Introduction
-
Blood transfusion and plasma exchange are life-saving medical procedures that involve the transfer of blood or blood components from a donor to a recipient.
-
It is widely used in the management of anemia, massive blood loss, hematological disorders, malignancies, coagulation abnormalities, and critical care conditions.
-
With advancements in transfusion medicine, there has been a shift from whole blood transfusion to component therapy.
-
Component therapy allows targeted replacement of deficient blood components, improving efficacy and reducing complications.

-
Modern transfusion practice also includes the use of transfusion filters to prevent infusion of clots and cellular debris.
-
Post-transfusion monitoring is essential for early detection and management of transfusion reactions.
-
Advanced procedures such as therapeutic plasma exchange (TPE) have expanded the role of transfusion medicine in immune-mediated and metabolic disorders.
-
Proper knowledge of transfusion techniques, safety measures, and post-procedure care is vital to ensure patient safety, improve clinical outcomes, and minimize transfusion-related risks.
Blood Transfusion
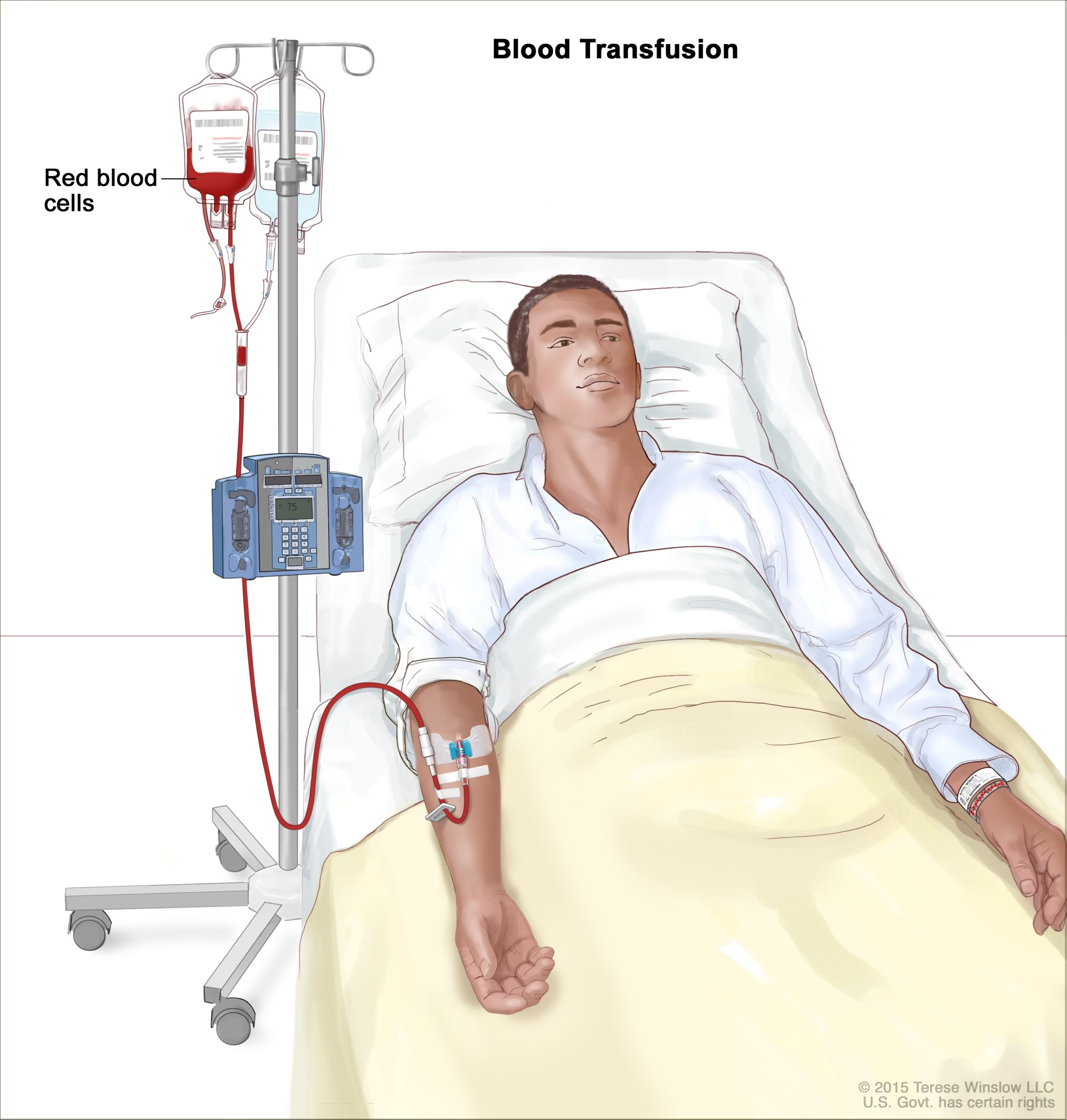
Blood transfusion is the intravenous administration of whole blood or specific blood components such as red blood cells (RBCs), platelets, plasma, or cryoprecipitate to a patient for therapeutic purposes.
