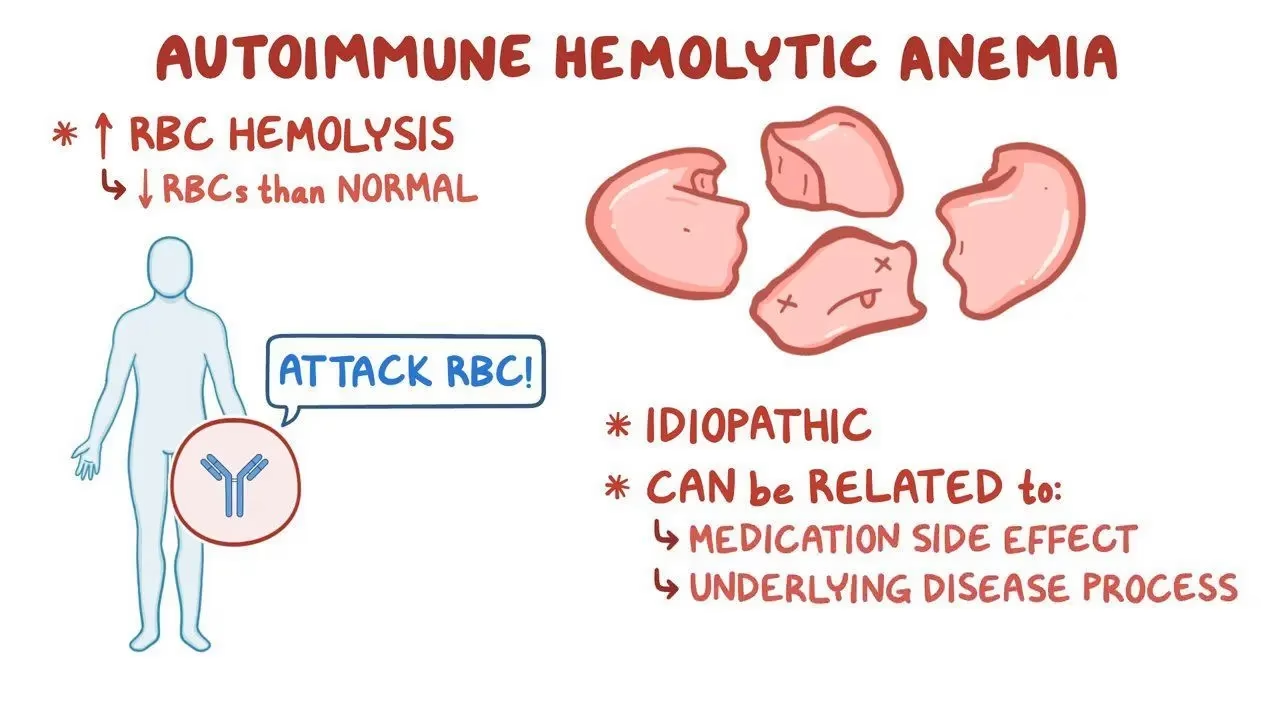
Acquired Autoimmune Hemolytic Anaemia (AIHA) is a rare blood disorder in which the immune system produces autoantibodies that attack and destroy red blood cells (RBCs), leading to premature hemolysis.
-
It is acquired, meaning it develops later in life rather than being inherited.
-
The destruction of RBCs results in anaemia and related symptoms.
Types of AIHA
There are three main types, based on the temperature at which the antibodies work best:
A. Warm AIHA
-
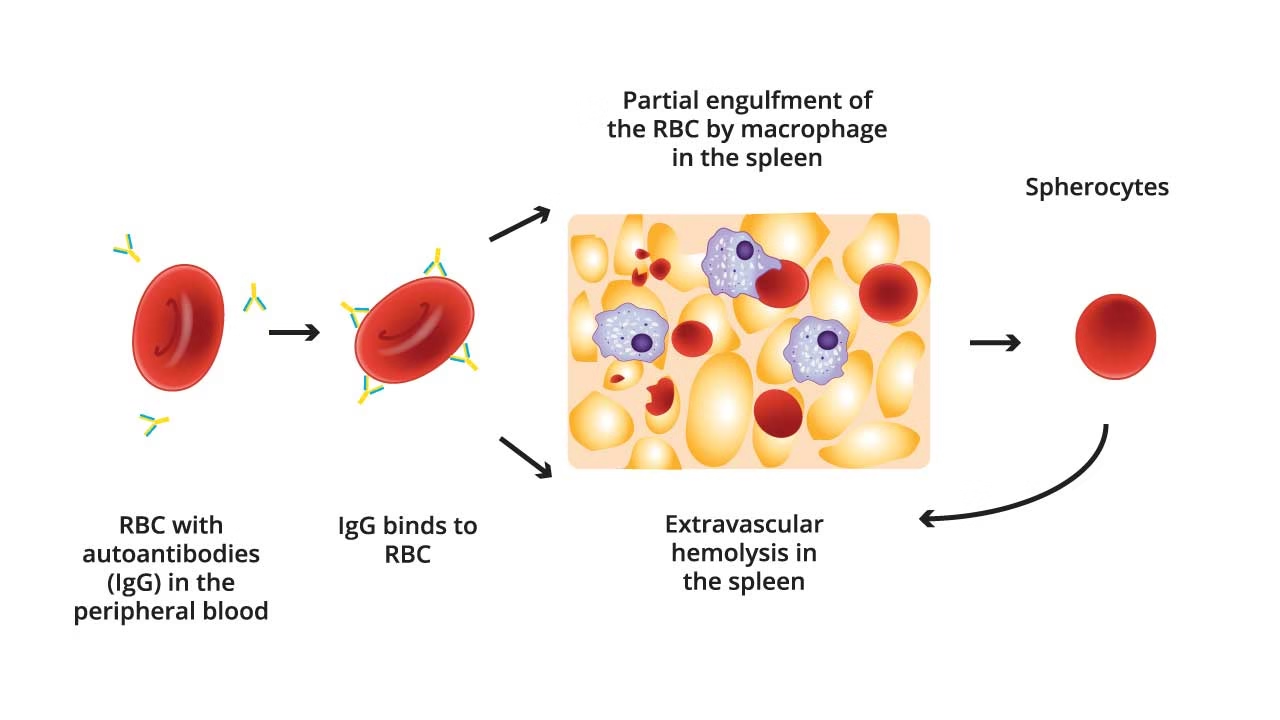
Most common (about 70–80% of cases).
