Introduction
-
Prenatal diagnosis refers to medical tests performed during pregnancy to detect genetic, chromosomal, and congenital abnormalities in the fetus.
-
These diagnostic methods help identify inherited disorders and developmental defects before birth.
-
Advances in genetics, molecular biology, and imaging techniques have greatly improved the accuracy of prenatal diagnosis.
-
Early detection allows timely medical intervention, appropriate pregnancy management, and informed parental decision-making.
-
Prenatal diagnosis plays a crucial role in reducing neonatal morbidity and mortality associated with genetic diseases.
-
It also provides an opportunity for genetic counseling, helping families understand risks, prognosis, and future reproductive options.
-
With increasing awareness and availability of advanced tests, prenatal diagnosis has become an integral part of modern antenatal care.
Genetic Diseases
Prenatal diagnostic techniques help in early identification of a wide spectrum of genetic and congenital disorders. These diseases can be broadly classified into the following categories:
Chromosomal Disorders
These result from numerical or structural abnormalities of chromosomes and are among the most commonly detected prenatal conditions.
-
Down syndrome (Trisomy 21)
-
Edwards syndrome (Trisomy 18)
-
Patau syndrome (Trisomy 13)
-
Turner syndrome (45,X)
-
Klinefelter syndrome (47,XXY)
-
Structural rearrangements (deletions, duplications, translocations)
Detected by:
-
NIPT
-
Amniocentesis
-
Chorionic villus sampling
-
Karyotyping / FISH
Single-Gene (Mendelian) Disorders
These are caused by mutations in a single gene and follow Mendelian inheritance patterns.
Autosomal Recessive Disorders
-
Thalassemia
-
Sickle cell anemia
-
Cystic fibrosis
-
Phenylketonuria
Autosomal Dominant Disorders
-
Achondroplasia
-
Osteogenesis imperfecta
X-Linked Disorders
-
Hemophilia
-
Duchenne muscular dystrophy
Detected by:
-
PCR-based tests
-
DNA mutation analysis
-
Next-generation sequencing
Congenital Structural Anomalies
These involve abnormal development of organs or body structures.
-
Neural tube defects (spina bifida, anencephaly)
-
Congenital heart diseases
-
Cleft lip and palate
-
Skeletal dysplasias
-
Renal malformations
Detected by:
-
Ultrasonography
-
Fetal anomaly scan
-
Maternal serum markers
Inherited Metabolic Disorders
These result from enzyme deficiencies affecting metabolism.
-
Maple syrup urine disease
-
Galactosemia
-
Tay-Sachs disease
-
Urea cycle disorders
Detected by:
-
Enzyme assays
-
Molecular genetic testing
-
Targeted mutation analysis
Sex-Linked and Sex Determination Disorders
-
Disorders of sex development
-
X-linked genetic diseases (for carrier mothers)
Detected by:
-
Fetal karyotyping
-
Molecular sex determination
Methods of Prenatal Diagnosis
Prenatal diagnosis involves a variety of screening and diagnostic techniques used during pregnancy to detect genetic, chromosomal, and structural abnormalities in the fetus. These methods are broadly classified into non-invasive and invasive techniques.
A. Non-Invasive Prenatal Diagnostic Methods
These tests are safe and performed routinely during pregnancy.