Indications of Blood Transfusion
Blood transfusion is indicated in the following conditions:
-
Acute blood loss (trauma, surgery, obstetric hemorrhage)
-
Severe anemia (Hb <7 g/dL or symptomatic anemia)
-
Hematological disorders (thalassemia, aplastic anemia)
-
Bleeding disorders and coagulopathies
-
Thrombocytopenia with active bleeding
-
Burns and shock
-
Liver disease with coagulation factor deficiency
Types of Blood Transfusion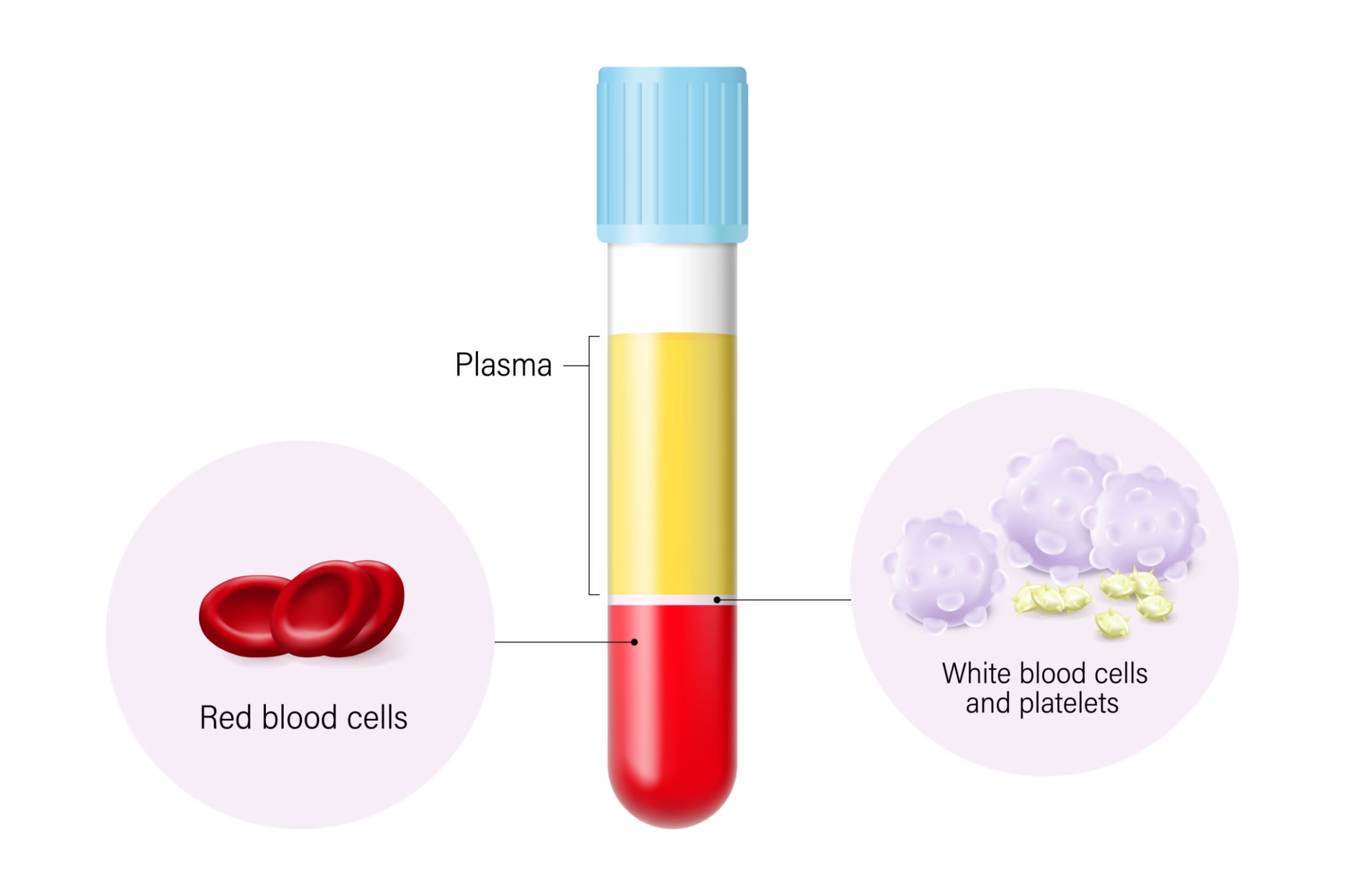
a) Whole Blood Transfusion
-
Contains RBCs, plasma, platelets, and clotting factors
-
Rarely used today
-
Indicated in massive acute blood loss where component separation is unavailable
b) Component Therapy (Preferred Method)
| Component | Indication |
|---|---|
| Packed Red Blood Cells (PRBCs) | Anemia, blood loss |
| Platelet Concentrates | Thrombocytopenia |
| Fresh Frozen Plasma (FFP) | Coagulation factor deficiency |
| Cryoprecipitate | Hemophilia A, hypofibrinogenemia |
Pre-Transfusion Compatibility Testing
Before transfusion, the following tests are mandatory:
-
ABO blood grouping
-
Rh typing
-
Antibody screening
-
Cross-matching
-
Infectious disease screening (HIV, HBV, HCV, Syphilis, Malaria)
Risks and Complications of Blood Transfusion
-
Acute hemolytic transfusion reaction
-
Febrile non-hemolytic reaction
-
Allergic reactions
-
Transfusion-related acute lung injury (TRALI)
-