-
Antibodies: IgG (sometimes IgA).
-
Best active at body temperature (37°C).
-
RBCs mainly destroyed in the spleen (extravascular hemolysis).
-
Associated with:
-
Autoimmune diseases (e.g., SLE, rheumatoid arthritis).
-
Blood cancers (CLL, lymphoma).
-
Medicines (methyldopa, penicillin).
-
-
Peripheral smear: spherocytes.
B. Cold AIHA (Cold Agglutinin Disease)
-
Antibodies: IgM.
-
Work best in cooler temperatures (<30°C).
-
Cause clumping (agglutination) of RBCs and complement activation.
-
RBCs destroyed in liver and circulation (intravascular and extravascular hemolysis).
-
Associated with:
-
Infections (Mycoplasma pneumoniae, EBV, HIV).
-
Lymphoid cancers.
-
-
Clinical feature: acrocyanosis (blue fingers/toes in cold).
C. Paroxysmal Cold Hemoglobinuria (PCH)
-
Very rare, usually in children after viral illness.
-
Antibody: Donath–Landsteiner (IgG).
-
Attacks RBCs when body rewarms after cold exposure.
-
Often self-limiting.
Causes of AIHA
-
Primary (Idiopathic): No clear underlying reason (about 50% of cases).
-
Secondary (due to other conditions):
-
Autoimmune diseases: SLE, rheumatoid arthritis.
-
Blood cancers: CLL, lymphoma.
-
Infections: EBV, HIV, Mycoplasma.
-
Drugs: penicillin, cephalosporins, methyldopa.
-
Symptoms
-
From anemia: fatigue, weakness, pale skin, dizziness, rapid heartbeat, shortness of breath.
-
From hemolysis: yellow eyes (jaundice), dark urine (hemoglobinuria), enlarged spleen, gallstones.
-
Warm AIHA: gradual tiredness, enlarged spleen.
-
Cold AIHA: cold hands/feet, bluish skin, Raynaud’s phenomenon, hemoglobin in urine after cold exposure.
-
Severe cases: chest pain, fainting, heart strain.
Diagnosis
Blood tests to confirm AIHA:
-
Complete Blood Count (CBC):
-
Low hemoglobin.
-
Often normal-sized (normocytic) RBCs.
-
-
Reticulocyte count: High (bone marrow trying to make more RBCs).
-
Peripheral smear:
-
Warm AIHA: spherocytes (small round RBCs).
-
Cold AIHA: RBC clumping (agglutination).
-
-
Biochemistry:
-
High indirect bilirubin (from RBC breakdown).
-
High LDH.
-
Low haptoglobin.
-
-
Direct Antiglobulin Test (DAT/Coombs test):
-
Positive in most patients.
-
IgG positive → Warm AIHA.
-
C3 positive → Cold AIHA.
-
Negative in rare cases (DAT-negative AIHA).
-
-
Special tests:
-
Cold agglutinin titer.
-
Donath–Landsteiner test (for PCH).
-
Tests for underlying disease (ANA, viral serology, blood cancer markers).
-
Treatment
Warm AIHA
-
First-line:
-
Steroids (Prednisone 1 mg/kg/day).
-
Works in most patients; later slowly reduced.
-
-
Second-line (if steroids fail):
-
Rituximab (anti-CD20 antibody).
-
Splenectomy (removing spleen).
-
-
Other options:
-
Immunosuppressants (azathioprine, cyclophosphamide, cyclosporine).
-
-
Blood transfusion: May be needed in severe anemia, but matching is difficult because of antibodies.
Cold AIHA
-
Avoid cold exposure (keep warm).
-
Rituximab is effective in many cases.
-
New drug: Sutimlimab (blocks complement system, approved for Cold AIHA).
-
Steroids usually not useful.
-
Plasmapheresis (blood filtering) in severe cases.
Paroxysmal Cold Hemoglobinuria (PCH)
-
Avoid cold exposure.
-
Supportive care, blood transfusion if needed.
-
Usually gets better by itself.
Complications
-
Severe anemia → heart failure, breathlessness.
-
Gallstones from bilirubin buildup.
-
Blood clots (rare but possible).
-
Infections after splenectomy.
Prognosis
-
Warm AIHA: Most patients respond to steroids but some relapse.
-
Cold AIHA: Often long-term, needs ongoing management.
-
PCH: Usually temporary in children.