Ultrasonography (USG)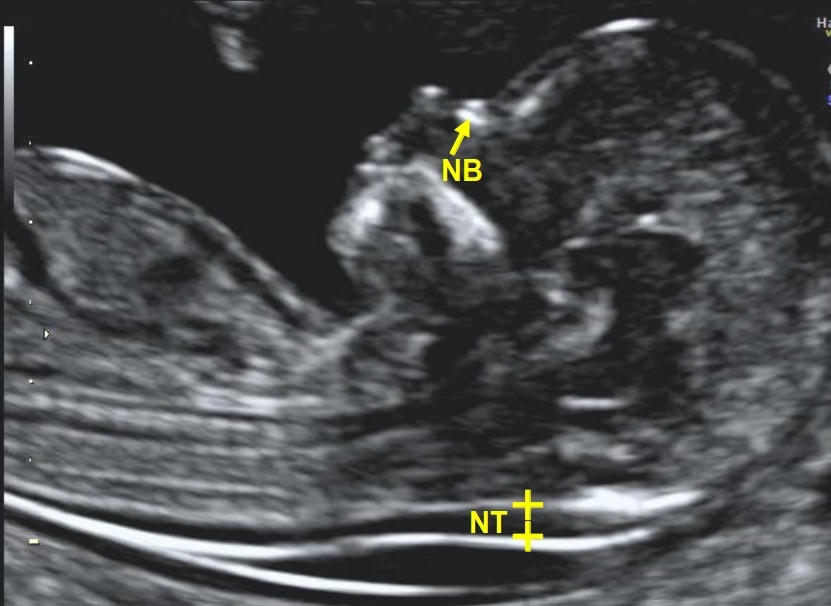
-
First-trimester dating scan
-
Nuchal translucency (NT) measurement
-
Detection of fetal structural anomalies
-
Assessment of fetal growth and development
Detects:
-
Neural tube defects
-
Congenital heart defects
-
Skeletal abnormalities
Maternal Serum Screening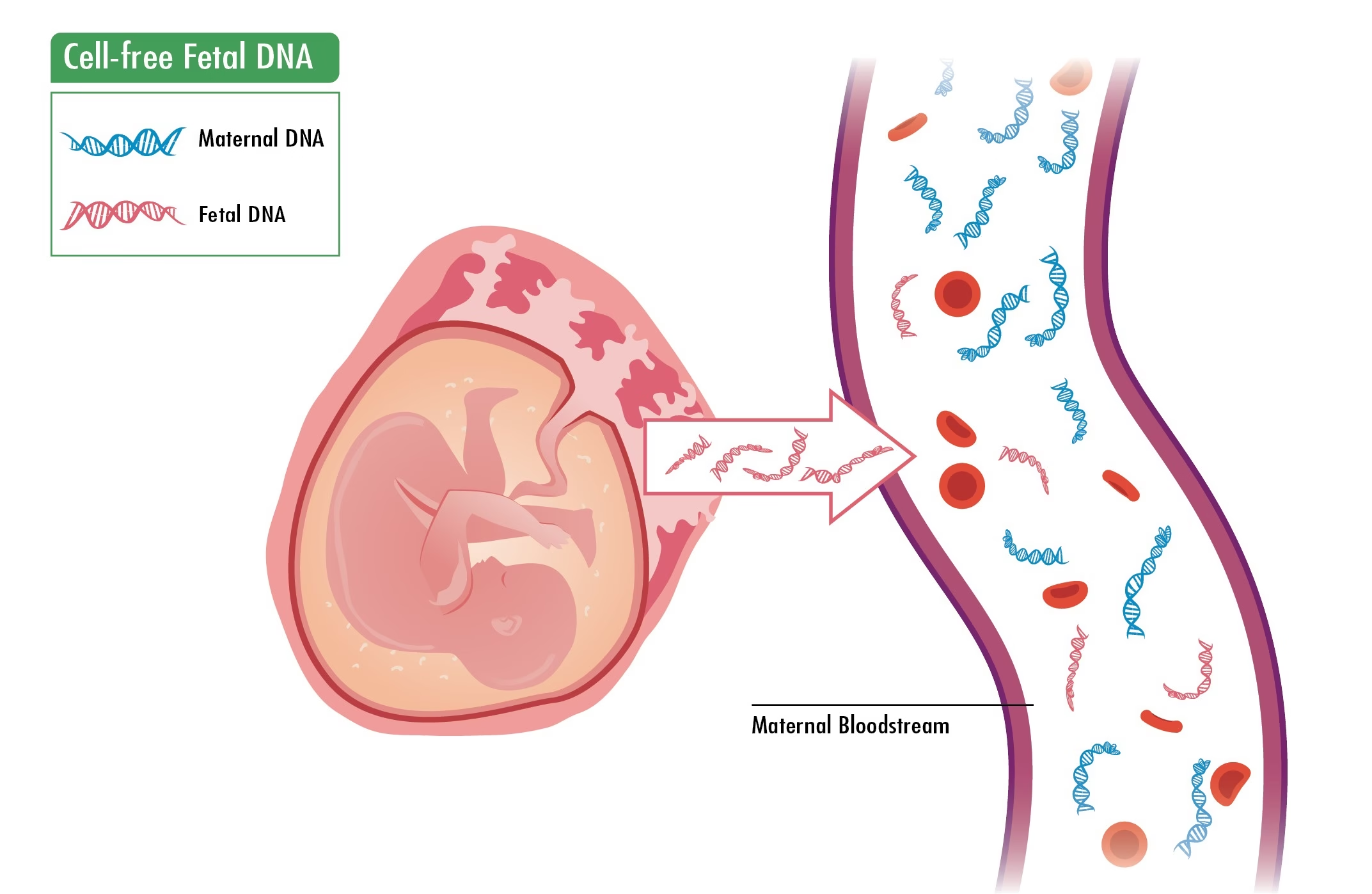
Biochemical markers measured in maternal blood.