Transfusion-associated circulatory overload (TACO)
-
Transmission of infections
-
Iron overload (chronic transfusion)
Transfusion Filters
A transfusion filter is a device incorporated into the blood transfusion set that removes clots, cellular debris, fibrin strands, and aggregates from blood or blood components before they enter the patient’s circulation.
Purpose of Transfusion Filters
-
Prevent microembolism
-
Reduce febrile transfusion reactions
-
Prevent infusion of clots and debris
-
Improve patient safety
Types of Transfusion Filters
a) Standard Blood Filters (170–260 µm)
-
Used routinely for whole blood and PRBC transfusion
-
Removes macroaggregates and clots
b) Microaggregate Filters (20–40 µm)
-
Used in massive transfusion
-
Removes platelet-leukocyte aggregates
c) Leukocyte Reduction Filters
-
Removes leukocytes
-
Reduces febrile reactions, CMV transmission, and HLA alloimmunization
d) Specialized Filters
-
Platelet-specific filters
-
Pediatric transfusion filters
Guidelines for Using Transfusion Filters
-
One filter per blood unit
-
Do not flush with dextrose or calcium-containing solutions
-
Maintain aseptic technique
-
Replace clogged filters immediately
Post-Transfusion Care
Importance of Post-Transfusion Monitoring
Post-transfusion care is critical for early detection of adverse reactions and ensuring therapeutic efficacy. Many transfusion reactions occur within the first few hours after transfusion.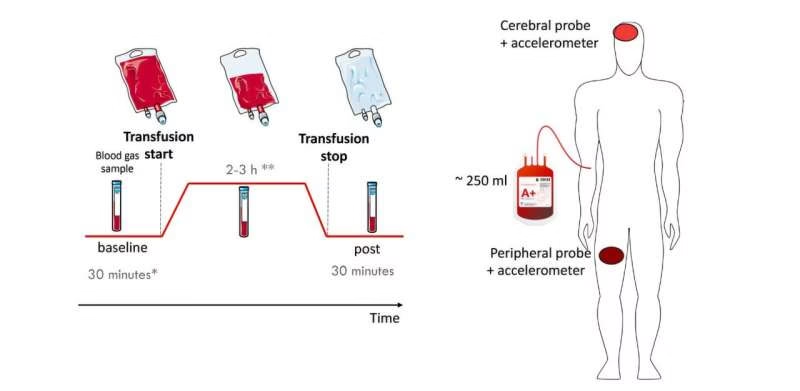
