Introduction
Blastomyces is a genus of dimorphic fungi that causes blastomycosis, a systemic fungal infection. The primary species causing human disease include:
-
- Blastomyces dermatitidis
- Blastomyces gilchristii
- Blastomyces helicus (less common, associated with CNS infections in immunosuppressed individuals).
Key Characteristics:
-
- Found in soil and decaying organic material.
- Endemic in specific regions, particularly in North America.
- Thermally dimorphic:
- Mold (mycelial) form: Produces infectious conidia (spores) in the environment at 22–25°C.
- Yeast form: Seen in host tissues at 37°C, growing as large, thick-walled, broad-based budding yeasts.
Clinical Relevance: Blastomycosis can range from self-limited pulmonary disease to disseminated systemic infections affecting multiple organs.
Epidemiology
- Geographic Distribution:
-
- Primarily in North America:
- Endemic in the Ohio River Valley, Mississippi River Valley, the Great Lakes region, and parts of southeastern Canada.
- Isolated cases have been reported in Africa, Central America, and India.
- Primarily in North America:
-
- Reservoir:
-
- Found in moist, acidic soils enriched with decaying organic material such as:
- Forests
- Riverbanks
- Marshlands
- Commonly associated with areas disturbed by human or animal activity.
- Found in moist, acidic soils enriched with decaying organic material such as:
-
- Transmission:
-
- Occurs via inhalation of airborne conidia (spores).
- No person-to-person transmission has been documented.
- Rarely, direct inoculation into the skin can cause localized infection.
-
- At-risk populations:
-
- Individuals participating in outdoor activities such as:
- Hunting, fishing, forestry work, camping, and construction.
- Immunosuppressed individuals (e.g., HIV/AIDS, organ transplant recipients, or those on immunosuppressive therapy) are at higher risk for severe and disseminated disease.
- Individuals participating in outdoor activities such as:
-
- Incidence:
-
- Blastomycosis is less common than other endemic fungal infections, such as histoplasmosis or coccidioidomycosis.
- Annual incidence in endemic regions is approximately 1–2 cases per 100,000 individuals.
-
Pathogenesis
The pathogenesis of Blastomyces involves a complex interplay between fungal virulence factors and host immune responses:
- Inhalation and Transition:
-
- Inhaled conidia (spores) enter the respiratory tract.
- At body temperature, conidia convert to yeast in the lungs.
-
- Adhesion and Immune Evasion:
-
- BAD1 (Blastomyces adhesin 1):
- A key virulence factor.
- Promotes adhesion to host epithelial cells and macrophages.
- Suppresses TNF-α and pro-inflammatory cytokine production, which weakens the immune response.
- BAD1 (Blastomyces adhesin 1):
-
- Host Immune Response:
-
- The host relies primarily on cell-mediated immunity to control infection:
- Th1 response produces cytokines like IFN-γ, which activate macrophages to kill yeast cells.
- In immunocompromised hosts, fungal replication and dissemination are unchecked.
- The host relies primarily on cell-mediated immunity to control infection:
-
- Granuloma Formation:
-
- The host mounts a granulomatous inflammatory response to contain the infection in immunocompetent individuals.
- Granulomas are composed of macrophages, lymphocytes, and multinucleated giant cells.
-
- Dissemination:
-
- Yeast cells can spread via the bloodstream or lymphatics to extrapulmonary sites:
- Commonly, skin, bones, genitourinary system, and CNS.
- Yeast cells can spread via the bloodstream or lymphatics to extrapulmonary sites:
-
Clinical Manifestations
Blastomycosis has a wide spectrum of clinical presentations, ranging from asymptomatic to life-threatening disease.
- Pulmonary Blastomycosis
-
- Asymptomatic: ~50% of infections may be subclinical or mild.
- Acute pulmonary disease:
- Flu-like symptoms: Fever, chills, cough, fatigue, myalgia.
- It can mimic bacterial or viral pneumonia.
- Chronic pulmonary disease:
- Progressive symptoms resembling tuberculosis or lung cancer:
- Weight loss
- Night sweats
- Persistent cough
- Hemoptysis
- Progressive symptoms resembling tuberculosis or lung cancer:
- Disseminated Blastomycosis
-
- Occurs in ~25–50% of symptomatic cases.
- Common sites of dissemination:
- Skin:
- Verrucous plaques, nodules, or ulcers.
- Resemble squamous cell carcinoma or pyoderma gangrenosum.
- Bones:
- Pain, swelling, or pathological fractures due to osteomyelitis.
- CNS:
- Meningitis, brain abscesses (rare but serious).
- Genitourinary system:
- Prostatitis, epididymitis, or testicular masses.
- Skin:
- Cutaneous Blastomycosis
-
- It may occur via direct inoculation or dissemination.
- Characterized by painless, verrucous, or ulcerated lesions.
- Immunocompromised Hosts
-
- More severe disease, often with widespread dissemination.
- Higher risk of respiratory failure or CNS involvement.
Laboratory Diagnosis
-
- The diagnosis of blastomycosis requires a combination of clinical suspicion and laboratory methods:
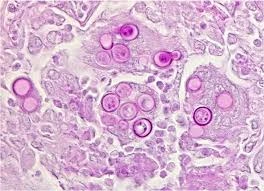
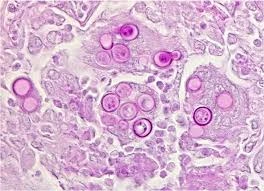
- Microscopy:
-
- KOH preparation of sputum, BAL fluid, or tissue biopsies:
- Reveals thick-walled, broad-based budding yeast cells.
- Stains:
- Periodic acid–Schiff (PAS)
- Gomori methenamine silver (GMS)
- KOH preparation of sputum, BAL fluid, or tissue biopsies:
- Culture:
-
- The gold standard for diagnosis.
- Specimen: Sputum, BAL, tissue biopsies, or pus.
- Grows on fungal media (e.g., Sabouraud agar).
- Morphology:
- 22–25°C: Mold phase with conidia.
- 37°C: Yeast phase with broad-based buds.
- Growth time: 1–4 weeks.
- Histopathology:
-
- Biopsy of infected tissue shows granulomatous inflammation with yeast forms.
- Antigen Testing:
-
- Blastomyces antigen detected in urine, serum, or BAL fluid.
- Useful for rapid diagnosis but may cross-react with Histoplasma.
- Molecular Diagnostics:
-
- PCR-based assays provide rapid and specific identification.
- Serology:
-
- Antibody detection has limited sensitivity and specificity, often used as a supplementary test.