-
Double test (β-hCG, PAPP-A)
-
Triple test (AFP, β-hCG, unconjugated estriol)
-
Quadruple test (Triple test + inhibin A)
Used for screening:
-
Down syndrome
-
Trisomy 18
-
Neural tube defects
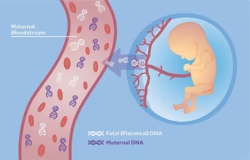
Non-Invasive Prenatal Testing (NIPT)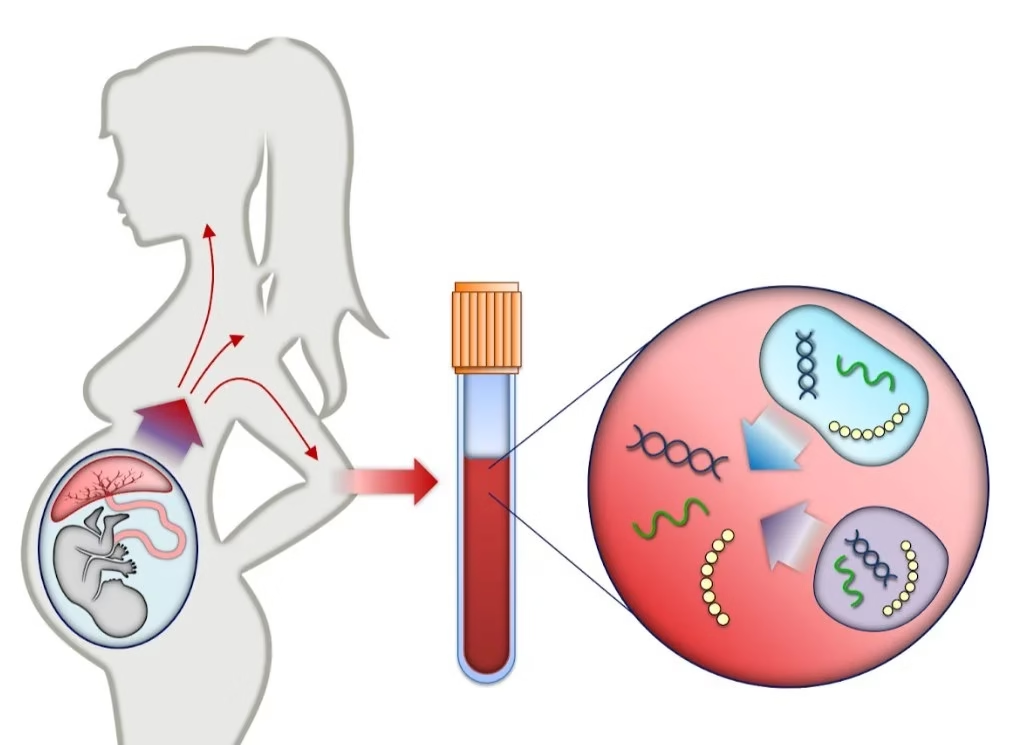
-
Based on cell-free fetal DNA in maternal blood
-
Can be done after 10 weeks of gestation
-
Very high sensitivity and specificity
Detects:
-
Trisomy 21, 18, 13
-
Sex chromosome abnormalities
B. Invasive Prenatal Diagnostic Methods
These tests provide definitive diagnosis.