Immediate Post-Transfusion Care
-
Monitor vital signs (pulse, BP, temperature, respiration)
-
Observe patient for:
-
Fever
-
Chills
-
Rash or itching
-
Dyspnea
-
Chest or back pain
-
-
Maintain IV access
-
Document transfusion details
Delayed Post-Transfusion Monitoring
Delayed reactions may occur days to weeks later:
-
Delayed hemolytic reaction
-
Post-transfusion purpura
-
Transfusion-associated graft-versus-host disease
-
Iron overload
Patients receiving chronic transfusions require:
-
Serum ferritin monitoring
-
Liver and cardiac evaluation
-
Iron chelation therapy if needed
Management of Transfusion Reactions
If any reaction is suspected:
-
Stop transfusion immediately
-
Maintain IV line with normal saline
-
Inform blood bank and physician
-
Send blood bag and patient samples for investigation
-
Provide symptomatic treatment
Therapeutic Plasma Exchange
Therapeutic plasma exchange is an extracorporeal procedure in which plasma containing pathogenic substances is removed from the patient’s blood and replaced with donor plasma or replacement fluids.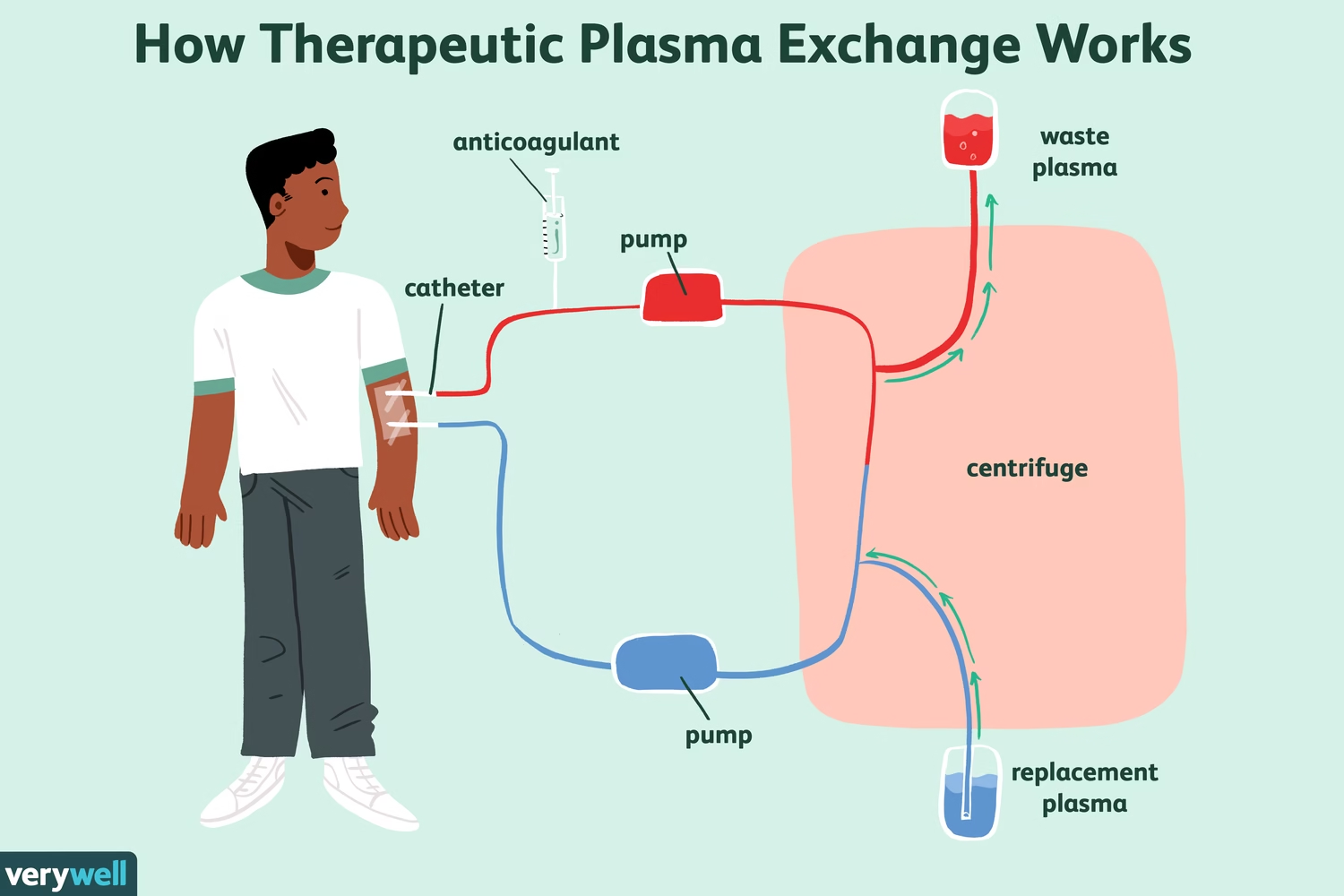
Principle of Therapeutic Plasma Exchange
-
Blood is withdrawn from the patient
-
Plasma is separated from cellular components
-
Plasma containing autoantibodies, immune complexes, or toxins is discarded
-
Cellular components are returned with replacement fluid
Indications of Therapeutic Plasma Exchange
Neurological Disorders
-
Guillain-Barré syndrome
-
Myasthenia gravis
-
Chronic inflammatory demyelinating polyneuropathy
Hematological Disorders
-
Thrombotic thrombocytopenic purpura (TTP)
-
Hyperviscosity syndrome
-
Cryoglobulinemia
Renal and Autoimmune Diseases
-
Rapidly progressive glomerulonephritis
-
Lupus nephritis
-
Goodpasture syndrome
Metabolic and Toxic Conditions
-
Familial hypercholesterolemia
-
Certain drug or toxin removal
Replacement Fluids Used
-
Fresh frozen plasma
-
Albumin solution
-
Normal saline (limited use)
Choice depends on disease indication and coagulation status.
Complications of Therapeutic Plasma Exchange
-
Hypotension
-
Electrolyte imbalance
-
Bleeding due to coagulation factor loss
-
Allergic reactions
-
Infection risk due to central venous access
Advantages of Therapeutic Plasma Exchange
-
Rapid removal of pathogenic substances
-
Life-saving in acute immune-mediated disorders
-
Improves response to immunosuppressive therapy
Role of Laboratory and Blood Bank Services
Laboratory services are central to safe transfusion practices:
-
Donor screening and selection
-
Component preparation and storage
-
Compatibility testing
-
Transfusion reaction investigation
-
Quality control and hemovigilance
Strict adherence to transfusion protocols significantly reduces morbidity and mortality.