Chorionic Villus Sampling (CVS)
-
Performed at 10–12 weeks
-
Placental tissue is sampled
-
Early diagnosis possible
Used for:
-
Chromosomal analysis
-
Single-gene disorders
-
DNA mutation testing
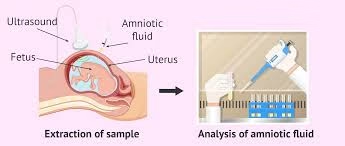
Amniocentesis
-
Performed at 15–20 weeks
-
Amniotic fluid containing fetal cells is analyzed
Gold standard for:
-
Karyotyping
-
Neural tube defect detection
-
Inherited metabolic disorders
Cordocentesis
-
Fetal blood obtained from umbilical cord
-
Used when rapid diagnosis is needed
Used for:
-
Hematological disorders
-
Fetal infections
-
Rapid chromosomal analysis
C. Molecular and Cytogenetic Techniques Used
-
Karyotyping
-
Fluorescence in situ hybridization (FISH)
-
Polymerase chain reaction (PCR)
-
Chromosomal microarray
-
Next-generation sequencing (NGS)
Laboratory Techniques
Karyotyping
-
Microscopic analysis of fetal chromosomes
-
Detects numerical and structural chromosomal abnormalities
-
Requires cultured fetal cells
Detects:
-
Trisomy 21, 18, 13
-
Turner syndrome
-
Translocations and deletions
Sample:
-
Amniotic fluid
-
Chorionic villi
-
Fetal blood
Fluorescence In Situ Hybridization (FISH)
-
Uses fluorescent DNA probes targeting specific chromosomes
-
Provides rapid results (24–48 hours)
Detects:
-
Common aneuploidies
-
Microdeletions
-
Sex chromosome abnormalities
Advantage: Faster than karyotyping
Limitation: Cannot detect all chromosomal changes
Polymerase Chain Reaction (PCR)
-
Amplifies specific DNA sequences
-
Highly sensitive and specific
Used for:
-
Single-gene disorders
-
Point mutations
-
Carrier detection
Detects:
-
Thalassemia
-
Sickle cell anemia
-
Cystic fibrosis
Chromosomal Microarray Analysis (CMA)
-
High-resolution technique analyzing copy number variations (CNVs)
-
Does not require cell culture
Detects:
-
Submicroscopic deletions and duplications
-
Unexplained developmental anomalies
Advantage: Higher resolution than karyotyping
Limitation: Cannot detect balanced translocations
Next-Generation Sequencing (NGS)
-
Massively parallel DNA sequencing
-
Allows whole-exome or targeted gene analysis
Used for:
-
Rare genetic disorders
-
Multiple gene mutations
-
Complex syndromes
Advantage: Comprehensive genetic analysis
Limitation: High cost and complex interpretation
Biochemical and Enzyme Assays
-
Measure enzyme activity or metabolite levels
-
Useful in diagnosing inherited metabolic disorders
Detects:
-
Phenylketonuria
-
Galactosemia
-
Urea cycle defects
MCQs
1. Prenatal diagnosis is mainly performed to detect:
A. Maternal infections
B. Genetic and chromosomal disorders
C. Postnatal diseases
D. Nutritional deficiencies
Answer: B
2. The safest prenatal diagnostic technique is:
A. Amniocentesis
B. CVS
C. Cordocentesis
D. Ultrasonography
Answer: D
3. Nuchal translucency measurement is done during:
A. Second trimester
B. Third trimester
C. First trimester
D. Postnatal period
Answer: C
4. Down syndrome is caused by:
A. Trisomy 18
B. Trisomy 21
C. Trisomy 13
D. Monosomy X
Answer: B
5. The most common chromosomal abnormality detected prenatally is:
A. Turner syndrome
B. Klinefelter syndrome
C. Down syndrome
D. Edwards syndrome
Answer: C
6. Which test detects cell-free fetal DNA?
A. Triple test
B. Amniocentesis
C. NIPT
D. CVS
Answer: C
7. NIPT can be performed after:
A. 6 weeks
B. 8 weeks
C. 10 weeks
D. 20 weeks
Answer: C
8. Chorionic villus sampling is usually done at:
A. 6–8 weeks
B. 10–12 weeks
C. 15–18 weeks
D. After 20 weeks
Answer: B
9. Sample used in amniocentesis is:
A. Placental tissue
B. Fetal blood
C. Amniotic fluid
D. Maternal serum
Answer: C
10. Gold standard test for fetal karyotyping is:
A. Ultrasonography
B. Amniocentesis
C. NIPT
D. Double marker test
Answer: B
11. Cordocentesis is also known as:
A. CVS
B. PUBS
C. Amniocentesis
D. FISH
Answer: B
12. Triple test includes all EXCEPT:
A. AFP
B. hCG
C. Unconjugated estriol
D. Inhibin A
Answer: D
13. Quadruple test includes:
A. AFP, hCG, Estriol
B. AFP, hCG, Estriol, Inhibin A
C. AFP only
D. hCG only
Answer: B
14. Neural tube defects are best detected by:
A. FISH
B. Ultrasonography
C. PCR
D. NIPT
Answer: B
15. Which marker is increased in neural tube defects?
A. hCG
B. Estriol
C. AFP
D. Inhibin A
Answer: C
16. Turner syndrome karyotype is:
A. 47,XXY
B. 46,XX
C. 45,X
D. 47,XXX
Answer: C
17. Klinefelter syndrome is:
A. 45,X
B. 46,XY
C. 47,XXY
D. 47,XYY
Answer: C
18. Which technique detects microdeletions?
A. Karyotyping
B. PCR
C. Chromosomal microarray
D. Ultrasonography
Answer: C
19. FISH is mainly used for:
A. Whole genome sequencing
B. Rapid aneuploidy detection
C. Enzyme estimation
D. Protein analysis
Answer: B
20. PCR is mainly useful for detecting:
A. Structural anomalies
B. Enzyme activity
C. Single-gene disorders
D. Gross chromosomal changes
Answer: C
21. Thalassemia is diagnosed prenatally by:
A. Ultrasonography
B. PCR
C. AFP estimation
D. NT scan
Answer: B
22. Inherited metabolic disorders are detected by:
A. Enzyme assays
B. Ultrasonography
C. NT scan
D. Triple test
Answer: A
23. Which test carries the highest fetal risk?
A. Ultrasonography
B. NIPT
C. Amniocentesis
D. Cordocentesis
Answer: D
24. CVS sample is obtained from:
A. Amniotic fluid
B. Placenta
C. Umbilical cord
D. Maternal blood
Answer: B
25. A screening test gives:
A. Definitive diagnosis
B. Risk estimation
C. Treatment plan
D. Cure
Answer: B
26. Definitive diagnosis is provided by:
A. Screening tests
B. Invasive diagnostic tests
C. Ultrasonography only
D. Serum markers
Answer: B
27. Advanced maternal age is defined as:
A. >25 years
B. >30 years
C. >35 years
D. >40 years
Answer: C
28. Which disorder is X-linked?
A. Thalassemia
B. Cystic fibrosis
C. Hemophilia
D. Down syndrome
Answer: C
29. Duchenne muscular dystrophy is:
A. Autosomal recessive
B. Autosomal dominant
C. X-linked recessive
D. Mitochondrial
Answer: C
30. Balanced translocations are best detected by:
A. CMA
B. PCR
C. Karyotyping
D. NGS
Answer: C
31. NIPT is:
A. Diagnostic
B. Invasive
C. Screening
D. Therapeutic
Answer: C
32. First-trimester screening includes:
A. Triple test
B. NT scan + Double test
C. Quadruple test
D. AFP only
Answer: B
33. Amniocentesis is contraindicated before:
A. 8 weeks
B. 10 weeks
C. 14 weeks
D. 20 weeks
Answer: C
34. Which disorder results from enzyme deficiency?
A. Down syndrome
B. PKU
C. Turner syndrome
D. Edwards syndrome
Answer: B
35. Galactosemia is diagnosed by:
A. Karyotyping
B. Enzyme assay
C. NT scan
D. AFP
Answer: B
36. Most accurate test for chromosomal aneuploidy:
A. Double test
B. NIPT
C. NT scan
D. AFP
Answer: B
37. Main limitation of NIPT:
A. High cost
B. Risk of miscarriage
C. Poor sensitivity
D. Invasive
Answer: A
38. Ethical issue in prenatal diagnosis includes:
A. Sample collection
B. Genetic counseling
C. Pregnancy termination
D. Test accuracy
Answer: C
39. Genetic counseling is important to:
A. Perform tests
B. Interpret risks
C. Treat fetus
D. Replace diagnosis
Answer: B
40. Which test detects fetal anemia?
A. Amniocentesis
B. Cordocentesis
C. NIPT
D. NT scan
Answer: B
41. AFP is produced by:
A. Placenta
B. Maternal liver
C. Fetal liver
D. Amniotic sac
Answer: C
42. CMA cannot detect:
A. Microdeletions
B. Copy number variations
C. Balanced translocations
D. Duplications
Answer: C
43. NIPT sample is:
A. Amniotic fluid
B. Placental tissue
C. Maternal blood
D. Fetal blood
Answer: C
44. FISH uses:
A. Enzymes
B. Fluorescent probes
C. Antibodies
D. Proteins
Answer: B
45. Neural tube defects occur due to deficiency of:
A. Vitamin B12
B. Vitamin D
C. Folic acid
D. Vitamin C
Answer: C
46. Turner syndrome patients are:
A. Male
B. Female
C. Hermaphrodite
D. Intersex
Answer: B
47. Most common indication for prenatal diagnosis:
A. Infection
B. Family history
C. Advanced maternal age
D. Malnutrition
Answer: C
48. NIPT cannot detect:
A. Trisomy 21
B. Trisomy 18
C. Structural malformations
D. Sex chromosome abnormalities
Answer: C
49. Prenatal diagnosis helps in:
A. Treatment only
B. Risk prediction only
C. Informed decision-making
D. Preventing pregnancy
Answer: C
50. Ultimate goal of prenatal diagnosis is:
A. Detect disease
B. Reduce fetal mortality
C. Improve maternal care
D. All of the above
Answer: D