MCQs
1. Blood transfusion is defined as:
A. Oral administration of blood
B. Transfer of blood from patient to donor
C. Transfer of blood or blood components from donor to recipient
D. Exchange of plasma only
✅ Answer: C
2. The most commonly used form of transfusion today is:
A. Whole blood
B. Plasma only
C. Component therapy
D. Autologous transfusion
✅ Answer: C
3. Packed red blood cells (PRBCs) are mainly indicated for:
A. Coagulation disorders
B. Thrombocytopenia
C. Anemia
D. Hypoproteinemia
✅ Answer: C
4. Fresh frozen plasma is used primarily to treat:
A. Anemia
B. Platelet deficiency
C. Coagulation factor deficiency
D. Iron overload
✅ Answer: C
5. Which blood component is rich in fibrinogen?
A. PRBCs
B. Platelets
C. Cryoprecipitate
D. Whole blood
✅ Answer: C
6. The minimum hemoglobin level commonly considered for transfusion in stable patients is:
A. 10 g/dL
B. 9 g/dL
C. 7 g/dL
D. 12 g/dL
✅ Answer: C
7. Cross-matching is done to detect:
A. Blood group
B. Rh factor
C. Antibody-antigen incompatibility
D. Platelet count
✅ Answer: C
8. Which infection is mandatorily screened before blood transfusion?
A. Tuberculosis
B. HIV
C. Dengue
D. Typhoid
✅ Answer: B
9. Acute hemolytic transfusion reaction is most commonly due to:
A. Platelet incompatibility
B. ABO incompatibility
C. Leukocyte reaction
D. Volume overload
✅ Answer: B
10. The safest route for blood transfusion is:
A. Intramuscular
B. Subcutaneous
C. Intravenous
D. Intra-arterial
✅ Answer: C
Transfusion Filters – MCQs
11. The main function of a transfusion filter is to remove:
A. Viruses
B. Bacteria
C. Clots and debris
D. Plasma proteins
✅ Answer: C
12. The pore size of a standard blood transfusion filter is:
A. 5–10 µm
B. 20–40 µm
C. 170–260 µm
D. 500 µm
✅ Answer: C
13. Microaggregate filters are mainly used during:
A. Platelet transfusion
B. Massive transfusion
C. Plasma exchange
D. Pediatric transfusion
✅ Answer: B
14. Leukocyte reduction filters help reduce:
A. Hemolysis
B. Iron overload
C. Febrile reactions
D. Bleeding risk
✅ Answer: C
15. One transfusion filter should be used for:
A. Multiple patients
B. One blood unit
C. One hospital shift
D. One donor
✅ Answer: B
16. Which solution should NOT be used to flush transfusion filters?
A. Normal saline
B. Dextrose
C. Sterile saline
D. Isotonic saline
✅ Answer: B
17. Transfusion filters are mandatory for transfusion of:
A. Oral iron
B. Blood components
C. IV fluids
D. Medications
✅ Answer: B
Post-Transfusion Care – MCQs
18. The most critical period for transfusion reactions is:
A. After 24 hours
B. First 15–30 minutes
C. After 7 days
D. After 1 month
✅ Answer: B
19. Which vital sign must be monitored during transfusion?
A. Pulse
B. Blood pressure
C. Temperature
D. All of the above
✅ Answer: D
20. The first step when a transfusion reaction is suspected is to:
A. Give antihistamines
B. Slow the transfusion
C. Stop the transfusion
D. Change IV line
✅ Answer: C
21. Febrile non-hemolytic transfusion reaction is commonly due to:
A. RBC destruction
B. Leukocyte cytokines
C. Plasma proteins
D. Platelet deficiency
✅ Answer: B
22. Which is a delayed transfusion reaction?
A. Anaphylaxis
B. TRALI
C. Delayed hemolytic reaction
D. Hypotension
✅ Answer: C
23. Iron overload is seen mainly in:
A. Single transfusion
B. Plasma transfusion
C. Chronic transfusion patients
D. Platelet transfusion
✅ Answer: C
24. Transfusion-associated circulatory overload (TACO) occurs due to:
A. Infection
B. Excess volume
C. Hemolysis
D. Allergy
✅ Answer: B
25. After stopping transfusion due to reaction, IV line should be kept open with:
A. Dextrose
B. Ringer lactate
C. Normal saline
D. Blood
✅ Answer: C
Therapeutic Plasma Exchange (TPE) – MCQs
26. Therapeutic plasma exchange involves removal of:
A. RBCs only
B. Platelets only
C. Plasma
D. Whole blood
✅ Answer: C
27. TPE is also known as:
A. Hemodialysis
B. Plasmapheresis
C. Hemofiltration
D. Ultrafiltration
✅ Answer: B
28. The main purpose of TPE is to remove:
A. Electrolytes
B. Pathogenic antibodies
C. Oxygen
D. Red cells
✅ Answer: B
29. TPE is the treatment of choice for:
A. Iron deficiency anemia
B. Thrombotic thrombocytopenic purpura
C. Hemophilia
D. Leukemia
✅ Answer: B
30. Guillain-Barré syndrome is treated by:
A. Whole blood transfusion
B. Platelet transfusion
C. Therapeutic plasma exchange
D. Cryoprecipitate
✅ Answer: C
31. Replacement fluid commonly used in TPE is:
A. Whole blood
B. Packed RBCs
C. Albumin
D. Platelets
✅ Answer: C
32. Which condition is NOT an indication for TPE?
A. Myasthenia gravis
B. TTP
C. Iron deficiency anemia
D. Hyperviscosity syndrome
✅ Answer: C
33. A common complication of TPE is:
A. Hypertension
B. Hypotension
C. Polycythemia
D. Hyperglycemia
✅ Answer: B
34. Loss of coagulation factors during TPE may cause:
A. Thrombosis
B. Bleeding
C. Infection
D. Fever
✅ Answer: B
35. Central venous access is often required for:
A. Platelet transfusion
B. Plasma exchange
C. IM injection
D. Oral therapy
✅ Answer: B
Mixed / Applied MCQs
36. TRALI stands for:
A. Transfusion-Related Acute Lung Injury
B. Transfusion-Related Allergic Lung Infection
C. Transfusion-Related Arterial Lung Ischemia
D. Transfusion-Related Autoimmune Lung Injury
✅ Answer: A
37. Which blood component should be ABO compatible?
A. PRBCs
B. Platelets
C. Plasma
D. All of the above
✅ Answer: D
38. CMV transmission risk is reduced by:
A. Plasma exchange
B. Leukocyte-reduced blood
C. Whole blood
D. Iron chelation
✅ Answer: B
39. The best blood component for hypofibrinogenemia is:
A. PRBC
B. FFP
C. Cryoprecipitate
D. Platelets
✅ Answer: C
40. Post-transfusion purpura is due to:
A. Platelet antibodies
B. RBC antibodies
C. Plasma proteins
D. Iron toxicity
✅ Answer: A
41. The safest IV fluid compatible with blood transfusion is:
A. Dextrose
B. Ringer lactate
C. Normal saline
D. DNS
✅ Answer: C
42. Which reaction presents with fever and chills without hemolysis?
A. Allergic reaction
B. Febrile non-hemolytic reaction
C. Acute hemolytic reaction
D. TRALI
✅ Answer: B
43. The aim of component therapy is to:
A. Reduce blood usage
B. Target specific deficiency
C. Increase transfusion reactions
D. Delay treatment
✅ Answer: B
44. Therapeutic plasma exchange is most useful in:
A. Infectious diseases
B. Immune-mediated diseases
C. Nutritional anemia
D. Trauma
✅ Answer: B
45. Which blood component has the longest shelf life?
A. Platelets
B. PRBCs
C. Plasma (frozen)
D. Whole blood
✅ Answer: C
46. Platelets should be transfused using:
A. No filter
B. Standard blood filter
C. Microaggregate filter only
D. Dialysis filter
✅ Answer: B
47. Iron chelation therapy is required in:
A. Acute transfusion
B. Platelet transfusion
C. Chronic transfusion patients
D. Plasma exchange
✅ Answer: C
48. The primary goal of post-transfusion care is to:
A. Increase Hb rapidly
B. Detect adverse reactions early
C. Reduce blood cost
D. Improve storage
✅ Answer: B
49. Blood transfusion reactions should always be:
A. Ignored
B. Documented and reported
C. Treated at home
D. Delayed
✅ Answer: B
50. Therapeutic plasma exchange mainly removes substances present in:
A. RBCs
B. Platelets
C. Plasma
D. Bone marrow
✅ Answer: C